Beyond the Numbers: Advanced Analytics for Better Healthcare Outcomes

Cut Unanticipated Deaths 26%—And Costs: The Advanced Analytics Hospitals Ignore
Advanced analytics healthcare is changing how hospitals, researchers, and health systems deliver care. Here’s what you need to know:
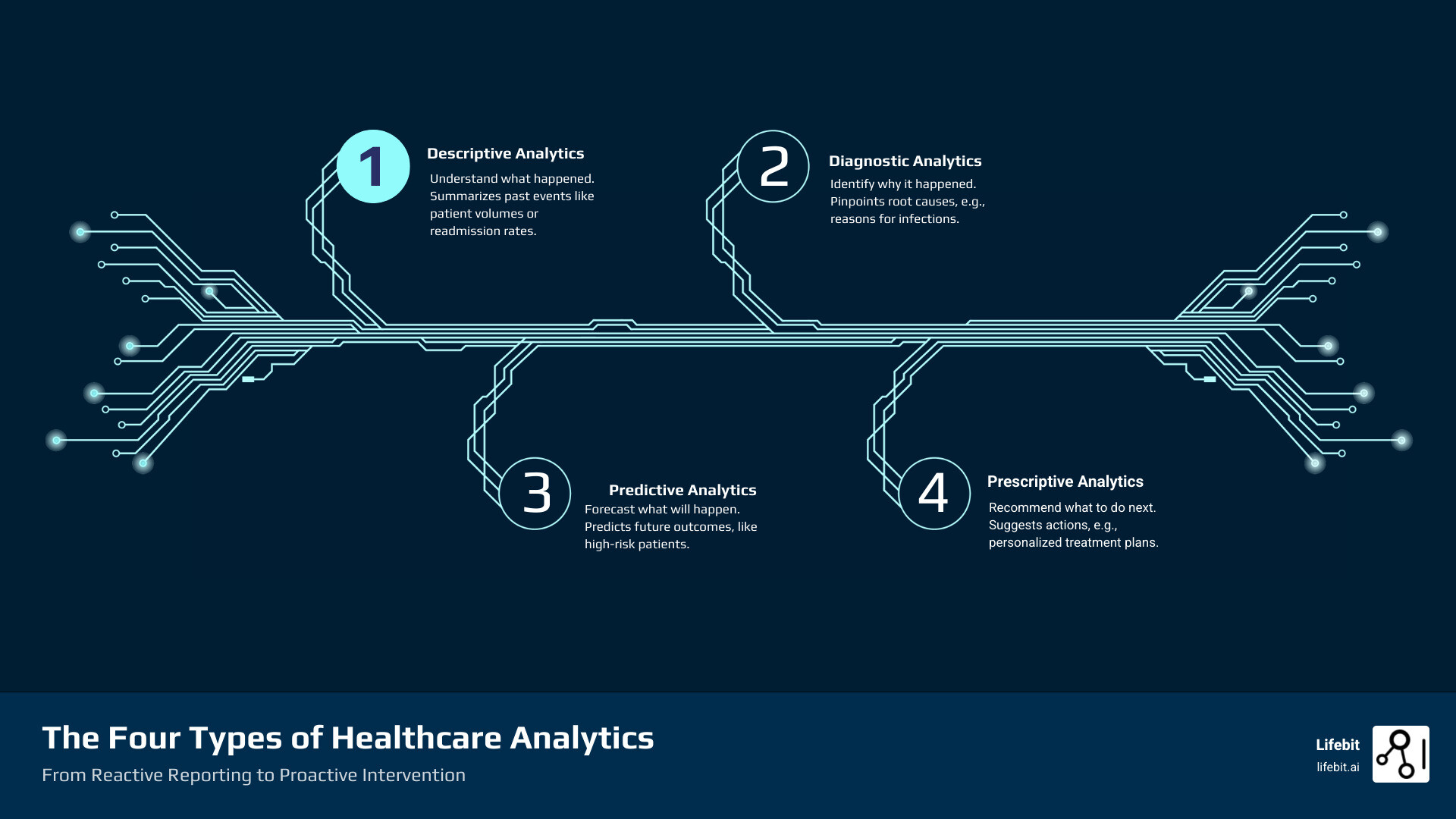
- Descriptive Analytics: Understand what happened (e.g., patient volumes, readmission rates)
- Diagnostic Analytics: Identify why it happened (e.g., root causes of infections)
- Predictive Analytics: Forecast what will happen (e.g., which patients are at risk)
- Prescriptive Analytics: Recommend what to do next (e.g., personalized treatment plans)
Healthcare organizations are drowning in dataelectronic health records, genomic sequences, wearable sensors, insurance claims. Yet most struggle to turn this information into better patient outcomes or smarter operations.
The stakes are high. Unity Health Toronto launched over 50 AI and analytics tools that reduced unanticipated patient deaths by 26%. Meanwhile, organizations without advanced analytics face rising costs, preventable readmissions, and missed opportunities for early intervention.
The gap isn’t about having datait’s about using it. Traditional reporting tells you what already happened. Advanced analytics tells you what’s coming and what to do about it. It’s the difference between reacting to a crisis and preventing it.
But real success requires more than algorithms. You need clean data pipelines, cross-functional teams, and secure environments that respect patient privacy. You need to harmonize structured data from EHRs with unstructured clinical notes and genomic information. And you need tools that work across siloed systems without moving sensitive data.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit, where we’ve spent over 15 years building federated platforms that enable Advanced analytics healthcare at scale across secure, compliant environments for global pharma, regulators, and research institutions. This guide will show you how advanced analytics is reshaping every corner of healthcareand how to implement it successfully in your organization.
Predict Crises Before They Hit: AI That Cuts Deaths 26%
When we talk about advanced analytics healthcare, we’re really talking about a fundamental shift in how we understand and use health data. Think of it this way: traditional business intelligence is like looking in your rearview mirrorit tells you where you’ve been. Advanced analytics, powered by Artificial Intelligence (AI) and Machine Learning (ML), is more like having a GPS with real-time traffic updatesit tells you where you’re going and helps you avoid problems before you hit them.
This isn’t just about fancy algorithms. It’s about moving from reactive reporting to proactive intervention. Instead of finding problems after they’ve already harmed patients or drained budgets, we can spot patterns early and act on them.
Machine Learning excels at finding patterns in massive datasets that would be impossible for humans to detect. Feed it thousands of patient records, and it can identify subtle warning signs that a patient is heading toward a serious complication. For instance, models like Random Forests and Gradient Boosting Machines are commonly used to analyze hundreds of variables in an EHR to generate a real-time risk score for conditions like sepsis or acute kidney injury. Predictive modeling takes this further, forecasting specific eventswhich patients face the highest risk of readmission, how an infectious disease might spread, or when a hospital will face capacity constraints.
But prediction alone isn’t enough. Prescriptive analytics answers the crucial “what now?” question. It doesn’t just warn you that a patient is at riskit recommends the specific interventions most likely to help. For example, it doesn’t just warn that a patient is at high risk for a post-surgical infection; it might recommend a specific prophylactic antibiotic regimen based on the patient’s microbiome data, the type of surgery, and local hospital infection patterns. For a pre-diabetic patient, it could suggest a personalized low-glycemic diet plan and a specific weekly exercise routine, while also modeling the long-term cost-effectiveness of this intervention versus future treatment.
Deep learning, a specialized branch of ML, has revolutionized how we analyze complex data like medical images and genomic sequences. These neural networks can process MRIs, X-rays, and genetic data with remarkable accuracy, powering breakthroughs in both diagnostics and drug findy. For example, in oncology, deep learning models can perform tumor segmentation on MRI scans with pixel-level accuracy, helping to plan radiation therapy. In radiology, they can flag subtle fractures on X-rays that might be missed during a high-volume reading session.
Then there’s Natural Language Processing (NLP), which finally open ups the treasure trove of information buried in unstructured text. Doctor’s notes, clinical reports, patient feedbackNLP transforms this messy, unstructured data into structured insights that can inform care decisions and research. This allows systems to extract critical information like medication adherence, patient-reported symptoms, social determinants of health (e.g., housing instability, food insecurity), and even subtle changes in sentiment that might indicate declining mental healthall from free-text fields. This matters because roughly 80% of healthcare data is unstructured, sitting unused in text form.
What separates advanced analytics from basic business intelligence isn’t just the technologyit’s the ability to transform raw data into actionable intelligence that guides better decisions across the entire healthcare ecosystem.
From Prediction to Action: Proven AI Impact
The real test of any technology is whether it works in the real world, with real patients and real constraints. AI and ML are passing that test with flying colors.
Take Unity Health Toronto’s experience. They didn’t just pilot one AI toolthey deployed over 50 AI and analytics solutions across their system. The results speak for themselves. Their CHARTWatch AI tool reduced unanticipated patient deaths by 26%. That’s not a marginal improvementthat’s lives saved because AI flagged warning signs early enough for clinicians to intervene.
AI in diagnostics is showing similar promise across multiple specialties. Deep convolutional neural networks can now screen for retinopathy of prematurity with remarkable accuracy. In one study, an algorithm correctly diagnosed 91 out of 100 images, while eight human experts averaged 82% accuracy. The AI wasn’t replacing the expertsit was providing consistent, reliable screening that could augment their expertise.
Early disease detection for cancer has seen breakthrough results too. When researchers tested a CNN against 58 dermatologists in diagnosing melanoma, the AI achieved a median area under the curve (AUC) of 0.86 compared to 0.79 for the human experts. You can read more about this peer-reviewed research on AI in diagnostics. This doesn’t mean AI is better than doctorsit means AI can serve as a powerful second opinion, catching cases that might otherwise be missed.
Risk scoring for critical conditions has become a standard tool in many hospitals. Predictive models identify patients at high risk for 30-day readmission or mortality, allowing care teams to focus intensive resources where they’ll have the most impact. These aren’t theoretical exercisesthey’re practical tools helping real-world hospital AI systems allocate limited resources more effectively.
The pattern is clear: we’re moving from prediction to action. AI doesn’t just generate reportsit provides the insights clinicians need to intervene earlier, target resources better, and ultimately save lives. That’s the promise of advanced analytics healthcare being realized today, not someday in the distant future.
End Data Silos Now: Secure Analytics That Boost Outcomes and Catch Fraud
Healthcare has traditionally operated in silosproviders, researchers, payers, and policymakers each working with their own data systems, rarely sharing insights. But advanced analytics healthcare is changing that. We’re finally breaking down these walls and building a connected health system where data flows securely between stakeholders, creating a complete picture of health and disease.
This isn’t just about better technology. It’s about fundamentally rethinking how we collaborate. When a hospital can share anonymized outcomes data with researchers studying treatment effectiveness, when payers can work with providers to identify fraud patterns, when public health officials can access real-time disease surveillance datathat’s when we open up the true power of healthcare data.

The impact of this connected approach touches every corner of healthcare. Let’s look at how different sectors are using advanced analytics to drive real change.
For Healthcare Providers: Better Care, Less Waste
Hospitals and clinics are under constant pressure to do more with lessimprove patient outcomes while controlling costs. Advanced analytics healthcare gives providers the tools to achieve both.
The most powerful application? Predicting which patients need help before they deteriorate. Imagine knowing which patients are at high risk for hospital-acquired infections before they show symptoms, or identifying who’s likely to be readmitted after CABG surgery. These predictive models allow clinical teams to intervene early with targeted care, preventing complications that are both dangerous for patients and expensive for the system.
Another critical application is enhancing diagnostic accuracy. AI algorithms serve as a tireless ‘second pair of eyes’ for specialists like radiologists and pathologists. By analyzing medical images or pathology slides, these tools can highlight suspicious areas, measure abnormalities, and cross-reference findings against vast databases of similar cases. This doesn’t replace the clinician’s judgment but augments it, helping to reduce diagnostic errors, catch diseases earlier, and increase confidence in complex diagnoses, ultimately leading to more appropriate and timely treatment.
Beyond individual patient care, analytics transforms how hospitals run day-to-day operations. By forecasting patient admissions and lengths of stay, we can optimize staff scheduling and resource allocation with remarkable precision. No more overstaffed night shifts or scrambling to find beds during unexpected surges. Resources go where they’re needed, when they’re needed.
The results are measurable: shorter wait times for patients who need care now, lower infection rates from better resource management and infection control protocols, and improved outcomes through evidence-based clinical decision support that helps doctors make the best choices at the point of care. For a detailed look at the tools making this possible, explore our Clinical Analytics Software Ultimate Guide.
For Research and Life Sciences: Accelerating Findies
Drug findy is painfully slow and expensive. Getting a new medication from concept to patient can take over a decade and cost billions. Advanced analytics is changing that timeline.
In drug findy, we use machine learning to identify promising drug targets faster, predict how molecules will interact, and screen thousands of potential compounds in a fraction of the time traditional methods require. During clinical trial optimization, analytics helps identify the right patients, monitor progress in real-time, and spot safety signals earlygetting effective treatments to patients months or even years faster.
But perhaps the most exciting development is real-world evidence (RWE). Instead of relying solely on tightly controlled clinical trials, researchers can now analyze data from actual patient experiences in everyday clinical settings. It’s important to distinguish between Real-World Data (RWD)—the raw data collected from EHRs, claims, and patient registries—and Real-World Evidence (RWE), which is the clinical evidence derived from the analysis of RWD. This evidence is increasingly used by regulatory bodies like the FDA and EMA to support drug approvals, especially for rare diseases where large clinical trials are not feasible, or to expand the approved use of an existing drug. This real-world data (RWD) helps regulatory bodies understand how drugs perform across diverse populations, informs market access strategies, and supports ongoing pharmacovigilance to catch adverse reactions that might not appear in trials.
At Lifebit, we’ve built secure research environments specifically for this kind of collaborative science. Our trusted research platform lets scientists analyze sensitive biomedical data without compromising patient privacy. This enables breakthroughs in Oncology Data Analytics and Precision Medicine Data Analysis by leveraging comprehensive Real-World Data to find rare disease patients and prioritize novel targets. Our Trusted Research Environments make large-scale, collaborative research possible while keeping data secure.
For Payers and Policymakers: Smarter Cost and Population Management
If you’re responsible for managing healthcare costs or public health policy, you’re dealing with an impossible challenge: improve care for entire populations while controlling spiraling expenses. Advanced analytics healthcare provides the intelligence to tackle both.
Fraud detection is a massive opportunity. Healthcare fraud, waste, and abuse drain billions from the system every yearmoney that should go to patient care. Analytics with embedded AI can spot suspicious patterns in claims data, flagging potential fraud for investigation before payments go out. For example, AI can detect sophisticated fraud schemes like ‘upcoding’ (billing for a more expensive service than was provided), ‘phantom billing’ (billing for services never rendered), or coordinated fraud rings involving multiple providers and patients. This isn’t just about catching bad actors; it’s about protecting resources for legitimate care.
For population health management, analytics helps identify who’s most at risk and where to focus limited resources. By creating a complete picture of a healthcare system’s population, we can spot health disparities, predict disease outbreaks, and implement preventive programs before problems explode. This risk stratification approach means high-risk individuals get the intensive support they need, while healthy populations receive appropriate preventive care. Furthermore, advanced analytics is the engine that powers the shift toward value-based care. To succeed in models where payment is tied to patient outcomes rather than the volume of services, payers and providers must be able to accurately measure risk, track outcomes, and identify the most cost-effective care pathways. Without robust analytics, value-based care remains a theoretical ideal rather than a practical reality.
The COVID-19 pandemic showed us how critical this capability is. Public health officials used analytics to predict virus spread, allocate ventilators and PPE, and inform policy decisions that saved lives. That same approach now helps policymakers address everything from improving immunization rates to ensuring healthcare access in underserved communities.
Research confirms this shift is real. A scientific study on Big Data in healthcare found that medical facilities are increasingly moving toward data-based healthcare, empowering decision-makers with evidence to improve public health management and epidemiological surveillance. At Lifebit, we’re working to make Health Data Analysis Platforms for All accessible, ensuring these powerful tools serve the greater good.
Fewer Deaths, Shorter Stays, Lower Costs: What Advanced Analytics Delivers
When we talk about advanced analytics healthcare, we’re not discussing abstract concepts or distant possibilities. We’re talking about measurable improvements happening right nowlives saved, operations streamlined, and costs reduced. The change touches every aspect of healthcare delivery, from the individual patient encounter to system-wide resource management.
Improving Patient Outcomes
The most compelling reason to accept advanced analytics is simple: it helps us take better care of people. Instead of waiting for problems to emerge, we can now anticipate them and act early.
Consider personalized medicine, where treatment isn’t a one-size-fits-all approach. By analyzing genetic data alongside clinical history and lifestyle factors, AI-powered solutions can tailor therapies to each individual. This turns what used to be guesswork into precision care, meaning fewer ineffective treatments, fewer side effects, and better outcomes.
Proactive interventions change the entire dynamic of care delivery. When we identify patients at high risk for sepsis, heart failure, or dangerous complications, clinicians can step in before a crisis develops. Unity Health Toronto’s CHARTWatch tool demonstrates this powerreducing unanticipated patient deaths by 26% isn’t just a statistic. Behind that number are real people who went home to their families instead of becoming another preventable tragedy.
Early disease detection powered by AI has shown remarkable results. Deep convolutional neural networks now diagnose retinopathy of prematurity with 91% accuracy, outperforming human experts who averaged 82%. In melanoma detection, these systems achieved a median area under the curve of 0.86 compared to 0.79 for experienced dermatologists. Earlier detection means earlier treatment, which often means the difference between a manageable condition and an advanced disease.
All these capabilities work together to lower mortality rates and improve treatment planning across conditions. The shift from reactive to proactive care is fundamentally changing what’s possible in medicine.
Boosting Operational Efficiency
Healthcare organizations operate under constant pressuretoo many patients, too few resources, never enough time. Advanced analytics healthcare helps ease that pressure by making operations smarter and more efficient.
Streamlined workflows and automated reporting free staff from tedious manual tasks. Instead of spending hours compiling reports, analytics platforms generate them automatically, ensuring consistency and giving people time back to focus on what matters most: patient care.
Optimized resource allocation transforms how hospitals function. By forecasting patient volumes and predicting lengths of stay, administrators can match staffing levels to actual need, allocate beds more effectively, and ensure equipment is available where it’s needed. No more overstaffed slow days followed by chaotic understaffed emergencies.
The reduced administrative burden makes a tangible difference in clinician burnout and satisfaction. AI tools are handling more of the paperwork, documentation, and scheduling that used to consume hours of a provider’s day. When doctors and nurses spend less time on admin work, they have more energy for the human connections that drew them to healthcare in the first place.
Better resource management and improved clinical decision-making naturally lead to shorter patient stays. When care is delivered more efficiently, patients recover faster and return home soonera win for both the patient and the healthcare system.

Think of a modern hospital command center, with real-time dashboards showing patient flow, resource utilization, and risk alerts. This isn’t science fictionit’s how leading healthcare systems operate today, using data to make rapid, informed decisions that keep everything running smoothly.
Driving Down Costs
The financial reality of healthcare is stark: costs keep rising while budgets remain flat or shrink. Advanced analytics offers a practical path to doing more with less, without sacrificing quality.
Preventing costly adverse events delivers immediate savings. A single case of sepsis can cost tens of thousands of dollars to treat. A surgical complication can double the cost of a procedure. When predictive models identify high-risk patients early, targeted interventions prevent these expensive complications before they happen.
Reducing readmission penalties matters increasingly as payers penalize hospitals for patients who return within 30 days. Analytics identifies which patients face the highest readmission risk, enabling targeted post-discharge support like home visits, medication management, and follow-up calls. These relatively inexpensive interventions prevent costly readmissions while improving patient experience.
Optimizing the supply chain might sound unglamorous, but it represents significant savings. Analytics reveals patterns in purchasing, identifies supplier performance issues, and highlights inventory inefficiencies. Small improvements across thousands of items add up to millions in savings.
In the insurance sector, eliminating fraudulent claims protects billions of dollars annually. Advanced analytics with embedded AI capabilities can rapidly detect suspicious patterns, investigate potential fraud, and prevent payment on illegitimate claimsmoney that can instead fund patient care.
Perhaps most importantly, analytics enables a shift to preventative care. Identifying at-risk populations allows targeted prevention programs that are far more cost-effective than treating advanced disease. Helping someone manage their diabetes through lifestyle changes and medication costs a fraction of treating kidney failure or amputations. This strategic shift doesn’t just save moneyit prevents suffering and improves quality of life.
The financial benefits of advanced analytics healthcare aren’t theoretical. They’re measurable, substantial, and growing as more organizations adopt these tools. The question isn’t whether analytics saves moneyit’s how quickly you can start realizing those savings.
Stop Pilot Purgatory: Deploy Advanced Analytics That Clinicians Use
Success with advanced analytics healthcare takes more than cutting-edge technology. It requires a thoughtful strategy that brings together your data, your people, and your processes. Think of it as building a houseyou need a solid foundation before you can add the smart home features.
The reality is that most healthcare organizations already have the raw materials. What they’re missing is the blueprint for putting it all together in a way that actually works.
Handling Complex Healthcare Data
Healthcare data is messy, and that’s putting it mildly. You’re dealing with information that arrives in different formats, from different sources, at different times. Some of it is neatly organized in databases. Much of it isn’t.
Structured data is the easy partthings like electronic health records, insurance claims, lab results, and vital signs. These come in neat rows and columns that computers love. They’re predictable, searchable, and relatively straightforward to analyze.
Unstructured data is where things get interesting (and complicated). Clinical notes written by doctors, medical images like X-rays and MRIs, genomic sequences, patient feedback surveys, even audio recordings of patient consultationsall of this contains valuable insights, but it doesn’t fit into traditional database tables.
The challenge isn’t just handling these different types of data separately. It’s bringing them together in a meaningful way. A patient’s genomic data might reveal a predisposition to a certain condition, but you need to combine that with their clinical notes, lab results, and treatment history to get the full picture.
Data integration is often where implementation efforts stumble. Healthcare systems have grown organically over decades, with different departments using different software that doesn’t talk to each other. Breaking down these silos requires both technical solutions and organizational willpower.
Data quality and governance can’t be an afterthought. Garbage in, garbage out applies doubly in healthcare, where poor data quality can literally cost lives. You need clear policies about who can access what data, how it’s stored, how it’s protected, and how you ensure its accuracy. This isn’t just good practiceit’s often a regulatory requirement.
Data harmonization—getting data from different sources to speak the same language—is particularly crucial when you’re working across multiple institutions or countries. One hospital’s “high blood pressure” might be coded differently than another’s. This is where data standards and common data models become indispensable. Standards like HL7 FHIR (Fast Healthcare Interoperability Resources) provide a common language for exchanging healthcare information, while models like the OMOP (Observational Medical Outcomes Partnership) Common Data Model transform data from disparate sources into a standard format. Adopting these standards is a heavy lift, but it’s the foundational work that enables scalable, multi-institutional research and analytics. Lifebit’s platform includes built-in capabilities for harmonization, making it possible to analyze data from diverse sources without compromising security or spending months on manual data cleaning.
Building Your Analytics Team
Technology alone won’t get you there. You need people who understand both the data and the healthcare context it lives in.
Data scientists bring the statistical and machine learning expertise to build predictive models and extract insights from complex datasets. They’re the ones turning raw data into actionable intelligence.
Data engineers build and maintain the infrastructure that makes analytics possiblethe pipelines that move data, the systems that store it, and the platforms that make it accessible. Without them, even the best data scientists are stuck waiting for data.
Clinical informaticists are your bridge between the technical team and the clinical staff. They understand both medicine and data, which makes them invaluable for ensuring that your analytics actually address real clinical needs rather than just technical possibilities.
But here’s the thing: these roles need to work together, not in isolation. Cross-functional collaboration isn’t optionalit’s essential. Your data scientists need to understand clinical workflows. Your clinicians need to trust and understand the models. Your engineers need to build systems that work in the real world, not just in theory.
Perhaps most importantly, you need to foster a data-driven culture throughout your organization. This means getting buy-in from leadership, training staff to use analytics tools, and creating an environment where decisions are based on evidence rather than intuition alone.
At Lifebit, we recognize that building this capability takes time and support. That’s why we’ve launched initiatives like the Health AI Academy to help organizations develop the skills they need to succeed with advanced analytics.
Overcoming Analytics Challenges in Healthcare
Let’s be honest: implementing analytics in healthcare is hard. Really hard. But understanding the common pitfalls can help you avoid them.
Integration with existing IT systems is often the first major hurdle. Healthcare organizations have invested millions in their current systems, and ripping everything out to start fresh isn’t realistic. Your analytics solution needs to work with what’s already there, not replace it entirely. This is where federated approaches shinethey allow you to analyze data where it lives without requiring massive migration projects.
Model validation and evaluation is critical in healthcare, where the stakes are literally life and death. A model that works beautifully on historical data might fail when deployed in the real world. You need rigorous testing, ongoing monitoring, and clear metrics for success. For practical considerations on improving healthcare with advanced analytics, this research article offers valuable insights.
Addressing Ethical Concerns and Algorithmic Bias: A challenge of paramount importance is ensuring that AI models are fair, transparent, and ethical. Healthcare data often reflects historical and systemic biases in how care is delivered. If a model is trained on this biased data, it can learn and even amplify those inequities. For example, an algorithm designed to predict healthcare needs might inadvertently allocate fewer resources to minority populations if it uses cost as a proxy for need, and those populations have historically received less costly care. To combat this, organizations must prioritize ‘algorithmic hygiene.’ This involves conducting fairness audits to check for biased performance across different demographic groups, ensuring model transparency so clinicians can understand why a recommendation was made (a concept known as ‘explainable AI’ or XAI), and establishing strong governance frameworks to oversee the entire lifecycle of an AI model, from development to deployment and ongoing monitoring. Ignoring these ethical dimensions not only risks harming patients but also erodes the trust necessary for clinical adoption.
Ensuring clinical adoption might be your biggest challenge of all. Doctors and nurses are busy, often skeptical of new technology, and rightly cautious about tools that might affect patient care. Your analytics solution needs to fit into existing workflows, not create extra work. It needs to earn trust by demonstrating clear value and being transparent about how it reaches its conclusions.
Scalability becomes an issue faster than you’d think. A pilot project with 100 patients is one thing. Scaling to 100,000 patients across multiple facilities is entirely different. Your infrastructure needs to handle that growth without breaking, and your costs need to remain sustainable.
The good news? None of these challenges are impossible. Organizations around the world are successfully implementing advanced analytics healthcare solutions and seeing real results. The key is approaching implementation as a journey, not a destinationstarting with clear goals, building incrementally, learning from setbacks, and keeping patient outcomes at the center of everything you do.

