Healthcare Data Integration Standards 101

Your Health Data Is Trapped. Standards Are the Key to Open uping It.
Healthcare data integration standards are the rules that let different health systems share patient information safely and efficiently. Without them, your organization’s critical data is trapped in silos, creating dangerous gaps in patient care and blocking the insights needed for better outcomes.
Key healthcare data integration standards include:
- HL7 FHIR: A modern API standard for real-time data exchange.
- USCDI: The core data set mandated for U.S. interoperability.
- SNOMED CT: Universal clinical terminology for diagnoses and procedures.
- LOINC: Standard codes for lab tests and clinical observations.
- DICOM: The standard for medical imaging like CT scans and MRIs.
Historically, the lack of common standards has fragmented healthcare, preventing information sharing between labs, pharmacies, providers, and payers. This doesn’t just slow down operations—it puts patient safety at risk when care teams can’t access a complete medical history.
Imagine a patient’s medical history is scattered across dozens of disconnected systems. Their care team struggles to piece together a complete health story, leading to delayed decisions and compromised safety. The solution is adopting standardized approaches to data integration. When implemented correctly, these standards enable the delivery of the right care at the right time, reduce administrative burdens, and open up powerful AI-driven insights.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. I’ve spent over 15 years developing healthcare data integration standards and federated analytics platforms to break down data silos, accelerate precision medicine, and improve patient outcomes.
The Blueprint for Interoperability: Key Data Exchange Standards
Think of healthcare data integration standards as the universal translators of medicine. They provide the shared rules for data exchange formats, messaging, and APIs that allow different systems to communicate. Without them, sharing patient information is like having a conversation where everyone speaks a different language—critical information gets lost, delaying care and risking patient safety. When data exchange is standardized, a patient’s medical history can follow them instantly to a new specialist, and researchers can seamlessly combine data from multiple sources, creating a connected healthcare ecosystem.
HL7: The Backbone of Health Messaging
Health Level Seven (HL7) has been the foundation of healthcare messaging since 1987. Its most widespread version, HL7v2, is used by over 90% of U.S. healthcare organizations. It organizes information into pipe-and-hat delimited text messages with predictable segments (e.g., a PID segment for Patient Identification). However, its implementation flexibility—allowing for custom “Z-segments”—sometimes created interoperability challenges, as each implementation could be slightly different.
To address document sharing, HL7 developed C-CDA (Consolidated Clinical Document Architecture). C-CDA provides standardized XML-based templates for common clinical documents like discharge summaries and the crucial Continuity of Care Document (CCD). While excellent for sharing snapshots of a patient’s history, C-CDA documents are often large and not easily queryable for specific data points.
HL7 V3 was a later attempt to create more structured messaging formats using a rigorous Reference Information Model (RIM), but its complexity hindered widespread adoption, paving the way for a more modern approach.
For a full overview, see the HL7 standards documentation.
FHIR: The Modern API for Real-Time Healthcare Data
If HL7v2 is like sending a letter, FHIR (Fast Healthcare Interoperability Resources) is like an instant message. Launched by HL7 in 2014, FHIR uses web-based, developer-friendly RESTful APIs. It breaks data into modular “resources”—like LEGO blocks—such as a Patient resource for demographics or an Observation resource for lab results.
This architecture is ideal for mobile app integration and cloud communication, as developers can request only the specific data they need (e.g., “get the latest blood pressure reading for this patient”). FHIR supports modern formats like JSON and XML, and its extension mechanism allows for customization while maintaining a common base compatibility. The result is faster integration, lower development costs, and greater flexibility in using patient data for innovative applications, such as patient-facing health apps.
Learn more about FHIR to see how it’s reshaping health tech.
DICOM, X12, and SCRIPT: Specialized Exchange Standards
Beyond clinical messaging, other critical standards serve specific domains.
- DICOM (Digital Imaging and Communications in Medicine) is the universal standard for medical imaging. It’s more than an image format; DICOM defines a comprehensive protocol for storing and transmitting medical images and their associated metadata. This ensures that a CT scan, MRI, or X-ray can be viewed on any compatible system, complete with crucial information like patient ID and study details.
- X12 standards handle the business side of healthcare, defining electronic formats for insurance claims, eligibility verification, and other administrative and billing data exchanged between providers and payers.
- NCPDP SCRIPT standards enable secure e-prescribing, ensuring prescription details are transmitted accurately between providers, pharmacies, and payers to reduce medication errors.
Together, these specialized standards work with the broader HL7 ecosystem to support coordinated and efficient care.
USCDI: The Mandated Core Data Set for U.S. Interoperability
The United States Core Data for Interoperability (USCDI) is a standardized set of health data classes and elements that all certified health IT systems in the U.S. must be able to exchange. Mandated by the 21st Century Cures Act and managed by the Office of the National Coordinator for Health Information Technology (ONC), USCDI defines the minimum data that must flow freely and securely between healthcare systems, providers, and patients.
Without USCDI, a patient’s lab results from one hospital might not be accessible to their primary care doctor. USCDI creates the common vocabulary and structure that makes seamless, nationwide patient care possible, breaking down the data silos that have long plagued the industry.

The Evolution of USCDI
USCDI is not a static standard; it evolves annually through a public, collaborative process to meet the changing needs of the healthcare ecosystem. The process began with USCDI v1, which established the foundational data set. Each subsequent version has expanded on this core, reflecting industry feedback and emerging health priorities.
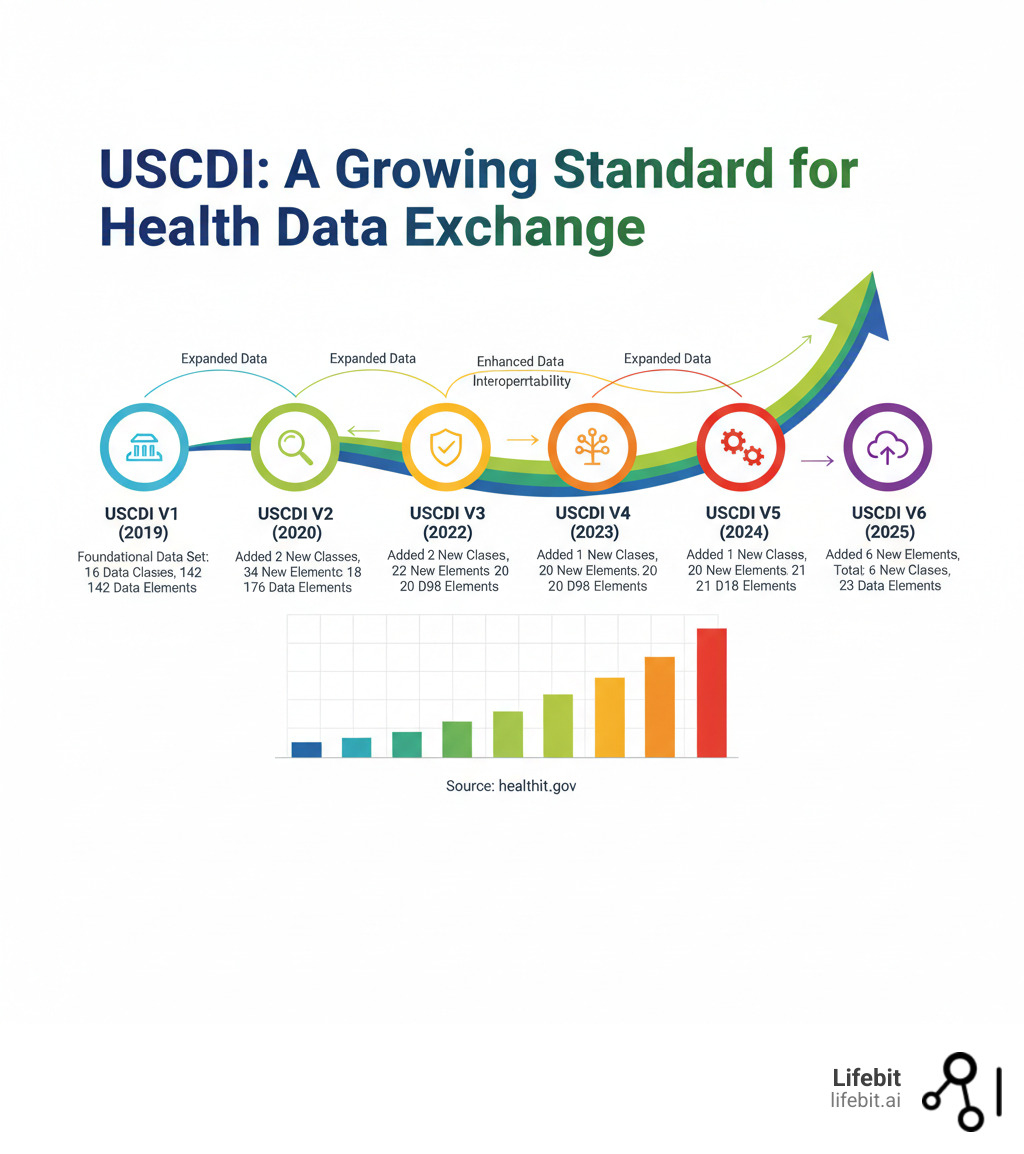
Recent versions have significantly expanded the standard’s scope. For example, USCDI v3 improved patient demographic data to include elements for Sexual Orientation and Gender Identity (SOGI). USCDI v4 added 20 new data elements and a new data class for Facility Information. The evolution continues with USCDI v5, which introduced new data elements related to health status, and the draft USCDI v6, which proposes additions for public health reporting. This iterative process ensures the standard remains relevant, incorporating critical information like Social Determinants of Health (SDOH) and Health Insurance Information, recognizing that healthcare extends far beyond clinical data.
USCDI Structure: Data Classes and Elements
USCDI organizes data into a logical hierarchy of Data Classes (broad categories) and Data Elements (specific information). This structure provides a clear framework for health IT developers. Key Data Classes in USCDI include:
- Allergies and Intolerances
- Care Team Members
- Clinical Notes
- Diagnostic Imaging
- Encounter Information
- Health Insurance Information
- Immunizations
- Laboratory
- Medications
- Patient Demographics
- Problems
- Procedures
- Provenance
- Social Determinants of Health (SDOH)
- Vital Signs
For example, the Problems Data Class includes Data Elements like “Problem/Diagnosis Name,” “Date of Diagnosis,” and “Clinical Status.” This ensures that when a patient’s problem list is exchanged, all systems can parse and display this critical information consistently.
How USCDI Drives Interoperability and Addresses SDOH
USCDI turns the abstract goal of interoperability into concrete requirements. Through the ONC Health IT Certification Program, it mandates that EHRs support this common data set, ensuring a patient’s core information can follow them across different care settings. This leads to better-informed clinical decisions and fewer medical errors.
The inclusion of Social Determinants of Health is a major shift, requiring systems to capture data on non-clinical factors like housing instability and food insecurity. This allows providers to understand the whole patient, tailor care plans, and connect patients with social services, acknowledging that a patient’s zip code can be as important as their genetic code.
For providers, USCDI means a more complete patient picture. For EHR vendors, it shifts competition toward innovation. For patients, it means safer care and unprecedented access to their own health information. Initiatives like USCDI+ for Public Health further extend these benefits, creating specialized datasets for needs like cancer surveillance and maternal health.
Terminology Standards: Ensuring Data Means the Same Thing Everywhere
Imagine a patient’s record says “heart attack,” but the billing system uses code “I21.9” for “myocardial infarction.” They mean the same thing, but without standardized medical language, computer systems can’t connect the dots. This is why healthcare data integration standards must also ensure data is understood consistently. This is known as semantic interoperability.
Terminology standards provide the precise coding systems to represent medical concepts, ensuring the meaning of data remains clear as it moves between systems. This is critical for accurate data analysis, reliable clinical decision support, and patient safety.
SNOMED CT: The Global Language for Clinical Concepts
SNOMED CT (Systematized Nomenclature of Medicine – Clinical Terms) is the world’s most comprehensive clinical terminology, containing over 350,000 unique concepts. Its power lies in its structure: each concept has a unique identifier, multiple descriptions (synonyms), and defined relationships to other concepts. For example, “Viral pneumonia” is linked to “Infectious pneumonia” with an “Is a” relationship, and to “Lung” with a “Finding site” relationship. This polyhierarchical structure allows for sophisticated, machine-readable queries and reasoning. Its granular vocabulary covers everything from symptoms and diagnoses to procedures, allowing clinical decision support systems to understand nuances and provide more intelligent alerts.
LOINC and RxNorm: The Standards for Labs and Medications
Specialized vocabularies for labs and medications are essential to prevent dangerous errors.
LOINC (Logical Observation Identifiers Names and Codes) is the universal language for identifying lab tests and clinical measurements. Each LOINC term is highly specific, defined by parts like the component, specimen type, and timing. This precision is vital. For example, LOINC can distinguish between “Glucose in Serum or Plasma” and “Glucose in Urine,” which are clinically very different. Using LOINC ensures that a lab result from any facility can be correctly interpreted and trended over time.
RxNorm, from the National Library of Medicine, provides standardized names for clinical drugs. It normalizes brand and generic names into a common representation that includes the active ingredient, strength, and dose form. This ensures that a prescription for “Tylenol 500mg tablet” is understood by the doctor and pharmacy in the same way as “Acetaminophen 500mg tablet,” preventing confusion.
The Challenge of Terminology Mapping
One of the biggest hurdles in achieving semantic interoperability is terminology mapping—the process of linking a local or legacy code system to a standard one. Many hospitals have historically used proprietary codes for lab tests or billing. To integrate this data, each local code must be accurately mapped to its corresponding LOINC or SNOMED CT code. This is a complex, resource-intensive task that requires clinical expertise and specialized tools. Without proper mapping, data remains siloed and unusable for larger-scale analytics, undermining the purpose of adopting standards.
ICD, CPT, and Other Classification Systems for Administration
Beyond clinical care, standardized codes are needed for billing, reporting, and public health.
- ICD-10-CM (International Classification of Diseases) provides codes for diseases and injuries, used for billing and public health reporting.
- CPT (Current Procedural Terminology) describes medical procedures and services for billing and reimbursement.
- HCPCS (Healthcare Common Procedure Coding System) covers a broader range of services and supplies.
- NDC (National Drug Code) identifies specific drug products for inventory and billing.
- NPI (National Provider Identifier) assigns unique IDs to healthcare providers.
These systems work with clinical terminologies to create a seamless flow of information that supports both patient care and healthcare administration.
From Standards to Breakthroughs: Powering AI and Research
Healthcare data integration standards are more than just compliance requirements; they are the foundation for the future of medicine. When patient records, lab results, and imaging studies all follow common standards, data transforms from a passive record into a powerful asset for innovation.
The global healthcare data integration market is projected to grow at a CAGR of 14.5% through 2032, as organizations recognize the transformative power of connected data. Federated platforms like Lifebit leverage these standards to enable secure, real-time analysis across diverse datasets without forcing data movement or compromising privacy.
Fueling AI and Advanced Analytics
AI in healthcare is only as good as its data. Messy, inconsistent data leads to unreliable results. When clinical, genomic, and real-world data speak the same language, AI becomes a powerful clinical tool. Machine learning models thrive on clean, standardized data, enabling them to build robust predictive models for disease risk, treatment response, and patient outcomes.
The applications are transformative:
- Predictive Analytics: AI models trained on standardized EHR data can flag a patient’s high risk for sepsis hours before symptoms appear, enabling early intervention for conditions like hospital-acquired infections or heart failure.
- Population Health Management: With standardized data, organizations can analyze health trends across large populations, identify at-risk communities, and deploy targeted interventions for chronic disease management.
- AI-Powered Diagnostics: In radiology, AI algorithms trained on DICOM images can help detect subtle signs of cancer in MRIs and CT scans, acting as a second pair of eyes for radiologists.
- Generative AI and Clinical Workflows: Emerging generative AI tools can assist providers by summarizing clinical notes and packaging observations as structured FHIR resources directly into the EHR, reducing administrative burden.
Lifebit’s platform provides built-in capabilities for data harmonization and advanced AI/ML analytics, delivering real-time insights while keeping sensitive data secure.

Accelerating Clinical and Real-World Research
Standards have revolutionized clinical research. Successful trials now depend on harmonizing data from diverse sources. CDISC (Clinical Data Interchange Standards Consortium) standards are crucial for this process and are required by regulatory bodies like the FDA for new drug submissions. These include:
- CDASH (Clinical Data Acquisition Standards Harmonization): Standardizes the collection of data in clinical trials.
- SDTM (Study Data Tabulation Model): Provides a standard format for organizing and submitting trial data.
- ADaM (Analysis Data Model): Defines a standard for creating analysis datasets.
You can explore more about CDISC standards for clinical research.
Integrating EHR data with Real-World Data (RWD)—data collected outside of traditional trials—provides invaluable insights. When standardized, this data can be used to generate Real-World Evidence (RWE) to support regulatory decisions, create external control arms to accelerate trials, and conduct post-market safety monitoring.
Federated learning is the cutting edge of this evolution. It allows AI models to be trained across multiple, distributed datasets without the data ever leaving its secure, local environment. This enables large-scale research across hospital networks while maintaining strict privacy and data sovereignty—a core capability of Lifebit’s federated platform.
The Bottom Line for Providers, Payers, and Patients
The adoption of healthcare data integration standards benefits the entire ecosystem:
- Providers get a complete view of patient histories, leading to better decisions, fewer errors, and reduced administrative burden.
- Patients benefit from unified health records, proactive care, and safer, more personalized treatment plans.
- Payers and organizations pursuing value-based care can streamline reporting and focus on improving outcomes instead of managing paperwork.
Standards create an environment where innovation thrives and healthcare becomes more proactive and responsive to patient needs.
Frequently Asked Questions about Healthcare Data Integration Standards
What is the difference between data exchange standards (like FHIR) and terminology standards (like SNOMED)?
Think of it like sending a letter. Data exchange standards (FHIR, HL7) are the postal system: they define the envelope, address format, and delivery process. Terminology standards (SNOMED CT, LOINC) are the language inside the letter, ensuring the message is understood correctly upon arrival.
Exchange standards provide the technical framework for moving data, while terminology standards provide the shared medical vocabulary so that a diagnosis of “Myocardial infarction” (SNOMED code 22298006) means the same thing everywhere. You need both for true interoperability.
Why are there so many different healthcare data standards?
Healthcare data standards evolved over time to solve specific problems, much like a city grows with a mix of old streets and modern highways. DICOM was created for medical imaging, HL7v2 for early EHR messaging, and X12 for financial transactions. Each served a unique purpose.
Today, the industry is focused on harmonizing these legacy systems. Modern standards like FHIR act as flexible bridges, creating a universal translator that helps all these different data “languages” work together.
Who enforces the use of these standards in the US?
The Office of the National Coordinator for Health Information Technology (ONC) is the primary enforcer in the United States. Through the 21st Century Cures Act, the ONC has the authority to mandate standards for certified health IT.
This means EHR vendors must support standards like USCDI and FHIR-based APIs to achieve certification, which is a requirement for most healthcare providers. Failure to comply can result in penalties. Other bodies, like the FDA, also enforce standards, requiring CDISC for clinical trial data submissions. This regulatory push is accelerating nationwide interoperability by breaking down data silos.
Conclusion: Turn Your Standardized Data into Actionable Intelligence
The journey from fragmented data to actionable intelligence is powered by healthcare data integration standards. Standards like HL7, FHIR, USCDI, and SNOMED are not just for compliance—they are the keys to open uping the immense value trapped in healthcare data silos.
When implemented correctly, these standards transform raw information into a cohesive patient story. This enables providers to deliver personalized care, researchers to accelerate findies, and AI systems to predict outcomes with greater accuracy. The entire healthcare system shifts from being reactive to proactive.
At Lifebit, we’ve built our next-generation federated AI platform to amplify the power of these standards. We enable secure, real-time access to global biomedical datasets without compromising privacy or data sovereignty. With built-in harmonization, advanced AI/ML, and federated governance, we help organizations turn standardized data into insights that drive better outcomes for patients worldwide.
The future of healthcare is data that works together seamlessly, securely, and intelligently. That future starts with standards.
Ready to transform your healthcare data into powerful insights? Explore Lifebit’s federated data platform to see how we can help you harness the full potential of standardized healthcare data.

