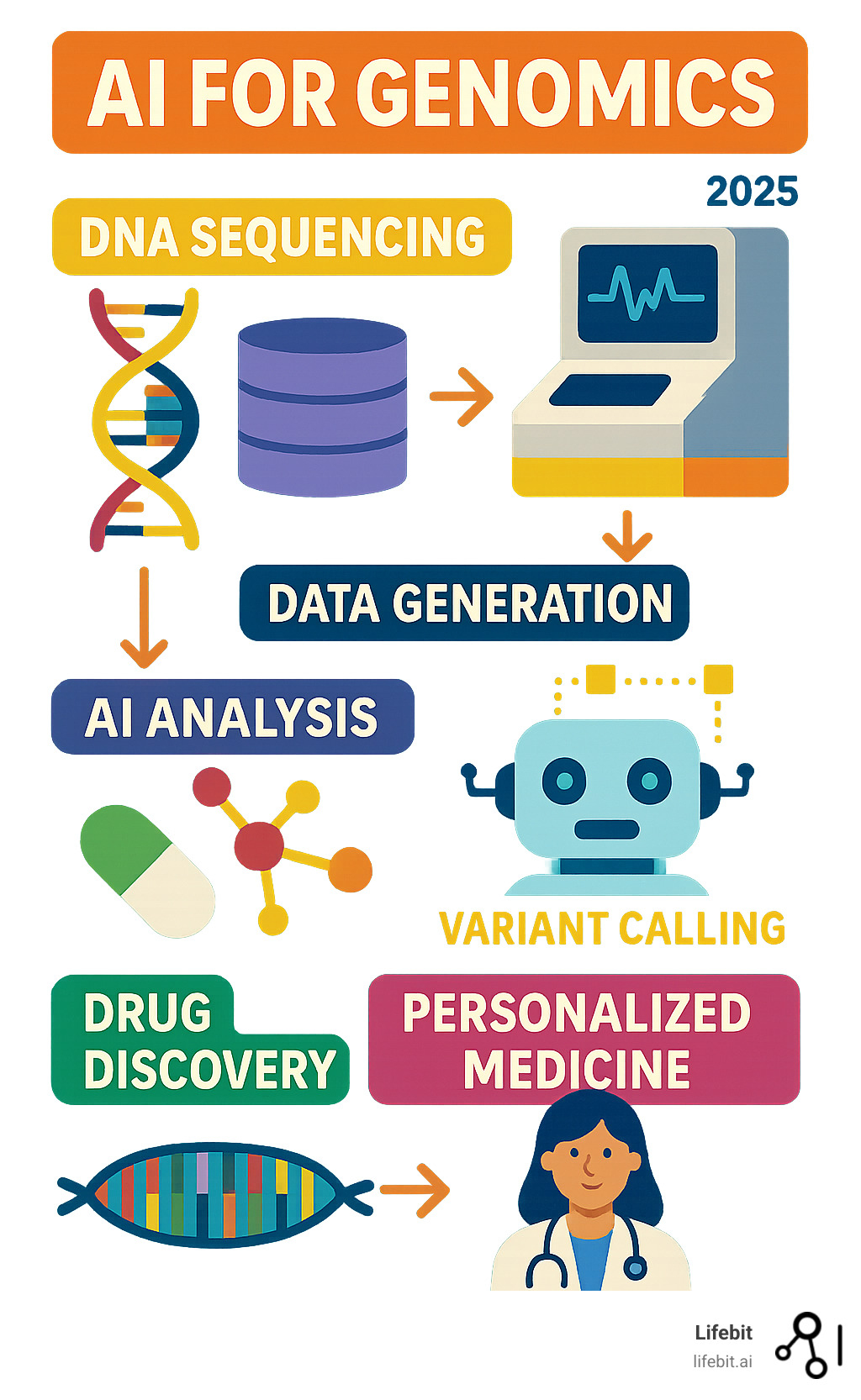
AI for Genomics: The 2025 Revolution
The Data Deluge: Why Genomics Needs Artificial Intelligence
The field of genomics is undergoing a massive change. Our DNA holds a wealth of information vital for future healthcare, but its sheer volume and complexity make AI for Genomics essential.
AI for Genomics uses artificial intelligence to open up the secrets hidden in our DNA. It helps us process huge amounts of genetic data faster and more accurately than ever before. This technology is changing how we approach health and medicine.
Here are the key ways AI is applied in genomics:
- Accelerating Research: AI speeds up the analysis of genomic data, from sequencing to interpretation.
- Finding New Drugs: It helps identify potential drug targets and predict patient responses to treatments.
- Diagnosing Diseases: AI improves the detection of genetic mutations linked to diseases, including rare conditions.
- Enabling Personalized Medicine: It creates custom treatments based on an individual’s unique genetic makeup.
- Understanding Gene Function: AI helps uncover the roles of different genes and how they impact health.
This guide explores how AI tackles massive genomic datasets, driving breakthroughs in drug findy, disease diagnosis, and personalized healthcare.
With over 15 years in computational biology and health-tech, including my role at Lifebit enabling secure drug findy, my work in AI for Genomics is extensive. My background, with a PhD in Biomedicine and an MSc in Bioinformatics, has fueled contributions to tools like Nextflow and the advancement of AI-driven precision medicine.
Imagine trying to drink from a firehose – that’s what dealing with genomic data feels like. The genomics revolution, driven by Next-Generation Sequencing (NGS), has been phenomenal. Sequencing a human genome, once costing millions, is now under $1,000 and takes days. This has democratized access but also releaseed a data deluge.
A single human genome generates about 100 gigabytes of data. With millions of genomes being sequenced globally, the numbers are staggering. By 2025, genomic data could reach 40 exabytes (a billion gigabytes each). Learn more about this projection here: 40 exabytes by 2025.
This data growth outpaces traditional computation, creating a bottleneck that challenges supercomputers and Moore’s Law. Analysis pipelines struggle to keep up, delaying critical insights. A Nature Biotechnology article highlights this, stating, “The rapid growth of genomic data is outstripping our ability to analyze it effectively…” Explore this challenge here: Analysis pipelines struggling.
This is where AI for Genomics is crucial. Manual analysis can’t handle petabytes of data to find subtle, key patterns. AI provides the computational power and pattern-recognition to turn this data into actionable knowledge. Without it, valuable information in our DNA would remain locked away.
Explaining the Tech: AI, Machine Learning, and Deep Learning in Genomics
To understand how AI for Genomics is changing healthcare, we must first clarify its core technologies. Artificial Intelligence (AI), Machine Learning (ML), and Deep Learning (DL) are often used interchangeably but are distinct. Think of them as Russian nesting dolls: AI is the largest, containing ML, which in turn contains DL.
- Artificial Intelligence (AI) is the broadest concept: the simulation of human intelligence in machines. It involves creating systems that can perceive, reason, learn, and problem-solve. The AI100 Stanford report defines it as “the science and engineering of making intelligent machines.” Read more here: One such definition.
- Machine Learning (ML) is a subset of AI where systems learn from data without explicit programming. ML algorithms identify patterns to make predictions, such as distinguishing between healthy and diseased genomic sequences after analyzing thousands of examples.
- Deep Learning (DL) is a specialized subset of ML using multi-layered artificial neural networks (hence “deep”). Inspired by the human brain, these networks process vast datasets to find intricate relationships invisible to traditional ML methods.
The relationship is hierarchical: all DL is ML, and all ML is AI. In genomics, ML and especially DL are leveraged to tackle complex, high-dimensional genetic data.
Within ML, we broadly distinguish between several learning paradigms:
- Supervised Learning: The model is trained on a “labeled” dataset where the correct output is known. For instance, training a model on thousands of genomic variants that have been expertly labeled as either “pathogenic” or “benign.” The model learns the features associated with each label and can then classify new, unseen variants.
- Unsupervised Learning: The model works with unlabeled data to find hidden patterns or structures. This is useful for exploratory analysis, such as clustering patients into distinct subgroups based on their gene expression profiles, potentially revealing new disease subtypes that respond differently to treatment.
- Reinforcement Learning: This involves an AI agent learning to make a sequence of decisions in an environment to maximize a cumulative reward. In genomics, this could be used to design optimal treatment strategies over time or to create novel protein sequences by rewarding designs that exhibit desired functional properties.
Core AI Models in Genomic Analysis
The specific types of AI models we deploy vary depending on the genomic task at hand:
- Convolutional Neural Networks (CNNs): Originally for image recognition, CNNs are powerful for identifying spatial patterns. In genomics, they are adapted to analyze sequence data by treating it as a 1D or 2D grid. For example, a DNA sequence can be one-hot encoded into a matrix, allowing the CNN to learn to recognize specific sequence patterns, or “motifs,” like transcription factor binding sites, that are indicative of regulatory function. Learn more: Analyzing sequence patterns.
- Recurrent Neural Networks (RNNs): RNNs are designed for sequential data, where order matters, making them ideal for genomic sequences (A, T, C, G) or protein sequences. Variants like Long Short-Term Memory (LSTM) networks are particularly effective as they can capture long-range dependencies in the data, which is crucial for understanding how distant parts of a gene or protein interact. They are used for tasks like predicting protein structure or identifying disease-linked variations. Learn more: Processing sequential data.
- Transformer Models: An evolution of RNNs, transformers use an attention mechanism to weigh the importance of different parts of the input data. This has made them state-of-the-art in natural language processing and increasingly powerful in genomics. Foundation models pre-trained on vast amounts of sequence data can be fine-tuned for specific tasks like predicting gene expression or variant effects.
- Generative Models: Models like Generative Adversarial Networks (GANs) or Variational Autoencoders (VAEs) can generate new data that resembles the training data. In genomics, this is a powerful tool for designing novel proteins with specific functions, creating realistic synthetic genomic datasets to augment research without compromising patient privacy, or simulating the effects of mutations to better understand disease mechanisms.
By understanding these core technologies, we can better appreciate how AI for Genomics is revolutionizing the way we interpret and apply genetic information to improve human health.
Changing Findy: Key Applications of AI for Genomics
We’ve covered the ‘what’ and ‘why’ of AI for Genomics; now for the ‘how.’ This technology is changing everything from basic gene function to drug findy and personalized healthcare. Let’s explore its most impactful applications.
Accelerating Analysis: How AI for Genomics Speeds Up Variant Calling
Variant calling in genomics is like finding every typo in a giant instruction manual—your DNA. It involves identifying all differences, from single-letter changes (SNVs) to large structural rearrangements, in a person’s DNA compared to a reference. With millions of potential variants in a genome, traditional methods are slow, computationally expensive, and struggle with accuracy, especially for complex variants.
The process involves aligning sequenced DNA fragments to a reference genome using tools like BWA-MEM or STAR, then identifying differences. This is where AI for Genomics shines. GPU acceleration, using powerful chips like NVIDIA’s H100, has been a game-changer. Tools like NVIDIA Parabricks can accelerate genomic tasks by up to 80x, reducing processes that took hours, like HaplotypeCaller, to minutes.
AI also dramatically improves accuracy. Google’s DeepVariant, for example, reframes variant calling as an image classification problem. It creates images of the aligned DNA reads around a potential variant site and uses a deep neural network to classify these images, distinguishing true variants from sequencing errors with remarkable precision. This approach often outperforms older statistical methods. Tools like NVScoreVariants further refine these findings, enabling faster, more accurate data processing, which is vital for research and clinical diagnostics.
Beyond single-letter changes, AI excels at detecting large Structural Variants (SVs)—deletions, duplications, inversions, and translocations of large DNA segments. These SVs are often linked to severe genetic diseases and cancers but are notoriously difficult to detect with standard methods. AI models can learn the complex signatures these SVs leave in sequencing data, providing a much clearer picture of genomic architecture.
From Code to Cure: The Role of AI for Genomics in Drug Findy
The path from a genetic insight to a new medicine is typically long (10-15 years), costly (over $2 billion), and has a failure rate of over 90%. AI for Genomics is revolutionizing this journey, accelerating every step from target identification to predicting patient response.
Here’s how AI is changing drug findy:
- Target Identification: AI sifts through massive multi-omic datasets—integrating genomics, transcriptomics, proteomics, and clinical data—to find novel drug targets. By identifying subtle patterns that link genes or proteins to disease pathology, AI helps researchers focus on the most promising candidates early on, reducing the risk of late-stage failure.
- Biomarker Findy: AI helps uncover new biomarkers—biological clues for early disease detection, progression tracking, and predicting treatment efficacy. This is crucial for developing companion diagnostics that ensure the right patient gets the right drug.
- Drug Repurposing: AI can identify new uses for existing drugs by analyzing molecular and genetic data. By finding overlaps between the disease mechanism and a drug’s mode of action, AI can suggest repurposing candidates, dramatically shortening the development timeline and cost.
- Predicting Drug Response: By analyzing a patient’s genetic data against drug response data from others, AI models can predict treatment efficacy and potential side effects, leading to smarter, personalized plans.
- Improving Gene Editing Tools: AI improves tools like CRISPR by helping ML models predict optimal guide sequences, reduce off-target effects, and design novel systems. This accelerates the development of gene therapies. Learn more here: Improving gene editing tools like CRISPR.
- Protein Structure Prediction: Understanding a protein’s 3D shape is vital for drug design. The game-changing AI system AlphaFold accurately predicts protein structures from their amino acid sequence. Its successor, AlphaFold 3, goes even further, modeling interactions between proteins, DNA, RNA, and other molecules, offering unprecedented insights for designing drugs that target these complex interactions.
Advancing Functional Genomics and Disease Diagnosis
AI for Genomics is also revolutionizing our understanding of gene function and the diagnosis of genetic diseases. A key challenge has been interpreting the non-coding genome. This 98% of our DNA doesn’t code for proteins but contains critical regulatory elements like improvers and silencers. AI models can now predict the function of these regions directly from the DNA sequence, helping us understand how non-coding variants contribute to disease.
- Gene Function Prediction: By analyzing evolutionary data, gene expression levels, and protein interactions, AI algorithms can predict the function of unknown genes, accelerating basic biological research.
- Identifying Disease-Causing Genomic Variants: Deep learning models can sift through millions of genetic variants to pinpoint the specific changes responsible for a disease. This is crucial for rare diseases with subtle or unique genetic causes. Learn more here: Identifying disease-causing genomic variants.
The long, frustrating path to a diagnosis for rare genetic conditions—the “diagnostic odyssey”—is being shortened by AI for Genomics. By analyzing a patient’s genetic data and symptoms, AI can spot subtle clues missed by older methods, including complex changes like CNVs found in disorders like Angelman or DiGeorge syndrome. As Professor Matthew Hurles of the Wellcome Sanger Institute noted, “a single genomic test promises accelerated diagnoses for rare genetic diseases,” highlighting the power of AI-driven testing to bring faster relief and care to patients. Read more here: Wellcome Sanger Institute’s directory and study author Professor Matthew Hurles said.
The Dawn of Personalized Medicine: How AI is Tailoring Healthcare

Imagine healthcare custom to your unique genetic blueprint. This is the vision of personalized medicine, and AI for Genomics is the engine making it a reality, shifting us from one-size-fits-all treatments to highly customized care.
Precision medicine relies on understanding our unique genetic differences. AI helps interpret these nuances, allowing for patient stratification—grouping individuals by their genomic profiles to ensure they receive the most effective therapies.
In cancer genomics, AI is a game-changer. Instead of treating cancer by location (e.g., lung, breast), we now analyze a tumor’s genomic landscape. AI pinpoints driver mutations and can even predict cancer progression, enabling oncologists to select targeted therapies. Furthermore, AI can analyze tumor heterogeneity—the mix of different cell populations within a single tumor—to predict resistance to therapy and guide combination treatments. This is a monumental leap from the broad effects of traditional chemotherapy. Learn more about AI’s predictive power here: Predicting cancer progression.
Liquid biopsy analysis is another exciting frontier. This non-invasive technique detects circulating tumor DNA (ctDNA) in a blood sample. The challenge is immense: ctDNA can constitute less than 0.01% of the total cell-free DNA in the bloodstream, making its detection like finding a needle in a haystack. AI algorithms act as expert detectives, using sophisticated pattern recognition to filter out the “noise” and accurately identify these tiny, cancer-specific DNA fragments. This allows for earlier cancer detection, real-time treatment monitoring, and recurrence spotting without invasive biopsies.
AI also powers Polygenic Risk Scores (PRS), which act as a genetic health report. A PRS quantifies an individual’s genetic risk for common conditions like heart disease or diabetes by summing the effects of thousands or millions of genetic variants. This tool enables proactive, personalized screening and prevention strategies. However, a major challenge is ensuring equity. Most genomic data used to develop PRS comes from individuals of European ancestry, making the scores less accurate for other populations. Addressing this bias by building more diverse datasets is a critical area of research to prevent AI from widening health disparities.
Pharmacogenomics, the study of how genes affect drug response, is being revolutionized by AI. By analyzing genetic variants, AI can predict how an individual will metabolize drugs. For example, variations in the CYP2D6 gene affect how over 25% of all prescribed drugs are processed, including antidepressants and opioids. Similarly, variants in the TPMT gene can cause severe toxicity from common chemotherapy drugs. AI-driven analysis can help physicians select the right drug and dose from the start, minimizing adverse reactions and maximizing efficacy for safer, more impactful treatments.
The Lifebit platform is built to support this vision. We provide secure, real-time access to global biomedical and multi-omic data, allowing researchers to integrate genomic, clinical, and lifestyle data. This creates a holistic patient view, ushering in the era of personalized healthcare.
The Road Ahead: Challenges and the Future of AI in Genomics
While the promise of AI for Genomics is immense, we must steer several challenges to realize its full potential.
Key problems include data quality and privacy. AI models require high-quality, standardized, and diverse data, but genomic data can be noisy, incomplete, or biased. As genomic information is highly sensitive, protecting patient privacy is paramount. Our federated AI platform addresses this by enabling analysis without moving data, ensuring security and compliance.
Algorithmic bias is another major concern. Models trained on non-diverse datasets, which are common in genomics, can amplify health disparities. This is a critical ethical and scientific challenge that requires a concerted effort to diversify data collection.
The black box problem—the opacity of many deep learning models—is a significant barrier to clinical adoption. For a doctor to trust an AI’s recommendation, they need to understand its reasoning. This has led to the rise of Explainable AI (XAI), a field focused on developing models that can provide clear justifications for their outputs. An XAI model might not only predict a variant as pathogenic but also highlight the specific sequence features or biological pathways that led to its decision, building crucial trust and enabling clinical validation.
Finally, regulatory problems and a shortage of skilled bioinformaticians are significant challenges. Regulatory frameworks, such as the FDA’s guidance on Software as a Medical Device (SaMD), are still evolving to keep pace with rapid AI advancements. Concurrently, there is a growing demand for experts who can bridge the complex worlds of biology and data science.
The Rise of Large Language Models (LLMs) in Genomics
An exciting development is the application of Large Language Models (LLMs) and other foundation models to genomics. Known for understanding and generating text, their potential is now extending to the “language of life.” Genomics-specific models like Geneformer and the Nucleotide Transformer are pre-trained on massive datasets of DNA sequences. They learn the fundamental grammar of the genome and can then be fine-tuned for a wide range of tasks.
A recent UC San Diego study found that LLMs could automate functional genomics tasks, achieving 73% accuracy in predicting gene function from text with minimal hallucination. This suggests LLMs could become powerful tools for summarizing literature, generating hypotheses, and designing experiments. Explore the study here: UC San Diego study and see more from the Ideker Lab web portal.
The Role of Collaboration and Generative AI
The future of AI for Genomics will be built on collaboration and generative AI.
Generative AI holds immense promise for synthetic genomics—designing novel biological systems from scratch. The Sanger Institute’s programme in this area aims to engineer biology for applications from disease modeling to biotechnology, potentially accelerating the creation of new therapies and tools. Learn more here: Sanger Institute’s programme. Furthermore, generative models can create high-fidelity synthetic patient data. This data can be used to augment rare disease datasets or be shared openly for research, accelerating findy without compromising the privacy of real individuals.
Collaboration is key, as no single institution can tackle genomics alone. Initiatives like the NIH and NHGRI’s Bridge to Artificial Intelligence (Bridge2AI) program exemplify this spirit, aiming to generate new data and tools to accelerate biomedical findy. Learn more: Bridge to Artificial Intelligence (Bridge2AI). Such partnerships are essential for pushing the boundaries of AI for Genomics. Our platform is designed to facilitate this type of secure, large-scale, compliant research.
Frequently Asked Questions about AI in Genomics
Here are answers to some of the most common questions about AI for Genomics and its impact on healthcare.
What is the main role of AI in genomics?
The main role of AI for Genomics is to analyze the massive, complex datasets that modern genomics produces. Traditional methods cannot handle this “data deluge.” AI algorithms act as data detectives, sifting through information to find meaningful patterns that humans would miss. This accelerates research, brings insights to the clinic faster, and helps open up the secrets hidden in our DNA.
How does AI help in identifying genetic diseases?
AI for Genomics is a game-changer for identifying genetic diseases, especially rare ones. The journey to a diagnosis, often called a “diagnostic odyssey,” can be long and frustrating. AI, particularly deep learning, excels at analyzing a patient’s genome and symptoms to find subtle disease-causing variants, including complex changes like Copy Number Variants (CNVs). By identifying the genetic cause quickly and accurately, AI dramatically shortens the diagnostic process, allowing patients to receive answers and appropriate care much sooner.
Is AI replacing human geneticists?
No, AI is not replacing human geneticists. It’s a common misconception. Think of AI for Genomics as a powerful assistant. It automates data-heavy tasks and identifies patterns at a scale humans cannot, but it doesn’t replace human expertise. Geneticists and researchers are essential for interpreting AI-driven insights, making complex clinical decisions, and providing ethical oversight. It’s a partnership between technology and human intellect to advance medicine.
Conclusion
We’ve explored how AI for Genomics is turning the data deluge from next-generation sequencing into powerful, actionable insights. AI makes sense of billions of base pairs, accelerating everything from variant calling to drug findy.
This represents a fundamental shift towards a proactive, predictive, and personalized future for healthcare. By pinpointing genetic causes of disease and tailoring treatments, AI is open uping the full potential of genomic information.
The future of personalized healthcare is happening now, thanks to the synergy between biology and technology. At Lifebit, we are proud to be at the forefront of this revolution with our next-generation federated AI for Genomics platform.
Our platform provides secure, real-time access to global biomedical datasets, featuring smart harmonization and advanced AI/ML analytics. With robust federated governance, we empower large-scale, compliant research and pharmacovigilance for biopharma and public health agencies. We deliver real-time insights, AI-driven safety surveillance, and secure collaboration to bring life-changing findies to patients faster.
To learn how we’re enabling real-time pharmacovigilance, find more information here: More info about Real-Time Pharmacovigilance. The genomics revolution, powered by AI for Genomics, is just beginning, and we are excited to lead the way!