Medicare and Medicaid Central: Finding Your Way Through CMS

Center for Medicaid and Medicare: Vital 2025 Guide
Understanding America’s Largest Healthcare Administrator
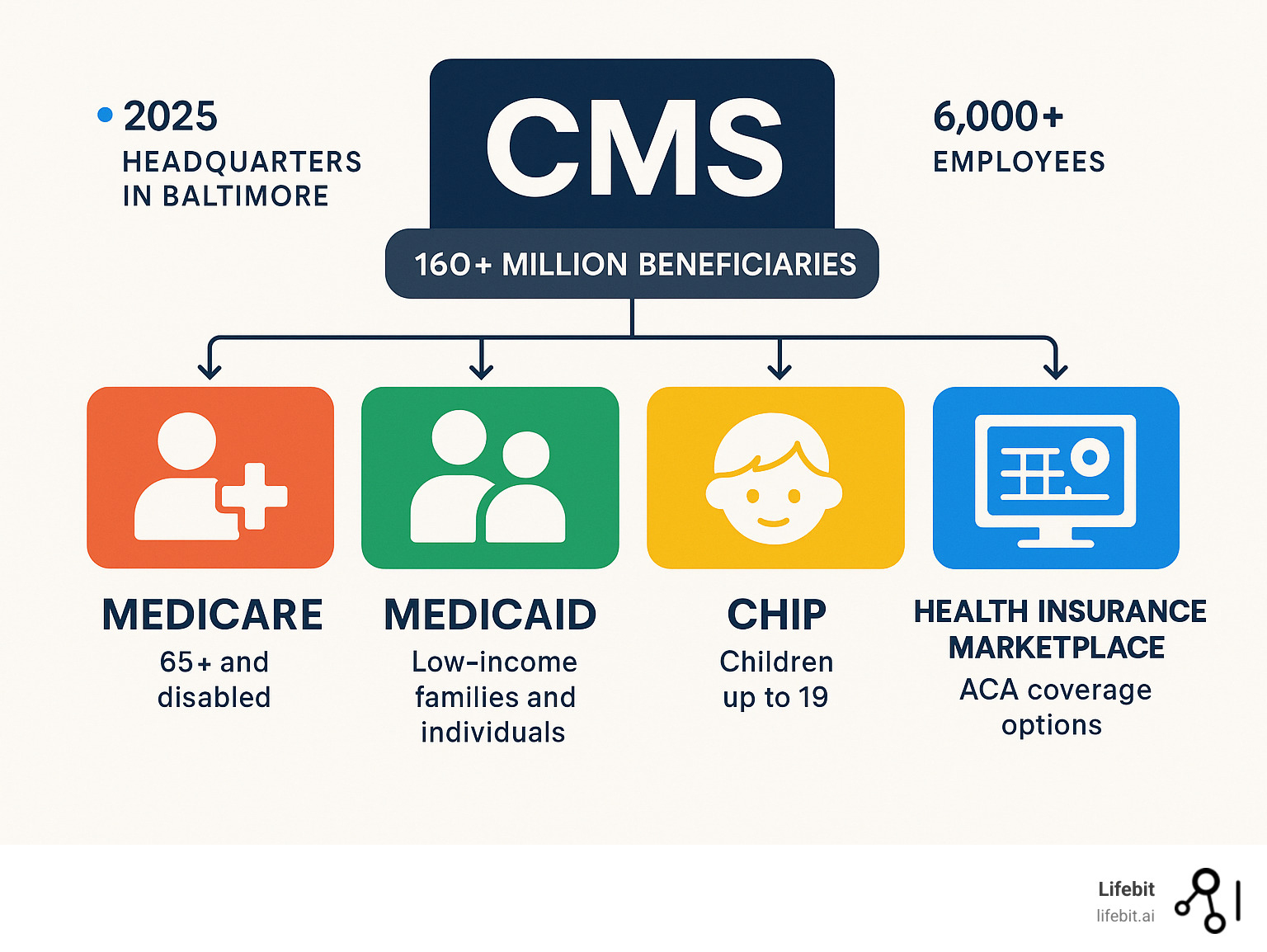
The center for medicaid and medicare, officially the Centers for Medicare & Medicaid Services (CMS), is the federal agency providing health coverage to over 160 million Americans through Medicare, Medicaid, the Children’s Health Insurance Program (CHIP), and the Health Insurance Marketplace.
Quick Facts About CMS:
- Location: 7500 Security Boulevard, Baltimore, MD 21244
- Parent Agency: U.S. Department of Health and Human Services (HHS)
- Employees: Over 6,000 staff members
- Coverage: Serves 160+ million Americans
- Programs: Medicare, Medicaid, CHIP, Health Insurance Marketplace
- Mission: Strengthen and modernize healthcare while providing access to high-quality care at lower costs
As one of the world’s largest purchasers of healthcare, CMS’s role extends beyond insurance. Originally the Health Care Financing Administration (HCFA) from 1977, it was renamed in 2001. Today, it also oversees nursing home quality, manages HIPAA requirements, and drives innovation via the CMS Innovation Center.
For organizations in pharma, public health, and regulation, understanding CMS is crucial. Its vast datasets and frameworks impact research, drug development, and population health.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. With over 15 years in computational biology and health-tech, I’ve seen how the center for medicaid and medicare governs the complex landscape of healthcare data. My experience building secure platforms for biomedical data analysis underscores the critical need to understand CMS’s role in shaping data access and regulatory requirements.
Quick center for medicaid and medicare terms:
The Pillars of CMS: Medicare, Medicaid, and CHIP Explained
The center for medicaid and medicare provides America’s healthcare safety net through its core programs. Each is designed to fill a specific gap in the nation’s health coverage landscape, ensuring access to care for millions, from newborns to seniors.
What is Medicare?
Medicare is the federal health insurance program primarily for people 65 or older. It also provides crucial coverage for younger people with long-term disabilities (after a 24-month waiting period) and individuals with specific severe conditions like End-Stage Renal Disease (ESRD) or Amyotrophic Lateral Sclerosis (ALS), regardless of age.
Medicare is structured into several distinct parts, often referred to as Original Medicare (Parts A and B) and private plan options (Parts C and D).
- Medicare Part A (Hospital Insurance): This part covers inpatient care. Most beneficiaries receive Part A premium-free if they or their spouse paid Medicare taxes for at least 10 years. It helps pay for semi-private rooms, meals, nursing services, and drugs administered as part of inpatient treatment. It also covers care in a skilled nursing facility (following a qualifying hospital stay), hospice care, and home health care.
- Medicare Part B (Medical Insurance): Part B covers a wide range of outpatient services and supplies that are medically necessary to treat a health condition. This includes doctor visits, preventive care (like flu shots and cancer screenings), ambulance services, durable medical equipment (DME), and mental health services. Most people pay a standard monthly premium for Part B, which can be adjusted based on income.
- Medicare Part C (Medicare Advantage): These are all-in-one bundled plans offered by private insurance companies approved by the center for medicaid and medicare. Medicare Advantage plans must cover everything that Original Medicare (Parts A and B) covers. However, they often include additional benefits not covered by Original Medicare, such as routine dental, vision, and hearing care, as well as prescription drug coverage (MAPD plans). Plan types vary, including Health Maintenance Organizations (HMOs) and Preferred Provider Organizations (PPOs), which affect provider networks and costs. Enrollment in Medicare Advantage is growing, with 35.7 million people expected by 2025, as average monthly premiums continue to decrease, making these plans an increasingly affordable and popular choice.
- Medicare Part D (Prescription Drug Coverage): This part helps cover the cost of prescription drugs. It is offered through private insurance companies either as a standalone plan (for those with Original Medicare) or as part of a Medicare Advantage plan. Each plan has its own formulary, or list of covered drugs, which are often organized into tiers that determine copayments.
For comprehensive details on enrollment, costs, and coverage options, Medicare.gov is the official government resource.
What is Medicaid?
Medicaid is a joint federal and state program administered by the center for medicaid and medicare at the federal level. It provides free or low-cost health coverage to millions of Americans, including low-income individuals and families, children, pregnant women, seniors, and people with disabilities.
Unlike Medicare’s age-based eligibility, Medicaid is primarily based on Modified Adjusted Gross Income (MAGI) relative to the Federal Poverty Level (FPL). The Affordable Care Act (ACA) allowed states to expand Medicaid to cover nearly all low-income adults with incomes at or below 138% of the FPL. While most states have adopted this expansion, eligibility rules and covered benefits can vary significantly from state to state because of its unique state partnership model. CMS sets federal guidelines and provides matching funds, but each state designs and administers its own program. All states must cover certain mandatory benefits, such as hospital services, physician services, and laboratory tests, but they can also choose to cover optional benefits like prescription drugs, dental care, and physical therapy.
For detailed information on state-specific programs and federal policies, visit Medicaid.gov.
The Children’s Health Insurance Program (CHIP) and the Marketplace
CHIP was created to fill a crucial coverage gap for children. It provides low-cost health coverage for children up to age 19 in families who earn too much to qualify for Medicaid but cannot afford private insurance. Like Medicaid, CHIP is a federal-state partnership. States can structure their CHIP program as a separate entity, an expansion of their Medicaid program, or a combination of both. It covers essential services like routine check-ups, immunizations, and dental and vision care. To check eligibility for your family, InsureKidsNow.gov is the official resource.
The Health Insurance Marketplace, established by the ACA, serves as a centralized platform where individuals, families, and small businesses can compare and purchase private health insurance plans. The Marketplace is a critical access point, as it also screens applicants for eligibility for Medicaid and CHIP. For those who qualify, the Marketplace offers financial assistance to make coverage more affordable, including Premium Tax Credits to lower monthly payments and Cost-Sharing Reductions to reduce out-of-pocket costs. You can explore all options and apply at Healthcare.gov.
| Program | Primary Beneficiaries | Eligibility Criteria | Key Benefits |
|---|---|---|---|
| Medicare | Seniors (65+), younger people with disabilities | Age, disability status, or specific medical conditions (ESRD, ALS) | Hospital (Part A), medical (Part B), prescription drug (Part D), and managed care plans (Part C) |
| Medicaid | Low-income individuals, families, children, pregnant women, people with disabilities | Income and family size relative to FPL (varies by state) | Comprehensive health benefits, including mandatory and optional services (varies by state) |
| CHIP | Children up to 19 | Families with incomes above Medicaid limits but unable to afford private insurance | Low-cost health coverage for children, including preventive and comprehensive care |
The Evolution and Structure of the Center for Medicaid and Medicare

The history of the center for medicaid and medicare is a story of America’s evolving commitment to public health and healthcare access. From its legislative roots to its modern structure, the agency has continuously adapted to serve the millions who depend on its programs.
From HCFA to CMS: A Brief History
The agency’s origins trace back to the Social Security Act of 1965, signed into law by President Lyndon B. Johnson, which created the Medicare and Medicaid programs. For the first decade, these programs were managed by different federal entities. In March 1977, the federal government consolidated their administration by creating the Health Care Financing Administration (HCFA).
On July 1, 2001, a significant rebranding occurred: HCFA became the Centers for Medicare & Medicaid Services (CMS). This was more than a name change; it signaled a fundamental shift in philosophy. The new name was chosen to reflect a more beneficiary-centered approach and to emphasize the agency’s mission beyond just financing. It highlighted a focus on quality improvement, innovation, and positive patient outcomes. This modernization was further shaped by major legislation, including:
- The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), which introduced Medicare Part D, the prescription drug benefit.
- The Affordable Care Act (ACA) of 2010, which dramatically expanded CMS’s role by creating the Health Insurance Marketplace, allowing for Medicaid expansion, and establishing the CMS Innovation Center.
You can explore more about this history in the historical overview of the agency on the HHS website.
The Core Mission of the Center for Medicaid and Medicare
The mission of today’s center for medicaid and medicare is to strengthen and modernize the nation’s healthcare system while providing access to high-quality care at lower costs. This mission is driven by four key pillars:
- High-quality care: CMS ensures safe, effective, and patient-centered treatment by implementing quality reporting programs, such as the Hospital Inpatient Quality Reporting (IQR) Program, which ties payment to performance on specific quality measures.
- Lower costs: The agency focuses on creating a more efficient healthcare system by reducing administrative burdens and promoting innovative payment models, like value-based purchasing, that reward providers for better outcomes and cost-effectiveness rather than just the volume of services.
- Health equity: A central focus is addressing systemic disparities in healthcare. Through its Framework for Health Equity, CMS works to close gaps in care based on race, income, disability, and geography by improving data collection and implementing targeted policies.
- Access to care: CMS is dedicated to removing barriers to coverage. This involves simplifying enrollment processes, conducting outreach to underserved communities, and ensuring that eligible individuals can easily connect with and use their benefits.
As a major division of the U.S. Department of Health and Human Services (HHS), CMS leverages its position as one of the world’s largest purchasers of healthcare to drive meaningful change across the industry.
How CMS is Organized
The center for medicaid and medicare is a massive organization, managing healthcare for over 160 million Americans from its Baltimore headquarters with a staff of over 6,000 employees. Its operational reach is extended through ten regional offices across the U.S. These offices are crucial for bridging federal policy with local implementation, working directly with state governments, healthcare providers, and beneficiaries.
The agency’s internal structure is organized into several core components, each with distinct responsibilities:
- The Center for Medicare manages all aspects of the Medicare program. This includes setting payment policies (like the annual Physician Fee Schedule), overseeing Medicare Advantage and Part D plans, and managing quality standards for providers.
- The Center for Medicaid and CHIP Services (CMCS) oversees the federal-state partnerships for Medicaid and CHIP. It reviews and approves State Plan Amendments (SPAs) and waivers (such as Section 1115 demonstration waivers) that allow states to test innovative approaches to care delivery and financing.
- The Center for Program Integrity (CPI) is dedicated to combating fraud, waste, and abuse across all CMS programs. It uses advanced data analytics to detect suspicious billing patterns and coordinates with law enforcement to protect taxpayer dollars.
- The CMS Innovation Center (CMMI), established by the ACA, serves as the agency’s engine for research and development. It designs, tests, and evaluates new payment and service delivery models aimed at improving care quality and lowering costs.
This structure enables CMS to manage its vast and complex responsibilities, balancing the need for national standards with the flexibility required for effective state-level program administration.
Beyond Coverage: CMS’s Role in Quality, Safety, and Innovation

The center for medicaid and medicare‘s influence extends far beyond providing health insurance coverage. The agency is a primary force in setting national standards for healthcare quality, ensuring patient safety, combating fraud, and driving systemic innovation.
Ensuring Quality of Care and Patient Safety
CMS acts as a quality and safety regulator for the U.S. healthcare system, ensuring that providers participating in its programs meet stringent standards. Key efforts include:
- Nursing Home Oversight: CMS’s Five-Star Quality Rating System is a critical tool for consumers. It rates facilities on a one-to-five-star scale based on three domains: health inspections from on-site surveys, staffing levels (including registered nurse hours per resident), and a set of clinical quality measures. Persistently underperforming facilities may be designated as Special Focus Facilities, subjecting them to more frequent inspections and enforcement actions.
- Clinical Laboratory Improvement Amendments (CLIA): CMS regulates all laboratory testing performed on humans in the U.S. through the CLIA program. This ensures the accuracy, reliability, and timeliness of test results, regardless of where the test is performed. Laboratories must obtain a specific CLIA certificate (e.g., Certificate of Waiver for simple tests or Certificate of Compliance for complex tests) based on the complexity of their testing, which is crucial for preventing misdiagnoses.
- Provider Certification: For a facility like a hospital, home health agency, or dialysis center to receive payment from Medicare and Medicaid, it must be certified as meeting federal health and safety standards known as Conditions of Participation (CoPs) or Conditions for Coverage (CfCs). State survey agencies conduct these certification surveys on behalf of CMS, acting as a seal of approval that signifies a baseline of quality and safety.
Tackling Fraud, Waste, and Abuse
Healthcare fraud costs taxpayers billions of dollars annually and diverts critical resources from patient care. The center for medicaid and medicare employs a multi-pronged strategy to protect its programs:
- Fraud Prevention and Education: CMS educates beneficiaries on how to protect their Medicare information and recognize potential scams. Beneficiaries are encouraged to report suspicious activity to the fraud hotline at 1-800-447-8477. Common fraud schemes include billing for services never rendered, upcoding (billing for a more expensive service than was provided), and offering illegal kickbacks for patient referrals.
- Program Integrity and Data Analytics: The Center for Program Integrity (CPI) uses sophisticated data analysis and predictive modeling to identify unusual billing patterns and high-risk providers. It deploys Unified Program Integrity Contractors (UPICs) to conduct proactive data analysis and investigations to stop fraud before payments are made.
- Recovery Efforts: When fraud or improper payments are identified, CMS works aggressively to reclaim funds. This includes the use of Recovery Audit Contractors (RACs), who are tasked with reviewing claims post-payment to identify and recover overpayments made to providers, ensuring the financial sustainability of the programs.
Key Initiatives from the Center for Medicaid and Medicare
CMS is constantly evolving its policies and programs to improve the healthcare system:
- Value-Based Care Models: The CMS Innovation Center is at the forefront of shifting healthcare from a fee-for-service system (which rewards volume) to one that rewards value and outcomes. Key models include Accountable Care Organizations (ACOs), where groups of providers coordinate care for patients and share in savings, and Bundled Payments for Care Improvement (BPCI), which provides a single, comprehensive payment for all services related to an episode of care, like a knee replacement.
- Price Transparency: CMS has implemented landmark rules to empower consumers. The Hospital Price Transparency Rule requires hospitals to post their standard charges in a machine-readable file and a consumer-friendly format. Similarly, the Transparency in Coverage Rule requires health plans to disclose pricing data, creating unprecedented visibility into healthcare costs to foster competition and informed decision-making.
- Health Equity Initiatives: CMS is actively working to embed health equity into all its programs. This includes developing quality measures that capture health disparities, improving the collection of demographic data, and launching initiatives to address the social determinants of health that impact patient outcomes.
In all these initiatives, protecting patient privacy is paramount. CMS must balance the use of vast datasets for research and oversight with the need to preserve patient data privacy, maintaining public trust as it works to advance public health.
Navigating CMS: Key Resources and How to Get Help
Navigating the vast landscape of the center for medicaid and medicare can be straightforward with the right resources. CMS offers a comprehensive suite of tools and information portals for beneficiaries, providers, researchers, and states.
Top Online Resources for Beneficiaries and Providers
The Official CMS Website serves as the central hub for all information related to Medicare, Medicaid, CHIP, and the Health Insurance Marketplace. It offers everything from high-level policy announcements to detailed technical guidance.
- For Beneficiaries: Dedicated portals like Medicare.gov, Medicaid.gov, and InsureKidsNow.gov are designed to help individuals and families understand their benefits, check eligibility, compare plans, and complete enrollment.
- For Healthcare Providers: The CMS website provides essential technical resources to ensure compliance and proper billing. This includes access to program manuals, fee schedules, reimbursement codes, and coverage determinations. Providers rely on National Coverage Determinations (NCDs) and Local Coverage Determinations (LCDs) to understand which services are considered medically necessary and will be reimbursed.
- For Marketplace Partners: A dedicated resource section supports agents, brokers, and navigators who assist with enrollment, reflecting CMS’s commitment to supporting Federal Health initiatives through strong public-private partnerships.
How to Contact CMS
For direct assistance, CMS provides several clear points of contact:
- For general questions about Medicare, call the toll-free number 1-800-MEDICARE (1-800-633-4227).
- To report suspected Medicare fraud, waste, or abuse, use the dedicated hotline at 1-800-HHS-TIPS (1-800-447-8477).
- For official correspondence, the main address is: Office of External Affairs, 7500 Security Blvd., Baltimore, MD 21244. Regional offices primarily serve as liaisons for state governments and large provider organizations.
Understanding Data, Technology, and HIPAA
The center for medicaid and medicare is a data-driven organization that leverages technology for oversight, research, and quality improvement.
- Data Utilization and Research: CMS manages one of the largest and most valuable health data repositories in the world. To facilitate research, it provides secure access to de-identified data files through resources like the CMS Virtual Research Data Center (VRDC). Researchers can analyze claims data (inpatient, outpatient, Part D) and beneficiary summary files to study care patterns, costs, and outcomes. This data is foundational for evidence-based policymaking.
- HIPAA Administrative Simplification: A key responsibility of CMS is the implementation and enforcement of the Health Insurance Portability and Accountability Act (HIPAA) Administrative Simplification provisions. These rules standardize electronic health transactions and protect sensitive health information. The key components include:
- The Privacy Rule: Establishes national standards to protect individuals’ medical records and other individually identifiable health information (Protected Health Information, or PHI). It sets limits and conditions on the uses and disclosures that may be made without patient authorization.
- The Security Rule: Establishes national standards to protect electronic personal health information (ePHI). It requires covered entities to implement administrative, physical, and technical safeguards (e.g., access controls, encryption, risk analysis) to ensure the confidentiality, integrity, and security of ePHI.
- The Breach Notification Rule: Requires covered entities to provide notification to affected individuals and HHS following a breach of unsecured PHI.
Data security remains a constant challenge, as highlighted by a 2018 data breach. This incident underscores the critical need for robust cybersecurity measures when handling health data and the importance of secure platforms like a Trusted Research Environment to enable vital research while ensuring Data security in health research. CMS’s commitment to responsible data stewardship is essential for driving improvements across the healthcare system while maintaining public trust.
Frequently Asked Questions about CMS
Here are answers to common questions about the center for medicaid and medicare.
What was CMS previously called?
From its creation in 1977 until 2001, the agency was called the Health Care Financing Administration (HCFA). The 2001 renaming to CMS reflected an expanded, more beneficiary-focused mission and a shift toward modernization. When reviewing older documents, HCFA is the former name for CMS.
How does CMS work with state governments?
The center for medicaid and medicare partners with state governments for Medicaid and CHIP. CMS sets the federal framework, providing guidelines and funding, while each state administers its own program, defining specific eligibility and benefits within federal rules. This creates a system that balances national consistency with local flexibility. CMS ensures compliance through data reviews and technical assistance.
What is the CMS Innovation Center?
Established by the Affordable Care Act, the CMS Innovation Center develops and tests new healthcare payment and service delivery models. Its mission is to improve patient care, reduce costs, and promote healthier communities. The center explores approaches like value-based care and targeted programs, such as the GUIDE Model for dementia care. It focuses on evidence-based results, carefully testing and measuring models before broader implementation. For organizations working with complex health data, the Innovation Center’s work provides key insights into implementing new technologies safely and effectively.
Conclusion
The center for medicaid and medicare is the backbone of America’s healthcare system, providing coverage to over 160 million Americans while ensuring quality, preventing fraud, and driving innovation.
From its origins to today’s value-based care models, CMS has evolved to meet the needs of American families. The center for medicaid and medicare meaningfully impacts seniors, families, and providers alike.
The agency’s mission to strengthen and modernize healthcare with high-quality care at lower costs is a commitment with real-world impact, seen when patients receive care through Medicare, CHIP, or in safer nursing homes due to CMS oversight.
Empowering beneficiaries is central to CMS’s work, achieved through online resources, helplines, and state partnerships. The CMS Innovation Center also tests new healthcare approaches.
For organizations in pharma and public health, understanding CMS is essential. Its datasets and frameworks directly impact research, drug development, and improving health outcomes across the healthcare ecosystem.
As healthcare becomes increasingly data-driven, the need for secure, compliant platforms that can handle large-scale analysis becomes critical. For organizations facing these intricate challenges with health data, Lifebit’s federated platform offers secure and compliant solutions for large-scale analysis and collaboration, enabling the kind of real-time insights that can accelerate findies and improve patient outcomes.

