Unlocking Breakthroughs: Your Clinical Development Platform Playbook

Clinical Development Platform: Top 10 Essential Breakthroughs
Why Clinical Development Platforms Are Changing Medical Research
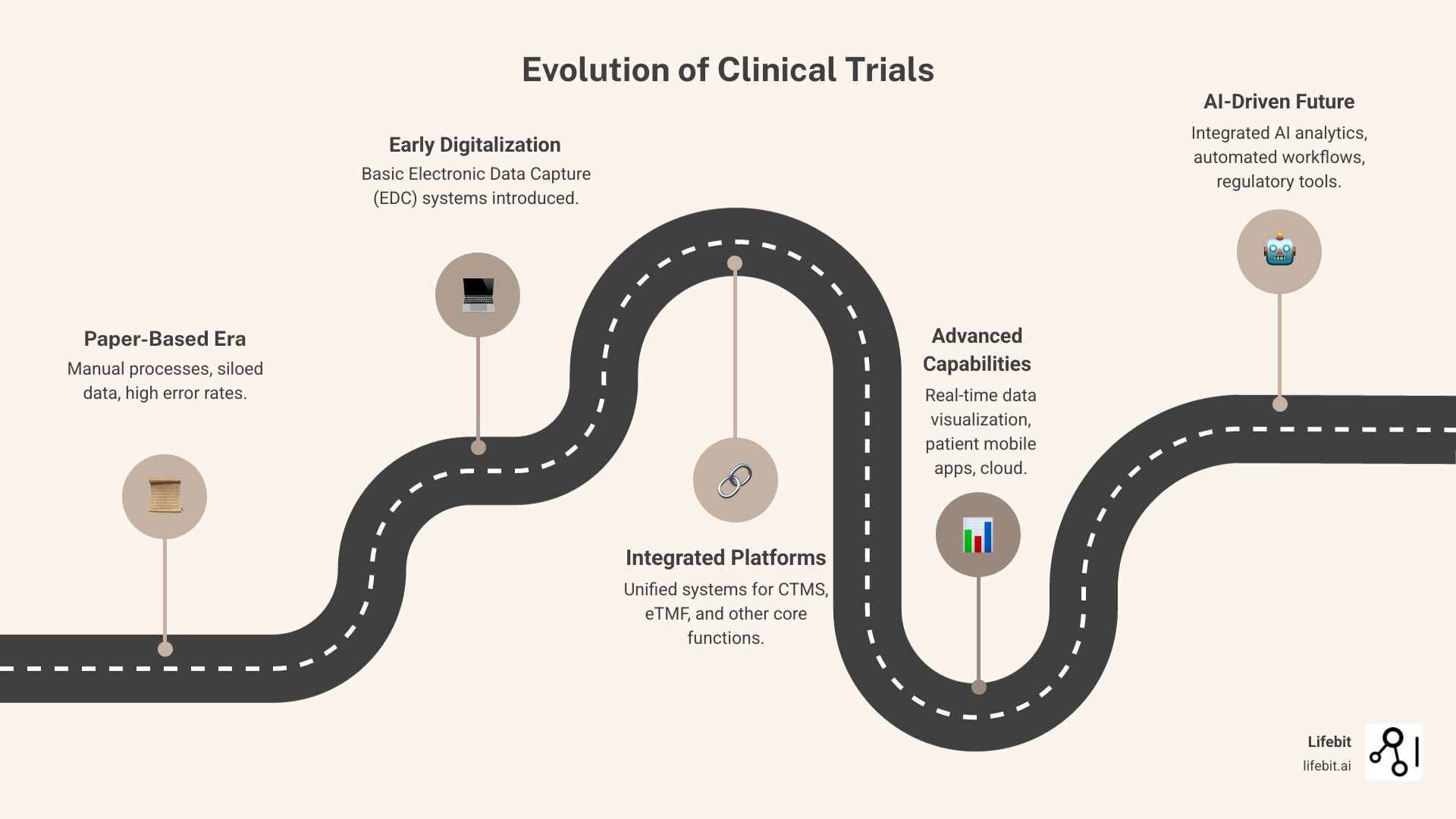
A clinical development platform is a unified software solution that integrates all aspects of clinical trial management, from study design and patient recruitment to data collection and regulatory submission. These platforms combine essential tools like Electronic Data Capture (EDC), Clinical Trial Management Systems (CTMS), and patient engagement technologies into a single, streamlined environment.
Key components of a clinical development platform:
- Electronic Data Capture (EDC) – Collects and manages trial data
- Clinical Trial Management System (CTMS) – Tracks study operations and milestones
- Electronic Clinical Outcome Assessment (eCOA/ePRO) – Captures patient-reported outcomes
- Randomization and Trial Supply Management (RTSM) – Manages patient randomization and drug supply
- Electronic Trial Master File (eTMF) – Maintains regulatory documentation
- AI and analytics tools – Provides predictive insights and automation
The shift from fragmented, paper-based processes to integrated digital platforms is revolutionizing how clinical trials are conducted. Organizations using unified platforms report up to 3x faster study completion timelines, 40% reduction in monitoring costs, and 13x ROI for Phase III trials. As one industry expert noted, “The life sciences industry is moving away from fragmented, standalone tools and embracing integrated, platform-based solutions.”
Modern clinical development platforms address critical challenges faced by pharmaceutical companies, regulatory agencies, and research institutions: slow data onboarding, poor data quality, regulatory bottlenecks, and the inability to access real-time insights across siloed datasets. These platforms enable secure, compliant access to diverse data sources while supporting both technical researchers and business users.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit, where I’ve spent over 15 years building genomics and biomedical data platforms that power precision medicine research. My experience developing clinical development platform solutions for global pharmaceutical companies and public sector institutions has shown me how the right technology can dramatically accelerate the path from findy to patient care.
What Are the Core Components of a Clinical Development Platform?
At its heart, a clinical development platform is a sophisticated ecosystem designed to streamline every phase of a clinical trial. It replaces disjointed software and manual processes with a cohesive, efficient workflow. Its core components are interconnected modules that share data seamlessly, providing a single source of truth. This integration is crucial for data quality, regulatory compliance, and accelerating research.
Essential Functionalities for Modern Research
To truly understand a clinical development platform, we need to dig into its essential functionalities. These are not just separate tools but deeply integrated modules that create a powerful, end-to-end research engine.
Electronic Data Capture (EDC)
As the backbone for collecting and managing trial data, a modern EDC system goes far beyond replacing paper forms. It provides real-time data entry with automated edit checks that instantly validate information, flagging inconsistencies or out-of-range values. This proactive approach to data cleaning significantly reduces downstream effort. A sophisticated query management system is also built-in, allowing data managers and monitors to raise, track, and resolve data discrepancies directly within the platform. This creates a clear, auditable trail for all data clarifications, ensuring the final dataset is clean, accurate, and ready for analysis.
Clinical Trial Management System (CTMS)
As the trial’s operational command center, the CTMS provides granular project management capabilities, tracking everything from site activation and patient enrollment rates to regulatory submission deadlines. It helps sponsors and CROs manage resources effectively, monitor site performance against key performance indicators (KPIs), and handle complex trial financials, including investigator payments and budget forecasting. This comprehensive oversight allows for proactive risk management, enabling teams to identify and mitigate potential bottlenecks before they derail study timelines.
Electronic Trial Master File (eTMF)
More than a digital filing cabinet, a modern eTMF is a dynamic, collaborative workspace for all essential trial documents. Often structured according to the industry-standard TMF Reference Model, it provides a standardized framework for organizing thousands of files. Advanced features like version control, automated workflows for document review and approval, and role-based access ensure that all stakeholders are working with the correct, most up-to-date information. This level of organization and control is critical for maintaining a constant state of inspection readiness, allowing for smooth audits and regulatory reviews.
Randomization and Trial Supply Management (RTSM)
An integrated RTSM system is critical for maintaining the scientific integrity and operational efficiency of a trial. It supports various complex randomization schemes, such as stratified and block randomization, to ensure balanced treatment groups across different patient populations. On the supply side, it manages the entire investigational product lifecycle, from depot to site to patient. By using predictive algorithms to forecast demand, the RTSM minimizes drug wastage, prevents stock-outs that could delay patient treatment, and automates re-supply orders, ensuring the right medication is always available for the right patient without compromising the trial’s blind.
Electronic Clinical Outcome Assessment (eCOA/ePRO)
By capturing data directly from the source—the patient (ePRO) or clinician (eCOA)—these tools eliminate the recall bias and transcription errors associated with traditional paper diaries. They can be deployed on provisioned devices or through a more convenient ‘Bring Your Own Device’ (BYOD) model, reducing patient burden. The platform can send automated reminders to patients to complete their entries, leading to higher compliance rates and more complete datasets. This continuous stream of high-quality, real-time patient data provides invaluable insights into treatment efficacy and safety from the patient’s perspective.
eConsent
The eConsent module transforms informed consent from a one-time, paper-based event into an interactive, educational process. By incorporating multimedia elements like videos, animations, and comprehension quizzes, it helps ensure patients truly understand the trial’s procedures, risks, and benefits before providing their signature. It also facilitates remote consenting, allowing patients to review materials at their own pace and discuss them with family members, which can increase trust and willingness to participate. All signed forms and version histories are stored securely within the platform, simplifying audit trails and re-consenting processes when protocols are amended.
Unifying the Trial Lifecycle
The true power of a clinical development platform is its ability to unify the entire trial lifecycle. By replacing disparate systems with an end-to-end workflow, it creates a single source of truth in one integrated environment. This integration and standardization accelerate research and transform how new treatments are brought to market. The future lies in intelligently connecting data, technology, and analytics to solve challenges and develop more patient-centric trials. The integration of advanced technologies like AI is paramount, as it will enable predictive insights and automated decision-making. Future Use of Artificial Intelligence in Clinical Trials will further improve these platforms.
The Unified Advantage: Why Integrated Platforms Outperform Fragmented Systems
Using fragmented systems versus a unified clinical development platform is the difference between a puzzle with missing pieces and a complete picture. Teams using disconnected tools battle data silos, vendor management headaches, and spiraling costs. In contrast, organizations that adopt integrated platforms gain centralized data in harmonized formats, streamlined workflows, and improved data integrity in real-time, avoiding the manual processes and high operational costs of fragmented systems.
| Fragmented Systems | Unified Platforms |
|---|---|
| Siloed data, inconsistent formats | Centralized data, harmonized formats |
| Multiple vendors, complex management | Streamlined workflow, single vendor or integrated suite |
| Integration challenges, data reconciliation issues | Improved data integrity, real-time data flow |
| Higher operational costs, manual processes | Reduced timelines, automated processes |
Accelerating Timelines and Maximizing ROI
A unified clinical development platform makes trials dramatically faster and more profitable. The numbers are compelling: research teams see up to 3x faster study completion timelines, cutting years off development. They also achieve a 30% reduction in data management costs by eliminating manual data transfer and reconciliation. Furthermore, monitoring costs drop by 40% thanks to remote access and real-time oversight, reducing the need for expensive site visits. The overall impact is staggering, with some organizations reducing trial timelines by up to 40% through automation. This culminates in a 13x ROI for Phase III trials as treatments reach the market faster with lower overhead. This efficiency improves quality and safety, as better data integrity leads to better decisions and patient outcomes.
Enhancing the Experience for Sites and Sponsors
Unified platforms significantly improve the experience for everyone involved. For a research site coordinator, juggling multiple systems for EDC, randomization, and patient outcomes is a major burden. A clinical development platform consolidates these tasks into one intuitive interface. This reduced administrative burden allows site staff to focus on patient care and trial quality. As one expert noted, “Minimizing the number of platforms and logins improves usability for sites, encouraging continued collaboration.”
For sponsors and CROs, the benefits include real-time visibility into trial progress to proactively address issues and improved collaboration from working with a single data source. This integrated approach creates a virtuous cycle: happier sites, better data for sponsors, and a smoother patient experience. For deeper insights, check out these insights from an expert on site engagement.
How Technology is Revolutionizing Clinical Development
Technology is rapidly changing medical research, and a modern clinical development platform is central to this shift. These platforms enable new trial models like decentralized (DCTs) and hybrid studies, using smart tech to improve efficiency and patient outcomes. DCTs and hybrid trials bring the study to the patient, reducing the need for clinic visits. This approach uses remote monitoring, digital data collection (eCOA/ePRO), and wearable sensors to gather information continuously. By making participation more convenient and reducing administrative burdens with automated reminders, platforms help more people join and stay in studies.

The Role of AI and Machine Learning in a Clinical Development Platform
Artificial Intelligence (AI) and Machine Learning (ML) are game-changers within a clinical development platform, enabling faster, deeper insights.
- Predictive Analytics: AI analyzes vast datasets to forecast trends, helping design better trials, predict patient enrollment, and identify potential risks early.
- Protocol Optimization: ML reviews historical trial data to suggest protocol improvements, increasing the likelihood of success.
- AI-Assisted Data Review: AI automates the scanning of clinical data, flagging errors and anomalies to ensure cleaner data and reduce manual effort.
- Risk-Based Monitoring: AI identifies high-risk sites or data points, allowing for targeted monitoring that saves time and resources.
- AI-Driven Safety Surveillance: AI monitors for adverse events in real-time, enabling faster detection of safety signals to protect patients.
AI-driven tools are changing clinical trials by extracting critical insights from health data to drive scientific breakthroughs. For more, see these Insights on AI in drug development from Brian Martin, Head of AI at AbbVie.
Ensuring Data Security and Regulatory Compliance
Ensuring data security, accuracy, and regulatory adherence is vital in clinical research. A top-notch clinical development platform is built to meet strict global standards.
Key regulations include:
- GxP (Good Practice guidelines): This umbrella of standards (GCP, GLP, GMP) ensures data and process integrity. A compliant platform provides a validated GxP environment.
- 21 CFR Part 11: This FDA rule governs electronic records and signatures, requiring features like audit trails and access controls to ensure data reliability.
- HIPAA & GDPR: These regulations protect patient privacy in the US (HIPAA) and Europe (GDPR), mandating secure handling of sensitive health information.
- ISO Standards: Certifications like ISO 27001 (information security) demonstrate a commitment to quality and security.
To maintain compliance, platforms use tools like Trusted Research Environments (TREs)—secure digital spaces for data analysis—and Data Provenance, which tracks the history of every data point for auditability. Our platform uses a Trusted Data Lakehouse (TDL) and a Real-time Evidence & Analytics Layer (R.E.A.L.) to provide real-time insights and secure collaboration with precise access controls. For more on regulatory platforms, explore the FDA’s precisionFDA Platform.
Key Considerations for Selecting and Implementing Your Platform
Choosing the right clinical development platform is a critical decision. It’s more than a feature checklist; it’s selecting a partner that will define your trial efficiency, speed to market, and overall success. The best platforms are scalable, user-friendly for all stakeholders, and future-proof.
Top 10 Selection Criteria
When evaluating platforms, we focus on ten critical areas that determine long-term success:
1. Unified vs. Best-of-Breed Architecture
A unified platform with integrated EDC, CTMS, eTMF, and eCOA eliminates vendor management headaches and data silos common with best-of-breed tools.
2. Scalability & Flexibility
The platform must scale from small Phase I studies to large global trials. Customizable modules allow you to tailor the system to each trial’s needs without paying for unused features.
3. Compliance & Security
Non-negotiable. The platform must meet GxP, 21 CFR Part 11, HIPAA, and GDPR standards. Enterprise-grade security, controlled data sharing, and clear audit trails are essential.
4. Stakeholder Experience
A positive user experience for sites and patients is crucial for trial success. The platform should be intuitive, reducing administrative burden so sites can focus on patient care.
5. AI & Analytics Capabilities
Go beyond basic reporting. Look for AI-driven predictive analytics, protocol optimization, and risk-based monitoring to turn data into actionable insights for faster, smarter decisions.
6. Support for DCT/Hybrid Models
The platform must natively support flexible decentralized and hybrid trial models with tools for remote data collection, patient engagement, and wearable integration.
7. Integration & Interoperability
Robust APIs are essential for interoperability, allowing the platform to connect with external systems like EHRs and lab systems to create a comprehensive research ecosystem.
8. Vendor Expertise & Support
Evaluate the vendor’s track record, commitment to customer success, and quality of support. Choose a partner with deep expertise in clinical research, not just software.
9. Total Cost of Ownership
Consider the total cost, including implementation, maintenance, and training. Flexible pricing models that align costs with usage can be more budget-friendly.
10. Future-Proof Technology
Choose a platform with modern architecture that can adapt to emerging trends like multi-omics data and RWE. Ensure it’s a long-term investment ready for future challenges.
Future-Proofing Your Research: Emerging Trends
Your clinical development platform must keep pace with a rapidly evolving research landscape. Key emerging trends include:
- Multi-omic data integration: Combining genomic, proteomic, and other ‘omic’ data with clinical data is essential for precision medicine and biomarker findy.
- Real-World Evidence (RWE): Incorporating data from EHRs and registries is crucial for understanding treatment performance in real-world settings.
- Federated learning: This privacy-preserving AI approach enables collaborative research by training models on distributed data without moving it. Federated data platforms are key to this approach.
- Patient-centric design: Future platforms will evolve beyond data collection to foster true patient partnership through advanced engagement tools.
Our platform is built for these trends, providing secure access to global biomedical and multi-omic data with advanced AI/ML analytics. Our federated governance enables large-scale, compliant research, ensuring you’re ready for the future of clinical research.
Frequently Asked Questions about Clinical Development Platforms
How do clinical development platforms accelerate time-to-market?
Imagine trying to launch a rocket with separate teams managing the fuel, navigation, and launch sequence, all using different communication systems! It would be slow and prone to errors. That’s a bit like traditional clinical trials with fragmented systems.
Clinical development platforms act like a unified mission control. By bringing all trial activities into one place, they help us move much faster. They automate tasks that used to take ages, like data entry or tracking documents. Plus, they use smart tools like AI to analyze data quickly, giving us insights in real-time. This means we can make quicker, better decisions throughout the trial.
All this efficiency can slash trial timelines by up to 40%. Think about it: shaving weeks or even months off a trial means getting life-changing treatments to patients much sooner. It also means significant cost savings, especially when you consider that developing a new drug can take over a decade and cost billions. It’s truly about speeding up the journey from findy to patient care.
What is the difference between a CTMS and a full clinical development platform?
This is a great question, and it’s easy to get them mixed up! Think of it this way:
A CTMS (Clinical Trial Management System) is like the engine of a car. It’s absolutely crucial and keeps things moving by focusing on the operational nuts and bolts. It helps you manage things like site visits, track key milestones, and handle the financial side of a trial. Essential, yes, but it’s just one part of the whole vehicle.
A full clinical development platform, on the other hand, is the entire car, fully loaded and ready to go! It integrates the CTMS engine with all the other vital systems. This means you get Electronic Data Capture (EDC) for collecting data, Electronic Patient-Reported Outcomes (ePRO) for patient input, Electronic Trial Master File (eTMF) for all your documents, and even advanced analytics, all working together seamlessly. It’s one unified solution that gives you a complete, holistic view of your trial, from start to finish. This comprehensive approach ensures all your data is connected, accurate, and easily accessible, providing a “single source of truth” that makes trial management much smoother.
How do these platforms improve patient engagement and retention?
Making clinical trials easier and more appealing for patients is key to their success, and clinical development platforms excel at this. They put the patient experience at the forefront.
Imagine participating in a trial from the comfort of your own home! These platforms often include user-friendly mobile apps that allow patients to submit data conveniently through ePRO/eCOA tools. This means less travel to clinics and more flexibility. They also streamline the consent process with eConsent, making it easier to understand and sign up digitally.
Beyond convenience, platforms keep patients engaged with automated reminders for appointments or data entries, and they can integrate telehealth for virtual consultations. Direct, secure communication tools also foster a stronger connection between patients and study teams. All these features combine to reduce the burden on patients, making participation much more manageable and positive. This can lead to impressive outcomes, with some platform-driven trials reporting an amazing 96.5% study completion rate! When patients feel supported and their experience is seamless, they are much more likely to stay engaged throughout the trial.
Conclusion: Building the Future of Medicine, Together
The change we’re witnessing in clinical research isn’t just about upgrading software—it’s about reimagining how we bring life-saving treatments to patients. Throughout this journey, we’ve seen how clinical development platforms are dismantling the barriers that have historically slowed medical innovation.
Think about where we started: researchers juggling multiple systems, sites drowning in paperwork, and patients struggling to participate in trials that could change their lives. Now picture a world where all these challenges dissolve into seamless, intelligent workflows. That’s the power of unified platforms working in perfect harmony.
The numbers tell an incredible story. Up to 3x faster study completion timelines. 40% reduction in monitoring costs. 13x ROI for Phase III trials. But behind every statistic is something far more meaningful—treatments reaching patients faster, research teams focusing on what truly matters, and hope delivered with unprecedented efficiency.
AI-driven insights are changing how we predict outcomes, optimize protocols, and ensure patient safety. Patient-centricity is no longer just a buzzword—it’s built into every interaction, from mobile-friendly ePRO tools to intuitive eConsent processes that respect people’s time and intelligence. The result? Study completion rates soaring to 96.5% because participation finally feels human.
What excites me most is how these platforms accept the complexity of modern medicine while making it feel simple. Multi-omic data integration, real-world evidence, federated learning—these aren’t distant dreams but realities that clinical development platforms are making accessible today. They’re breaking down data silos and creating collaborative ecosystems where insights flow freely while privacy remains sacred.
At Lifebit, we’ve built our platform around this vision of seamless collaboration. Our Trusted Research Environment (TRE), Trusted Data Lakehouse (TDL), and Real-time Evidence & Analytics Layer (R.E.A.L.) work together to deliver something remarkable: the ability to harness global biomedical data securely, analyze it intelligently, and act on insights immediately.
The future of medicine isn’t just about better technology—it’s about better connections. Between researchers and data. Between sponsors and sites. Between treatments and the patients who need them most. When we intelligently connect data, technology, analytics, and operational expertise, we don’t just solve challenges—we create possibilities that didn’t exist before.
This is how we build the future of medicine, together. Not through isolated efforts or fragmented systems, but through unified platforms that amplify human intelligence and accelerate human healing. Ready to be part of this change? Explore a next-generation federated data platform and find what becomes possible when barriers disappear.


