Electronic Health Records 101—Everything You Need to Know

EHRs 101: The Ultimate Guide to Better Care
Why EHRs Are Changing Modern Healthcare
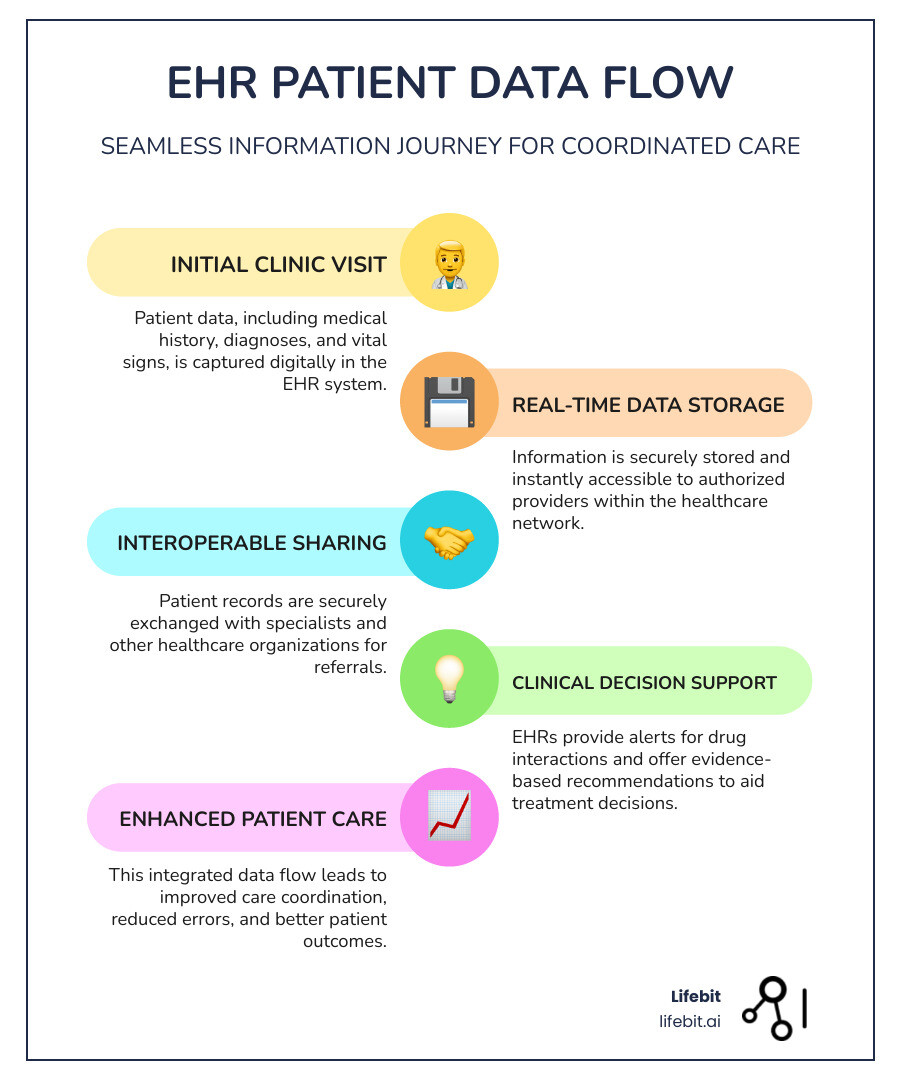
EHRs (Electronic Health Records) are digital versions of a patient’s paper chart, containing their complete medical history, diagnoses, medications, and lab results. Unlike paper records, EHRs allow for real-time data sharing across different healthcare providers, which improves care coordination and patient outcomes.
Key aspects of EHRs:
- Digital patient records replacing paper charts
- Real-time access to patient information
- Comprehensive data including demographics, medications, and test results
- Interoperability for secure sharing between providers
- Clinical decision support with alerts and recommendations
The healthcare industry has seen a massive digital change, with EHR adoption in the U.S. jumping from 10% in 2008 to 96% today. This shift is more than just going paperless; EHRs are fundamentally changing healthcare delivery by centering care decisions around patient data.
Fully implemented EHRs create a complete picture of a patient’s health journey, enabling providers to make faster, more accurate decisions while reducing medical errors. For organizations, this means improved efficiency, better patient safety, and the ability to demonstrate quality outcomes. This is crucial, as over 30% of Medicare payments ($117B annually) are now tied to clinical quality metrics.
As CEO and Co-founder of Lifebit, I’ve seen how EHRs generate massive amounts of health data that can transform patient care through advanced analytics and AI. My experience has shown the critical importance of making this data accessible for research while maintaining the highest security and compliance standards.
Essential EHRs terms:
What Are Electronic Health Records (EHRs)?
EHRs are the digital evolution of paper files, but they are much more than computerized charts. Electronic Health Records are real-time, patient-centered digital records that make health information instantly and securely available to authorized users, regardless of location or provider.
When you visit your family doctor, a specialist, and an emergency room, your EHR travels with you. It’s a comprehensive, secure digital biography of your health that follows you throughout your medical journey, creating a single, longitudinal record of all your health events.
EHR vs EMR: Understanding the Difference
You’ve likely heard EHR and EMR used interchangeably, but they have a key difference. An Electronic Medical Record (EMR) is a digital version of a chart in a single doctor’s office. It contains your medical and treatment history from that specific practice and is used for diagnosis and treatment within that clinic’s walls. It is not designed to be easily shared with outside providers.
An Electronic Health Record (EHR) is a universal health passport. It gathers information from all healthcare providers involved in your care—your family doctor, specialists, hospitals, labs, and pharmacies. This means a new specialist can immediately access your recent lab work from one facility and X-rays from another, creating a holistic view of your health.
There is also a Personal Health Record (PHR), which is a health management tool that you, the patient, control directly. Unlike EHRs, which are created and managed by healthcare providers, a PHR allows you to compile, maintain, and share your own health information. You might use a PHR to track your blood sugar readings, log your medications, or share your fitness data with your doctor. While some PHRs can connect to a provider’s EHR, they are fundamentally patient-driven tools designed to promote engagement in one’s own healthcare.
| Feature | Electronic Medical Record (EMR) | Electronic Health Record (EHR) |
|---|---|---|
| Scope | Digital version of paper charts within a single practice/clinic | Broader view of patient’s health across multiple organizations/providers |
| Information | Notes and information collected by a specific provider/clinic | Comprehensive data from all clinicians involved in a patient’s care |
| Sharing | Limited sharing, primarily internal to the practice | Designed for seamless sharing across various healthcare providers and settings |
| Primary Use | Used by providers for diagnosis and treatment within their setting | Supports coordinated, integrated care across the healthcare ecosystem |
| Portability | Not easily portable | Follows the patient across different healthcare settings and locations |
What Information is in an EHR?
Your EHR is a detailed story of your health journey, containing everything from basic details to complex medical data. A robust EHR includes:
- Patient identifiers and demographics: The foundational data, including name, birth date, contact information, age, gender, and preferred language.
- Diagnoses and problem lists: A snapshot of current and past health issues, coded using international standards like ICD-10 (International Classification of Diseases) for billing and epidemiology, and SNOMED CT (Systematized Nomenclature of Medicine—Clinical Terms) for detailed clinical documentation.
- Medication records: A complete list of all prescriptions, over-the-counter drugs, and supplements. This includes dosages, administration instructions, and start/end dates. This function is critical for medication reconciliation, the process of comparing a patient’s medication orders to all of the medications that the patient has been taking to avoid errors.
- Lab results and vital signs: Captures all diagnostic test results (e.g., blood tests, pathology reports) and measurements from each visit (e.g., blood pressure, heart rate, weight, BMI).
- Procedure data: Documents all surgeries, medical tests, and procedures performed, including dates, providers, and outcomes.
- Patient-generated health data (PGHD): Information shared by patients from personal devices is increasingly included. This can range from blood sugar readings from a continuous glucose monitor, blood pressure readings from a home cuff, or activity levels from a fitness tracker.
- Social Determinants of Health (SDoH): Non-medical factors that affect health outcomes are now being captured. This includes data on housing stability, food security, transportation access, and social support, giving providers a more complete context for a patient’s health.
- Other critical data: Your EHR also holds records of immunizations, allergies, radiology images (X-rays, MRIs), clinical notes from providers, and billing information.
Core Functionalities of an EHR System
Modern EHR systems are sophisticated digital ecosystems that support every aspect of healthcare delivery.
- The Clinical Information System (CIS) is the backbone, ensuring real-time information flows between departments and hospitals.
- Computerized Provider Order Entry (CPOE) allows providers to enter prescriptions, lab tests, and radiology orders directly into the computer. This eliminates handwriting errors and integrates with other systems to immediately transmit the order to the correct department (e.g., pharmacy, lab).
- Clinical Decision Support (CDS): This is one of the most powerful features. CDS systems provide real-time, evidence-based recommendations to clinicians at the point of care. Examples include automated alerts for dangerous drug-drug interactions, reminders for necessary cancer screenings, or checklists to ensure adherence to clinical guidelines for treating conditions like sepsis.
- The Drug Information System (DIS) acts as a vigilant pharmacist, managing your medication profile and checking for potential allergies, incorrect dosages, or harmful interactions.
- The Picture Archive and Communication System (PACS) handles digital storage, retrieval, and sharing of medical images like X-rays, CT scans, and MRIs, allowing specialists to view them from any location.
- Client registries ensure you’re correctly identified throughout the system using a unique patient identifier, preventing dangerous mix-ups.
- Patient portals give you direct, 24/7 access to your health information. Through a secure portal, you can view lab results, review visit summaries, schedule appointments, request prescription refills, pay bills, and communicate securely with your care team. Many portals also offer proxy access for parents or caregivers.
- Integrated billing and coding systems automatically capture information from a clinical visit to generate accurate bills and insurance claims, reducing administrative work and improving revenue cycle management.
At Lifebit, we’ve seen how these comprehensive EHR systems generate valuable health data that can transform patient care through advanced analytics and AI, all while maintaining the highest security and privacy standards.
The Transformative Impact of EHRs on Healthcare
The widespread adoption of EHRs has been revolutionary, moving healthcare from scattered paper files to an interconnected system where patient information flows seamlessly. This isn’t just about going digital; it’s about fundamentally changing care delivery.
The impact is remarkable. Patient safety has improved as medical errors decrease. Care coordination between providers is smoother than ever. Organizations run more efficiently, leading to cost reductions. Most importantly, providers can make evidence-based decisions with complete, up-to-date information.
What’s most exciting is how EHRs have shifted healthcare to a truly patient-centered approach. A cardiologist can instantly see what a family doctor prescribed, and an ER physician has immediate access to allergy information. This level of coordination was impossible with paper records.

How Do EHRs Improve Patient Safety?
EHRs have made healthcare dramatically safer by providing comprehensive, real-time information that helps prevent medical errors.
- Legible documentation eliminates the risk of misreading handwritten prescriptions or notes.
- Accurate patient information, including medical history and allergies, is instantly available at the point of care.
- Reduced duplication of tests occurs when recent lab results are accessible, saving patients time and money while reducing unnecessary procedures.
- Safer prescribing is a major leap. EHRs check for potential allergies, drug interactions, and dosage errors automatically.
- Clinical alerts and reminders prompt providers about necessary screenings or flag concerning lab values, helping prevent small issues from becoming serious.
- Improved diagnostics result from providers having a complete health picture, allowing them to spot patterns that might otherwise be missed. Scientific research on medication error prevention highlights how significant these safety improvements are.
Enhancing Care Coordination and Efficiency
Beyond safety, EHRs have revolutionized how healthcare teams collaborate, ending the days of phone tag and faxing records.
- Real-time data access allows an ER physician to instantly see a patient’s medications and conditions, leading to faster, more accurate care.
- Seamless information exchange means a patient’s hospital discharge summary is immediately available to their family doctor, eliminating the need to repeat medical histories.
- Reduced administrative tasks result from automated coding and billing, freeing up more time for patient care.
- Streamlined workflows improve efficiency, as orders flow directly to labs and pharmacies, and results return automatically.
- Improved provider communication happens when everyone accesses the same comprehensive record, ensuring the entire care team works toward the same goals.
- Better management of chronic conditions like diabetes is possible through continuous monitoring, allowing providers to track trends and adjust treatments proactively.
EHRs have transformed healthcare from a collection of disconnected providers into a coordinated team focused on patient health outcomes.
Implementation, Interoperability, and Security
The journey to implementing EHRs has been challenging. While the benefits are clear, getting these complex systems running and communicating securely requires navigating significant problems. It involves asking entire organizations to fundamentally change long-standing workflows, often while providing critical care. Successfully managing this transition is as much about people and processes as it is about technology.
Key Challenges in Adopting EHRs
Implementing EHRs presents real challenges that require careful planning and management.
- Financial investment: The upfront costs for software licenses, hardware upgrades, implementation support, and data conversion are substantial. For smaller practices, this can be a prohibitive barrier without financial incentives or careful budgeting.
- Clinician burden and workflow disruption: The transition period can be intense. Many providers report increased stress and longer hours as they learn a new system. Poorly designed EHRs can lead to “physician burnout,” characterized by excessive clicking, cumbersome interfaces, and “alert fatigue” from too many non-critical notifications. This often results in “pajama time,” where clinicians spend hours after work completing documentation.
- Data migration: Moving decades of patient information from paper charts or older, disparate electronic systems into a new EHR is a massive undertaking. This process, known as ETL (Extract, Transform, Load), is complex and requires meticulous planning to map data fields correctly and ensure data integrity is not compromised.
- Lack of standardization: Healthcare environments are diverse. An EHR designed for a primary care setting may be a poor fit for a highly specialized field like oncology or ophthalmology, which have unique workflow and data requirements. This has led to the development of specialty-specific EHR modules.
- Training and Change Management: Effective implementation goes beyond a one-day training session. It requires a robust change management strategy to address staff anxiety and resistance. Continuous training, ongoing support, and the identification of internal “super-users” or champions are critical for long-term adoption and success.
The Critical Role of Interoperability and Security
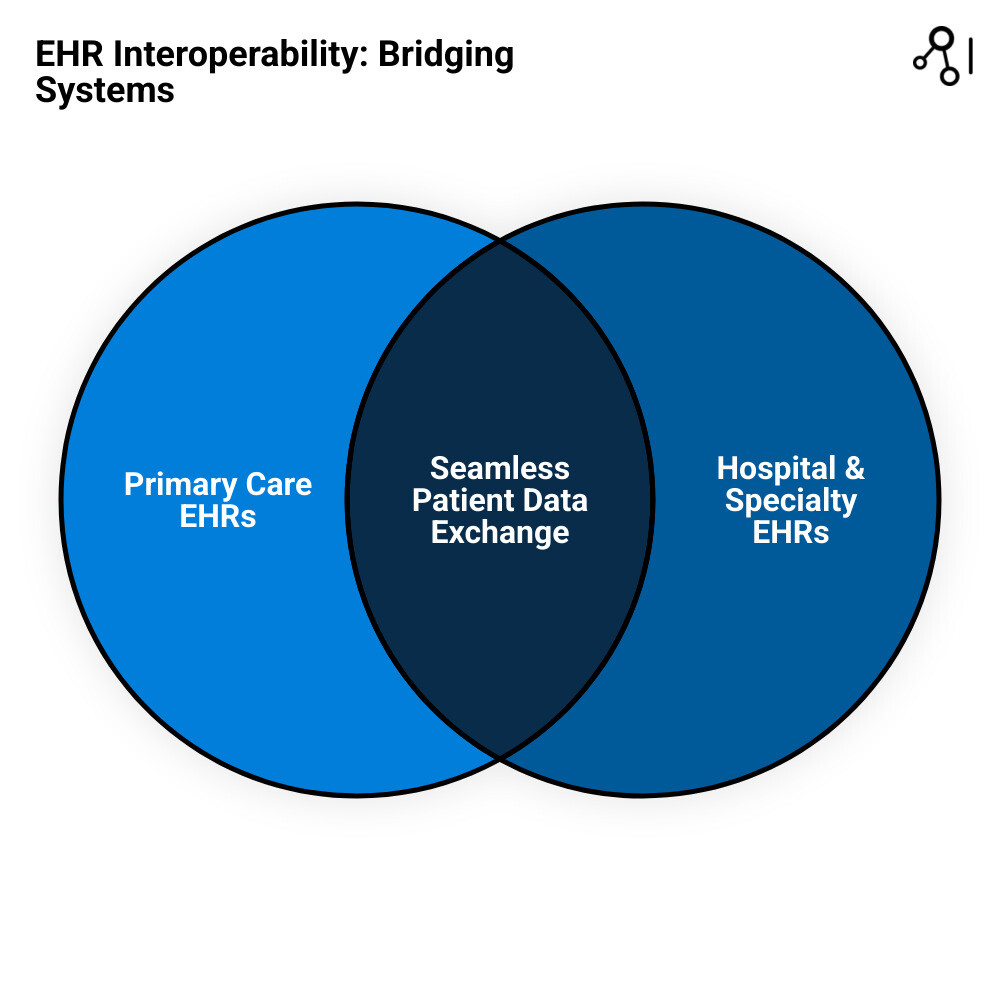
The true power of EHRs is realized only when different systems can share information seamlessly and securely. This is the challenge of interoperability and security.
- Health Information Exchange (HIE): These networks act as the digital backbone for connectivity, allowing different healthcare organizations within a region or state to securely share clinical and administrative data.
- Data standards like HL7 and FHIR: These standards provide a common language for different EHR systems. Health Level Seven International (HL7) has long provided standards for exchanging clinical data. The newer Fast Healthcare Interoperability Resources (FHIR) standard is a game-changer. It is based on modern web technologies and uses APIs (Application Programming Interfaces) to allow for more granular, flexible, and real-time data access. FHIR is what enables third-party apps, like those on a smartphone, to securely connect to an EHR and pull specific health data with patient consent.
- Secure data sharing: Contrary to some beliefs, digital systems can be far more secure than paper records. EHRs create detailed audit trails that log who accessed patient information, what they viewed, and when. This level of tracking is impossible with a paper file.
- HIPAA compliance: In the U.S., the Health Insurance Portability and Accountability Act (HIPAA) sets the standard for protecting sensitive patient health information. The HIPAA Privacy Rule dictates who can access and share data, while the HIPAA Security Rule mandates specific technical, physical, and administrative safeguards that organizations must implement to protect electronic health information.
- Patient consent: Patients must maintain control over their health information. EHR systems and HIEs must have clear policies and technical controls to ensure data is shared only with appropriate consent, except in specific situations like public health reporting or emergencies.
- Preventing unauthorized access: Healthcare is a prime target for cyberattacks. EHR systems use multi-layered security to guard against threats like ransomware and phishing. This includes data encryption (both in transit and at rest), multi-factor authentication, strict access controls, and regular security audits. The 21st Century Cures Act further promotes data sharing for patient access and interoperability while reinforcing these strict privacy and security requirements.
Achieving seamless interoperability while maintaining bulletproof security is an ongoing challenge, but it’s essential for creating a truly connected healthcare system. You can find more info about U.S. government interoperability standards to dive deeper into these technical standards.
The Power of EHR Data in Research and Public Health
The vast amount of health information in EHRs is revolutionizing medical research and public health. This digital goldmine of real-world data, previously locked in filing cabinets, is opening new doors for healthcare findy.

EHR data is powerful because it reflects what happens when real patients receive treatments in everyday clinical practice. This “real-world evidence” (RWE) is invaluable for understanding how treatments work across diverse populations, not just the carefully selected participants in a traditional clinical trial. Public health officials can now spot disease outbreaks faster, track vaccination rates in near real-time, and identify health disparities between different demographic groups. During the COVID-19 pandemic, EHR data was essential for understanding the virus’s risk factors, tracking its spread, and evaluating vaccine effectiveness in the general population.
Utilizing EHRs for Patient Registries and Research
EHRs have transformed how researchers conduct studies, making the process faster and more efficient while protecting privacy.
- Secondary data use: Information collected for routine patient care can be repurposed to answer critical research questions about disease patterns, treatment effectiveness, and long-term outcomes.
- Identifying research cohorts: Researchers can use EHRs like a powerful search engine to quickly and accurately find patients with specific conditions, demographics, or lab values for their studies, dramatically accelerating recruitment.
- Clinical trials: EHR integration helps match patients to appropriate clinical trials more accurately. It can also streamline data collection during a trial, reducing the burden on both patients and researchers.
- Genome-wide association studies (GWAS): By linking health outcomes documented in EHRs with genetic data from biobanks, researchers can uncover connections between specific genes and diseases on a massive scale.
- Real-world evidence: EHRs are the primary source for generating RWE on how treatments perform outside of controlled clinical trials, which is crucial for regulatory decisions and understanding long-term safety and effectiveness.
Overcoming Data Quality and Ethical Problems
While the potential is immense, using EHR data for research requires navigating significant challenges.
- Data Quality Challenges: EHR data is collected for care, not research, which can lead to inconsistencies. A major hurdle is the vast amount of unstructured data locked in clinical notes. Extracting meaningful information from this text requires advanced Natural Language Processing (NLP) techniques. Other issues include missing data, variability in coding practices between institutions, and data entry errors.
- Ethical and Privacy Frameworks: Protecting patient privacy is paramount. Researchers typically work with de-identified or anonymized data, where all personal identifiers are removed. The process is governed by strict ethical guidelines and oversight from Institutional Review Boards (IRBs), which must approve any research using patient data. Informed consent for secondary data use is a complex and evolving area, with models ranging from specific consent for each study to broader consent for future research.
You can find more info about using EHRs for research.
Future Trends in EHR Technology
The future of EHRs is exciting, as they evolve from passive data repositories to active, intelligent partners in care.
- Artificial intelligence and machine learning (AI/ML) are being integrated to analyze patterns in EHR data. This can help predict a patient’s risk of developing a condition like sepsis, forecast hospital readmissions, or identify patients who might respond best to a particular therapy.
- Natural Language Processing (NLP) and Voice Technology: To combat clinician burnout, EHRs are incorporating NLP and voice recognition. This allows doctors to dictate their notes naturally, with the system automatically extracting structured data. NLP also open ups the research value of decades of unstructured clinical notes.
- Hyper-personalization and Precision Medicine: The ultimate goal is to connect EHR data with genomic and other ‘omic’ data. This will allow for true precision medicine, where treatments for diseases like cancer can be custom to an individual’s unique genetic makeup and lifestyle, all documented within the EHR.
- Digital twins, virtual models of individual patients created from their EHR data, could allow doctors to simulate the effects of different treatments before prescribing them, personalizing care to an unprecedented degree.
- Mobile health integration allows providers to access patient information securely on smartphones and tablets, enabling care anywhere. This also includes better integration of patient-generated health data from wearables and home monitors, creating a more continuous and complete health picture.
- Global initiatives like the European Health Data Space (EHDS) Regulation aim to create frameworks for seamless health data sharing across borders to advance global health research and patient care.
At Lifebit, our federated AI platform enables secure analysis of EHR data across organizations without compromising privacy, allowing researchers to gain insights from larger datasets while maintaining top-tier security.
The future promises EHRs that are intelligent partners in healthcare, actively contributing to better health outcomes.
Conclusion
We’ve journeyed through EHRs and seen how these digital systems have transformed modern healthcare. We’ve evolved from scattered paper charts to interconnected systems that prioritize patient safety and care coordination.
As we’ve finded, EHRs have revolutionized patient safety by eliminating handwriting errors and preventing dangerous drug interactions. They improve care coordination by breaking down silos between providers, enabling real-time data sharing that follows patients everywhere. The efficiency gains are equally impressive, with streamlined workflows and reduced administrative burdens freeing up more time for patient care.
Most excitingly, the rich data EHRs collect is fueling groundbreaking research, improving population health management, and accelerating clinical trials.
The future of healthcare is connected and data-driven. As AI and machine learning advance, EHRs will evolve from record-keeping systems into intelligent partners that predict health risks and suggest personalized treatments. This technology strengthens the relationship between patients and care teams, paving the way for future medical breakthroughs.
At Lifebit, we recognize that open uping the full potential of this vast EHR data requires secure, real-time access combined with advanced analytics that respect privacy while enabling findy. Our next-generation federated AI platform is designed to bridge this gap, providing secure access to global biomedical data with built-in harmonization, advanced AI/ML analytics, and federated governance. We are committed to powering large-scale, compliant research, delivering real-time insights and secure collaboration across data ecosystems.
The change of healthcare through EHRs is just the beginning. As we continue to innovate, we’re reimagining what’s possible when technology, data, and human compassion work together.

