When Health Data Plays Nice Together (Finally!)
Why Health Data Interoperability Is Healthcare’s Most Critical Challenge
Health data interoperability enables different healthcare systems, devices, and applications to securely exchange and use patient information across organizational boundaries. Here’s what you need to know:
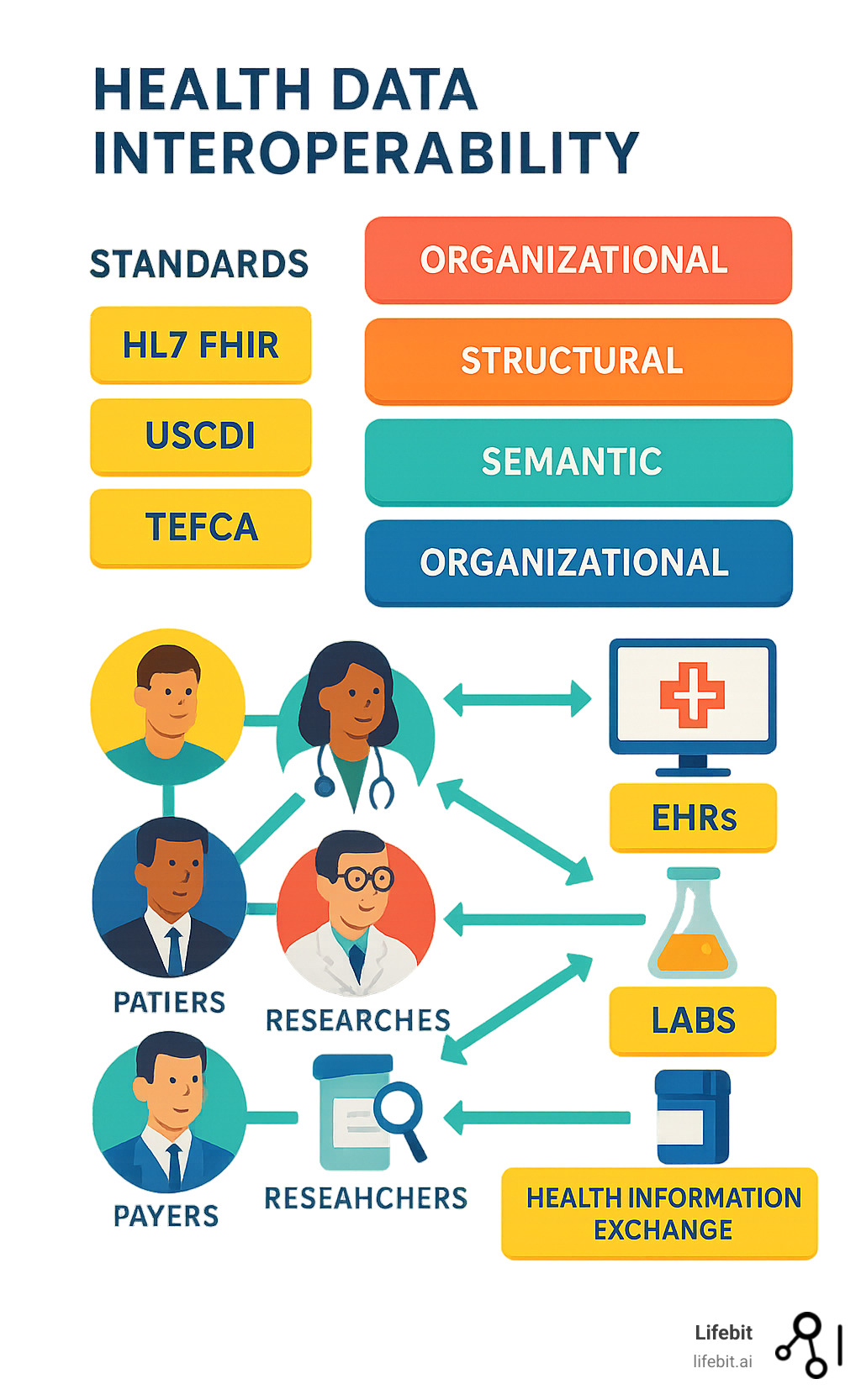
Key Components:
– Exchange: Moving data between systems (EHRs, labs, pharmacies)
– Integration: Combining data from multiple sources
– Interpretation: Understanding data meaning across platforms
– Standards: Common languages like HL7 FHIR and USCDI
Four Levels:
1. Foundational – Basic data transport
2. Structural – Standardized formats
3. Semantic – Shared meaning
4. Organizational – Governance and policies
Healthcare is sitting on a data goldmine that could save lives and billions of dollars. The average healthcare organization holds nearly 9 petabytes of medical data, yet most systems still can’t talk to each other effectively.
When you visit a new doctor, they often ask you to fill out the same forms again. Your previous test results might be sitting in another system just miles away, but your new provider can’t access them. This isn’t just inconvenient – it’s dangerous and expensive.
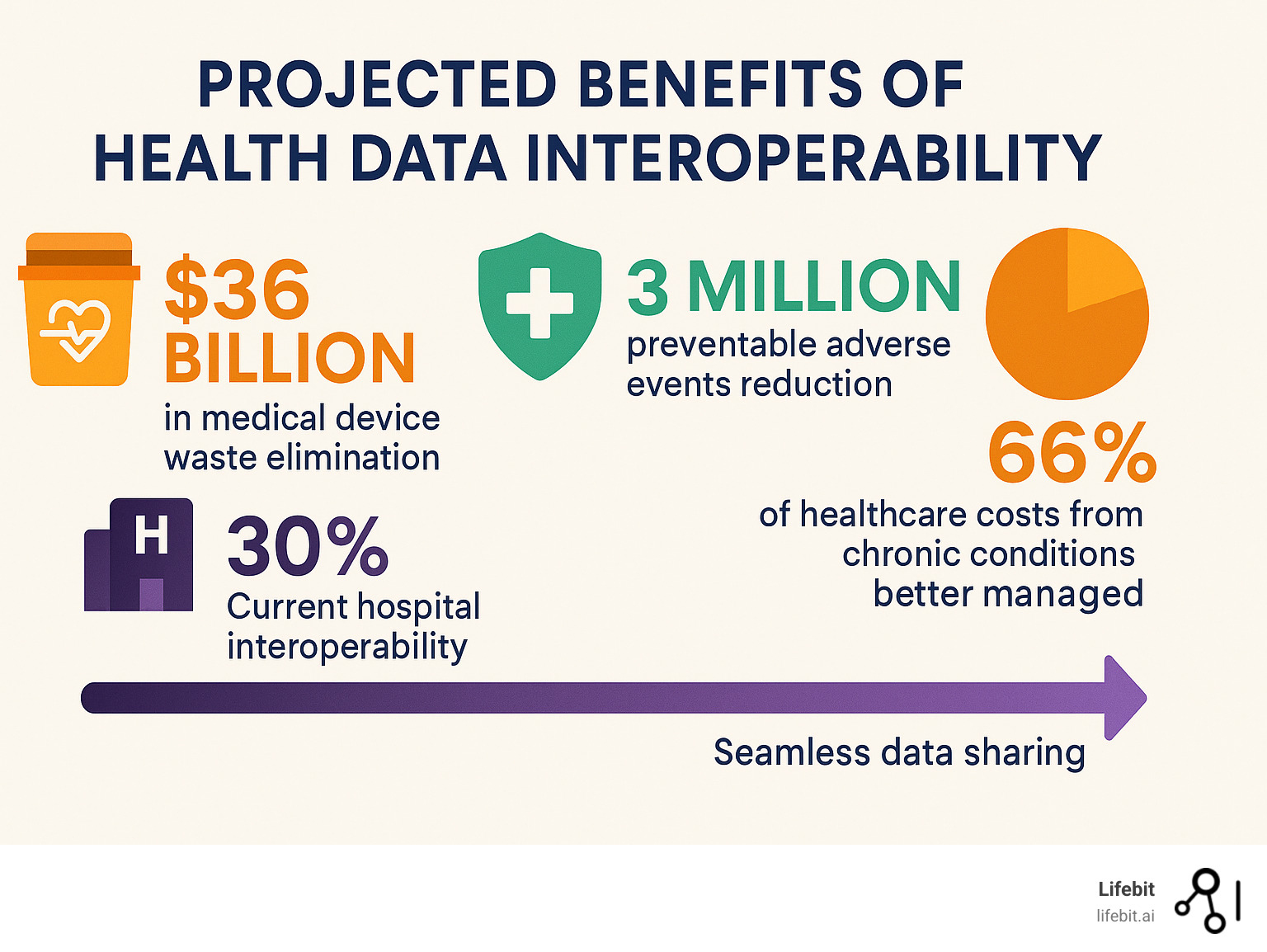
Medical errors result in as many as 3 million preventable adverse events each year in the US, leading to nearly 100,000 deaths and $17 billion in excess costs annually. Many of these errors happen because doctors don’t have complete patient information when they need it most.
The problem is massive but solvable. Countries like Canada are passing new laws (Bill C-72) to break down data silos. The US has the 21st Century Cures Act. Standards like FHIR are finally making real progress.
I’m Maria Chatzou Dunford, CEO of Lifebit, where we’ve spent years helping organizations break down health data interoperability barriers through federated analytics and secure data sharing.
What Is Health Data Interoperability?
Picture this: you’re traveling when you suddenly need emergency care. The ER doctor treating you has no idea about your diabetes medication, recent surgery, or penicillin allergy. This scenario happens thousands of times daily because healthcare systems can’t easily share information.
Health data interoperability changes that reality. It’s the ability for different healthcare systems, devices, and applications to exchange data and actually understand what that data means. HIMSS defines it as “the coordinated access, exchange, and use of data across systems and borders.”
Think of it like teaching all your devices to speak the same language. Your EHR at your family doctor’s office should communicate meaningfully with the hospital’s system, lab’s database, and pharmacy’s records. When these systems truly communicate, doctors get the complete picture they need to keep you safe and healthy.
Modern interoperability relies heavily on APIs (Application Programming Interfaces) that act like translators between different systems, ensuring data moves securely and maintains its meaning. These APIs enable real-time data exchange, allowing a cardiologist to instantly access your latest lab results from another facility while you’re sitting in their office.
The scope of health data interoperability extends far beyond simple data transfer. It encompasses everything from wearable device data streaming to your smartphone, to complex genomic information sharing between research institutions. Modern healthcare generates data from hundreds of sources: medical devices, laboratory instruments, imaging systems, patient-reported outcomes, social determinants of health, and even environmental factors that impact patient care.
Consider the complexity of a typical patient journey. Sarah visits her primary care physician for chest pain. The doctor orders an EKG, blood tests, and a chest X-ray. The EKG machine should automatically upload results to her EHR. Lab results from the hospital laboratory should appear in real-time. The radiology department’s imaging system should seamlessly share X-ray findings. If Sarah needs a cardiology referral, all this information should flow instantly to the specialist’s system, along with her complete medical history, current medications, and relevant family history.
Without proper interoperability, each step requires manual intervention: printing reports, faxing results, or asking Sarah to carry physical copies between providers. This manual process introduces delays, errors, and gaps in care that can have serious consequences.
Four Levels at a Glance – health data interoperability
Understanding health data interoperability means grasping its four building blocks, each representing increasing sophistication in how systems communicate:
Foundational interoperability is like having reliable mail service. Systems can send and receive data securely, but there’s no guarantee the receiving end will understand what it means. This level focuses purely on the technical ability to transmit information from point A to point B. Most healthcare organizations have achieved this basic level through secure messaging systems, encrypted email, or simple file transfers. However, foundational interoperability often requires significant manual processing on the receiving end to make sense of the incoming data.
Structural interoperability adds organization and standardization to the data format. Now we’re using agreed-upon formats and structures, like HL7 messages or standardized XML schemas. Systems can parse the structure even if they don’t fully grasp the content. This level ensures that when one system sends a lab result, the receiving system knows which field contains the test name, which contains the result value, and which contains the reference range. Structural interoperability eliminates much of the manual data entry that plagues foundational-level exchanges.
Semantic interoperability ensures systems actually understand what the data means. When one system sends “Type 2 diabetes mellitus,” another system knows exactly what condition this refers to, thanks to standardized vocabularies like SNOMED CT and LOINC. This level enables automated clinical decision support, population health analytics, and meaningful data aggregation across different organizations. Semantic interoperability is where the real clinical value emerges, as systems can automatically flag drug interactions, identify care gaps, or trigger clinical alerts based on incoming data.
Organizational interoperability brings in governance, policies, and legal frameworks. Organizations need agreements about when, how, and why they’ll share data, including patient consent and privacy protections. This level addresses the human and policy challenges that often prove more difficult than technical barriers. It includes establishing trust relationships between organizations, defining data use agreements, managing patient consent preferences, and ensuring compliance with regulations like HIPAA, GDPR, or local privacy laws.
| Level | Focus | Example | Key Challenge |
|---|---|---|---|
| Foundational | Data transport | Secure messaging between clinics | Ensuring reliable, secure transmission |
| Structural | Data format | HL7 messages with standard fields | Agreeing on common data structures |
| Semantic | Data meaning | SNOMED codes for consistent diagnoses | Standardizing medical vocabularies |
| Organizational | Governance | HIPAA-compliant sharing agreements | Aligning policies and legal frameworks |
Interoperability vs Integration – health data interoperability
Integration and interoperability work very differently in practice, and understanding this distinction is crucial for healthcare organizations planning their data strategy.
Integration is like building private roads between buildings you own. It connects specific systems within an organization or creates custom point-to-point connections. Every time you add a new system, you need another custom bridge. This creates “point-to-point spaghetti” – a tangled mess that’s expensive to maintain and nearly impossible to scale.
For example, a hospital might spend $200,000 integrating their EHR with their laboratory information system. When they add a new radiology system, they need another custom integration costing $150,000. Add a pharmacy system, and that’s another $100,000 integration project. Soon, they have dozens of custom connections, each requiring specialized maintenance and creating potential failure points.
Health data interoperability creates public highways that any authorized vehicle can use. Instead of custom connections, it relies on open standards and protocols that work across different vendors, organizations, and countries. When a hospital adopts FHIR-based interoperability, new systems can connect using the same standard protocols, dramatically reducing integration costs and complexity.
The economic impact is substantial. Organizations using traditional integration approaches often spend 15-20% of their IT budget maintaining custom interfaces. Those adopting standards-based interoperability typically see integration costs drop by 60-80% while gaining much greater flexibility to change vendors or add new capabilities.
Modern interoperability focuses on standards like HL7 FHIR that enable systems to communicate naturally without extensive custom programming. This approach also supports innovation by allowing third-party developers to create applications that work across multiple healthcare systems without requiring custom integration work for each deployment.
Real-World Implementation Challenges
While the concept of health data interoperability sounds straightforward, real-world implementation reveals complex challenges that organizations must steer carefully.
Data quality issues often surface when systems start sharing information. A hospital might find that their “clean” patient database contains thousands of duplicate records, inconsistent naming conventions, or missing critical information when they attempt to share data with external partners. Poor data quality doesn’t just create technical problems – it can lead to patient safety issues when providers receive incomplete or inaccurate information.
Workflow integration represents another significant challenge. Even when systems can technically share data, healthcare workers need that information presented in ways that fit their existing workflows. A nurse who’s used to seeing lab results in a specific format might miss critical abnormal values if interoperable data appears differently in their system. Successful interoperability requires careful attention to user experience design and change management.
Performance and scalability concerns emerge as data sharing volumes increase. A regional health information exchange might handle thousands of patient record requests per hour during peak times. Systems must be designed to handle these loads while maintaining sub-second response times that don’t disrupt clinical workflows.
Version control and system updates create ongoing complexity. When one organization updates their EHR system or changes their data formats, it can break interoperability connections with dozens of partner organizations. Successful interoperability requires governance processes that coordinate changes across multiple organizations and technical approaches that gracefully handle version differences.
Why Modern Healthcare Can’t Live Without It
66% of US healthcare costs go toward treating people with multiple chronic conditions. Two out of three older Americans juggle at least two ongoing health issues. When their medical information is scattered across systems that can’t communicate, managing their care becomes a nightmare.
Picture Maria, a 68-year-old with diabetes, heart disease, and arthritis. She sees multiple specialists, but none can see the complete picture. Her cardiologist prescribes medication that could interfere with her diabetes management, but he doesn’t have access to her latest blood sugar readings. Her rheumatologist adjusts her arthritis medication without knowing about her recent cardiac stress test results. Each provider makes decisions based on incomplete information, creating a cascade of suboptimal care decisions.
This fragmentation is the norm. Fewer than one in three US hospitals can electronically find, send, receive, and integrate patient information from other providers. The West Health Institute found that medical device interoperability alone could eliminate at least $36 billion of waste in hospitals.
Beyond dollars, this is about saving lives. When someone arrives unconscious at an emergency room, having instant access to their medication list, recent test results, and medical history can literally mean the difference between life and death. Emergency physicians report that lack of patient information contributes to diagnostic errors in approximately 12% of emergency department visits.
The COVID-19 pandemic starkly illustrated these gaps. Patients with breakthrough infections often couldn’t provide complete vaccination records to new providers. Contact tracing efforts were hampered by fragmented health data systems that couldn’t quickly identify exposure patterns. Countries with more integrated health data systems, like South Korea and Denmark, demonstrated significantly more effective pandemic responses.
Benefits for Every Stakeholder
Health data interoperability transforms healthcare for everyone involved in the care ecosystem:
Patients get control of their health story and experience truly coordinated care. Instead of repeating their medical history at every appointment, their complete record follows them seamlessly. Patient portals become comprehensive health dashboards showing information from all their providers. They can easily share their health information with family members, caregivers, or new providers. Research shows that patients with access to interoperable health records are 40% more likely to engage in preventive care and 25% more likely to adhere to treatment plans.
Healthcare providers can focus on caring for patients instead of hunting for information. Diagnostic uncertainty drops dramatically when doctors can see the complete patient picture with a few clicks. Primary care physicians report spending 30% less time on administrative tasks when they have seamless access to specialist reports and test results. Emergency department physicians can make faster, more accurate diagnoses when they have immediate access to patients’ medical histories, reducing average length of stay by 15-20 minutes per patient.
Specialists benefit enormously from comprehensive referral information. Instead of starting from scratch with each new patient, they receive complete context about why the patient was referred, what treatments have been tried, and what the referring provider’s specific concerns are. This leads to more efficient consultations and better treatment decisions.
Insurance companies can shift from reactive to proactive, identifying high-risk patients early and helping them avoid costly hospitalizations. Claims processing becomes more efficient when medical necessity can be verified automatically through integrated clinical data. Fraud detection improves significantly when insurers can cross-reference claims against comprehensive clinical records.
Public health agencies gain real-time disease surveillance instead of always playing catch-up. During COVID-19, countries with better health data integration responded faster and more effectively. Public health officials could track disease patterns, identify outbreaks, and coordinate responses based on real-time clinical data rather than waiting weeks for manual reporting.
Researchers can finally ask big questions and get meaningful answers when de-identified data from multiple sources can be safely combined. Clinical trials can recruit patients more efficiently by identifying eligible candidates across multiple health systems. Real-world evidence studies become possible at unprecedented scale, leading to faster medical breakthroughs and more personalized treatment approaches.
Healthcare administrators see operational improvements across multiple dimensions. Bed management becomes more efficient when hospitals can predict admissions based on emergency department and clinic data. Supply chain optimization improves when usage patterns can be analyzed across integrated systems. Quality improvement initiatives become more effective when outcome data can be tracked across the entire care continuum.
When Interoperability Is Missing
The absence of health data interoperability creates problems throughout healthcare that extend far beyond simple inconvenience. Information blocking became such a serious issue that it’s now illegal under federal law, with penalties reaching $1 million per violation.
Without proper data sharing, critical information gets lost at every handoff. A patient’s life-threatening allergy might not make it from their family doctor to the specialist. Lab results showing dangerous infections could sit in one system while the treating physician makes decisions based on incomplete information. Medication reconciliation errors occur in up to 70% of hospital admissions when complete medication histories aren’t available.
Over 20% of coronary stents placed in Medicare patients between 2019-2021 were unnecessary, wasting $2.44 billion. Many procedures might have been avoided if physicians had complete access to patients’ cardiac history, including previous stress tests, imaging studies, and treatment responses from other providers.
Duplicate testing represents another massive waste category. When providers can’t access recent test results, they often reorder expensive procedures “to be safe.” The average patient with multiple chronic conditions undergoes 2.3 duplicate imaging studies per year, costing the healthcare system approximately $12 billion annually. Beyond the financial waste, duplicate testing exposes patients to unnecessary radiation and delays appropriate treatment.
Care coordination failures become particularly dangerous for vulnerable populations. Elderly patients with multiple conditions often see 6-8 different specialists annually. Without interoperable systems, each provider works in isolation, leading to conflicting treatment plans, dangerous drug interactions, and fragmented care that confuses patients and families.
Emergency department inefficiencies multiply when critical patient information isn’t available. ED physicians report that lack of medical history information contributes to longer stays, more expensive workups, and increased patient anxiety. Patients with chronic conditions like diabetes or heart disease may receive suboptimal emergency treatment when their baseline values and treatment history aren’t accessible.
According to scientific research on medical device waste, when medical devices can’t communicate with each other or with electronic health records, it creates systematic inefficiencies that affect patient safety and drive up costs for everyone. Ventilators that can’t share data with monitoring systems require additional nursing time for manual documentation. Infusion pumps that don’t integrate with EHRs create opportunities for medication errors and require duplicate data entry.
The Economic Case for Interoperability
The financial arguments for health data interoperability are compelling across every sector of healthcare. Conservative estimates suggest that achieving full interoperability could save the US healthcare system $77.8 billion annually through reduced administrative costs, eliminated duplicate testing, improved care coordination, and better population health management.
Administrative cost savings represent the largest opportunity. Healthcare organizations currently spend approximately 8% of their total budgets on administrative activities related to data sharing, including manual data entry, phone calls to obtain records, faxing documents, and staff time spent tracking down patient information. Automated, standards-based data sharing could reduce these costs by 60-70%.
Clinical efficiency gains emerge when providers can access comprehensive patient information quickly. Studies show that physicians spend an average of 16 minutes per patient encounter searching for and reviewing external health information. Seamless interoperability could reduce this to 3-4 minutes, allowing providers to see more patients or spend more quality time with each patient.
Reduced medical errors translate directly to cost savings and improved outcomes. The Institute of Medicine estimates that medical errors cost the US healthcare system $17-29 billion annually. Many of these errors result from incomplete information at the point of care. Comprehensive, interoperable health records could prevent an estimated 25-30% of these errors.
Standards, Frameworks & Players Making Data Talk
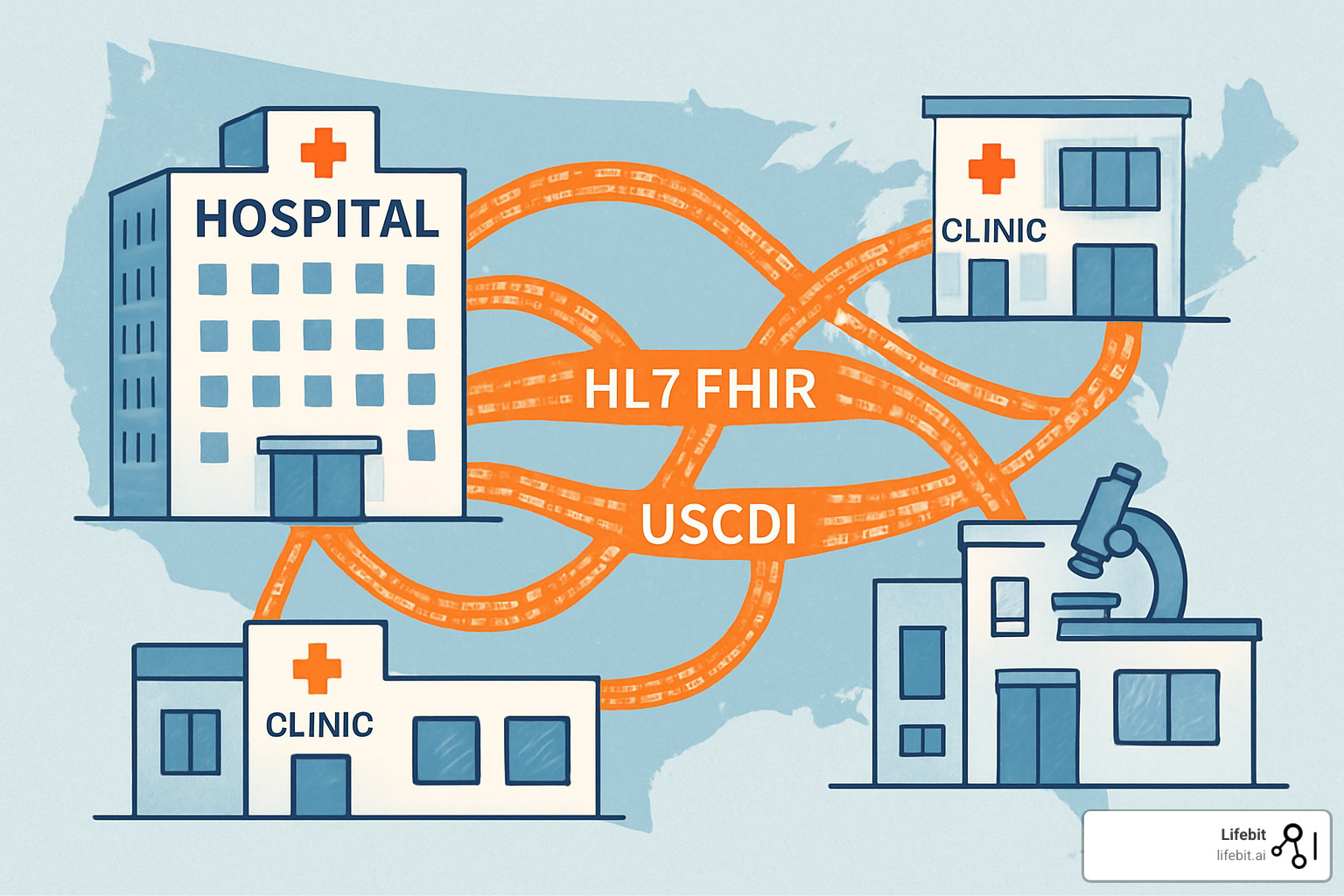
After decades of healthcare systems speaking different languages, we’re finally seeing real progress toward universal translation. The industry has rallied around common standards that make health data interoperability practical.
HL7 FHIR (Fast Healthcare Interoperability Resources) has become the breakthrough everyone was waiting for. Unlike clunky, complex standards that came before it, FHIR uses familiar web technologies like REST APIs and JSON – the same tools that power your favorite apps.
The US Core Data for Interoperability (USCDI) defines exactly what information must be shareable through standardized connections. Latest research on USCDI shows that health information organizations now make over two-thirds of required data elements available.
TEFCA (Trusted Exchange Framework and Common Agreement) creates governance rules that make nationwide data sharing possible. Canada has developed parallel frameworks with the Canadian Core Data for Interoperability (CACDI) and the Shared Pan-Canadian Interoperability Roadmap.
Specialized vocabularies ensure medical terms mean the same thing everywhere. SNOMED CT provides standardized codes for diagnoses and procedures, while LOINC does the same for laboratory tests.
More info about Health Data Standardisation explores how these different standards work together to create harmonious data exchange.
APIs & Fast FHIR Adoption
The move to API-based health data interoperability has transformed how quickly systems can share information. SMART on FHIR creates a secure platform where specialized healthcare apps can plug into any compatible EHR system.
The 21st Century Cures Act gave this movement legal teeth by requiring certified EHRs to provide patient-facing APIs. You can now use your smartphone to access your complete medical record and share it with any provider you choose.
While most health information organizations use older messaging standards, only about 15% have fully adopted modern FHIR APIs for routine operations. Organizations making the transition are seeing real benefits through easier application development and seamless integration.
Health Information Exchanges & QHINs
Health Information Exchanges (HIEs) have become essential infrastructure for large-scale data sharing. Major networks like the eHealth Exchange now connect over 75% of US hospitals and 40,000 medical groups. CommonWell Health Alliance serves 34,000 provider sites representing 231 million patients.
The real magic happens when these networks connect through TEFCA to become Qualified Health Information Networks (QHINs). This creates a nationwide web where any authorized provider can access patient information regardless of which network they belong to.
During emergencies, this connectivity becomes life-saving. When someone has a heart attack while traveling, emergency room doctors can now access their complete medical history within minutes instead of days.
Barriers on the Road—And How to Get Past Them
If achieving health data interoperability were easy, we’d have solved it decades ago. Healthcare organizations face a perfect storm of technical, organizational, and policy challenges.
The biggest culprit? Legacy systems older than some doctors using them. Picture a hospital running an EHR from 2003 trying to talk to a modern cloud-based lab system. These systems weren’t built with sharing in mind, creating data silos that persist even within single organizations.
Privacy and security concerns add complexity that keeps IT directors awake at night. Healthcare organizations handle extremely sensitive personal information. A single HIPAA violation can result in millions in fines, and cyberattacks on healthcare systems have tripled recently.
Patient consent management creates its own maze. Some states require explicit opt-in consent for data sharing. Others use opt-out models. Many allow patients to restrict sharing of sensitive information like mental health records. Managing these preferences across multiple systems becomes a full-time job.
The challenge isn’t just technical – it’s deeply human. Healthcare workers are already overwhelmed. If accessing external patient records requires logging into three different systems and waiting five minutes, busy clinicians will skip it.
More info about Data Harmonization challenges explores how organizations can overcome these barriers while maintaining data quality and compliance.
Tackling Technical Obstacles
Most technical barriers have solutions – they just require planning, investment, and patience. Data mapping lies at the heart of most interoperability challenges. When one system stores blood pressure as “120/80 mmHg” and another expects separate numeric values, someone needs to write translation rules.
Master patient indexes solve the tricky problem of matching patients across systems. Advanced algorithms now use multiple data points to create probabilistic matches with over 95% accuracy.
Cloud migration offers a path forward for organizations trapped by legacy systems. Modern cloud platforms provide FHIR-native databases and pre-built integration tools that dramatically reduce complexity.
Organizational & Policy Problems
Perfect technical architecture means nothing if your organization isn’t ready for change. Change management becomes crucial because interoperability almost always requires clinicians to modify established workflows.
Smart organizations involve clinicians in design from day one, create intuitive workflows, and measure success by adoption rates, not just technical functionality.
The federal Information Blocking Rule makes it illegal for healthcare providers and IT developers to deliberately interfere with health information access. Violations can result in fines up to $1 million per incident, finally tipping the scales toward openness and interoperability.
Global Roadmaps, Laws & The Future
Governments worldwide are recognizing that health data interoperability isn’t optional – it’s essential infrastructure for modern healthcare. The wave of new legislation represents the biggest shift in healthcare data governance in decades.
Canada made headlines with Government of Canada Bill C-72, the Connected Care for Canadians Act. This requires health IT vendors to ensure their systems can communicate and makes information blocking illegal.
The 21st Century Cures Act continues changing the US healthcare landscape. Its information blocking provisions and API requirements are forcing industry openness. Patients now have legal rights to access their health information through any app they choose.
Europe’s European Health Data Space (EHDS) aims to create continent-wide health data sharing. The Nordic countries are already testing cross-border patient data sharing, allowing citizens to access healthcare anywhere with their medical records automatically available.
More info about Changing Health Data 2023 explores how these global trends create new opportunities while addressing longstanding healthcare delivery challenges.
Innovation Horizon
The future of health data interoperability goes beyond getting existing systems to communicate. We’re entering an era where connected health data enables entirely new care delivery methods.
AI-powered triage systems with access to complete patient histories through interoperable networks make much smarter decisions about who needs immediate attention. Real-time analytics platforms can spot disease patterns within hours instead of months.
Federated research networks enable breakthrough findies while maintaining the highest privacy standards. Digital twins – virtual copies of patients or healthcare systems – become possible with comprehensive, real-time data flow.
Wearable device integration creates continuous health data streams that inform clinical decisions in real-time, enabling truly personalized, preventive care.
Steps Organizations Can Take Today
Organizations don’t need to wait for perfect standards to start their interoperability journey:
Start by assessing where you are today using frameworks like HIMSS’s interoperability maturity model. Adopt open standards wherever possible, making FHIR and USCDI non-negotiable requirements for new systems.
Join your regional Health Information Exchange even with limited current capabilities. Get tough with technology vendors by enforcing open contracts that prevent information blocking and require standard API support.
Invest in solid data governance frameworks addressing privacy, security, and consent management. Train your staff on both technical and clinical aspects of interoperability.
Frequently Asked Questions about Health Data Interoperability
When organizations start their health data interoperability journey, they often have similar questions about privacy, regulations, and practical implementation. Let me address the most common concerns I hear from healthcare leaders.
What is information blocking and how do new laws address it?
Information blocking happens when healthcare organizations, technology vendors, or data exchanges deliberately make it hard to access or share patient information. Think of it as digital hoarding – keeping valuable health data locked away when it could help patients get better care.
This might look like charging outrageous fees for basic data exports, creating unnecessarily complex technical barriers, or requiring patients to jump through multiple hoops just to get their own medical records. Some organizations used to view patient data as a competitive asset they needed to protect from rivals.
The 21st Century Cures Act changed everything by making information blocking illegal. Health IT developers and networks can face penalties up to $1 million per violation. Healthcare providers can receive civil monetary penalties through the Office of Inspector General. The law isn’t just symbolic – it has real teeth.
The regulations include reasonable exceptions for legitimate concerns like protecting patient safety or preventing cybersecurity threats. But they make it clear that data belongs to patients, not the organizations that happen to store it.
This legal shift recognizes what we’ve known for years: when health information gets trapped in silos, patients suffer and healthcare costs skyrocket. By forcing transparency and access, these laws are finally aligning technology incentives with patient needs.
How do FHIR APIs protect patient privacy?
One of the biggest misconceptions about health data interoperability is that more data sharing automatically means less privacy. Actually, modern FHIR APIs often provide better privacy protection than traditional systems.
The SMART on FHIR framework requires OAuth 2.0 authentication, which is the same security standard used by your online banking. Only authorized applications with proper patient consent can access health data. No backdoors, no shortcuts.
Patient consent becomes incredibly granular. Instead of all-or-nothing access, patients can authorize a diabetes app to see their glucose readings and medications while keeping their mental health records completely private. They control exactly what gets shared with whom.
Every API access gets logged in detail, creating clear audit trails of who accessed what data when. This transparency actually improves privacy protection compared to older systems where data access often happened without detailed tracking.
FHIR also supports advanced privacy techniques like differential privacy and federated analytics. These approaches allow researchers and clinicians to generate insights from large datasets without exposing individual patient information. At Lifebit, we use these techniques to enable secure collaboration across our federated platform while maintaining strict privacy controls.
The key insight is that better interoperability doesn’t mean weaker privacy – it means smarter, more controlled data sharing that puts patients in charge.
What’s the quickest first step for a small clinic?
Small healthcare practices often feel overwhelmed by interoperability requirements, but you don’t need to boil the ocean on day one. Start with the patient-facing APIs that federal law already requires – most modern EHR systems have these capabilities built in.
Begin by enabling patient access to their own data through your EHR’s patient portal or compatible third-party apps. This provides immediate value to your patients while ensuring compliance with information blocking regulations. Many practices find this feature was available all along but just needed to be activated.
Next, look at your most common referral patterns. If you regularly send patients to the same specialists or hospital system, investigate what data sharing capabilities already exist between your systems. Many EHR vendors have built-in connections to health information exchanges that might just need to be turned on.
Consider joining your regional Health Information Exchange if you haven’t already. The onboarding process typically includes technical support and training that can accelerate your entire interoperability journey. Plus, HIEs often provide valuable services like patient matching and care alerts.
Finally, make FHIR compatibility a requirement when evaluating any new systems or upgrades. Don’t accept vendor promises about “future interoperability” – insist on current standards support with demonstrated functionality.
The most important step is simply starting. Every small improvement in data sharing makes your practice more connected to the broader healthcare ecosystem and better positioned for future requirements.
Conclusion
The change of healthcare through health data interoperability isn’t some far-off dream – it’s happening right now. From Canada’s Bill C-72 to Europe’s Health Data Space initiative, governments worldwide are recognizing that healthcare can’t work properly when patient data is trapped in silos.
We’re talking about billions in cost savings, thousands of preventable deaths avoided, and genuinely better care for millions of patients with chronic conditions. As Americans living with chronic diseases climb from 141 million today to a projected 171 million by 2030, coordinated care becomes absolutely essential.
Organizations that accept health data interoperability today aren’t just solving current problems – they’re building the foundation for healthcare’s digital future. Those who delay risk scrambling to catch up as standards solidify and regulations tighten.
At Lifebit, we’ve seen what becomes possible when health data works together seamlessly. Our federated AI platform demonstrates how you can achieve secure collaboration and cutting-edge analytics without compromising privacy or governance. Our Trusted Research Environment (TRE), Trusted Data Lakehouse (TDL), and R.E.A.L. (Real-time Evidence & Analytics Layer) components open up insights from data across organizations while maintaining proper protection.
The future we’re heading toward is connected, intelligent, and patient-centered healthcare. More info about connected solutions demonstrates how federated approaches can release health data’s full potential while addressing privacy and security concerns.
The question isn’t whether health data interoperability will reshape healthcare – that’s already happening. The real question is whether your organization will be ready to make the most of it. The best time to start was yesterday. The second-best time is right now.



One thought on “When Health Data Plays Nice Together (Finally!)”
Comments are closed.