The Pulse of Care: Unlocking Real-Time Patient Insights

From Hindsight to Foresight in Healthcare
Real-time patient insights are changing healthcare from a reactive discipline to a proactive science. Instead of waiting for data from disconnected systems, clinicians can now access immediate, AI-powered analysis of patient data as it’s generated. This enables faster diagnoses, earlier interventions, and better outcomes, with proven results like a 32% improvement in sepsis detection and a 32% reduction in hospital readmissions.
The challenge isn’t collecting data—healthcare generates 30% of the world’s data. The challenge is making that data actionable in the moment it matters most. When an emergency nurse receives a real-time alert about an impending patient surge 90 minutes before it happens, that’s the difference between chaos and coordinated care.
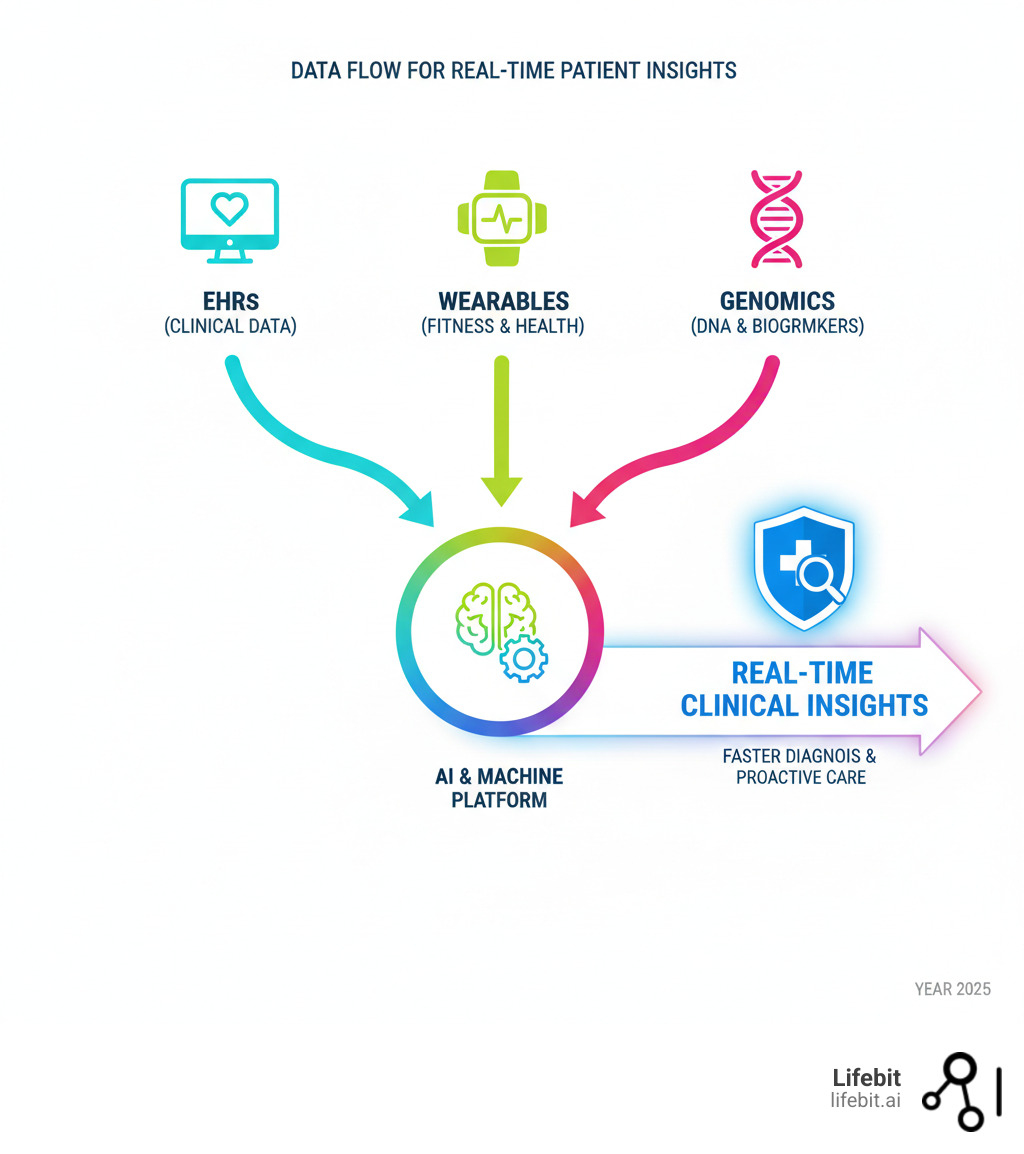
Traditional Electronic Health Records (EHRs) store data, but they don’t analyze it in real-time to predict which patient will develop sepsis or identify undiagnosed patients. Real-time patient insights bridge this gap by combining data from EHRs, wearables, labs, and genomics and applying AI to generate immediate intelligence. This isn’t about replacing clinicians; it’s about giving them superpowers to see patterns humans can’t and intervene before problems escalate.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. We build platforms that transform fragmented biomedical data into real-time patient insights using federated analytics and AI. Our work proves that the technology exists today to make proactive, precision healthcare a reality.
Relevant articles related to Real-time patient insights:
Step 1: Unify Fragmented Data into a Single Source of Truth
Healthcare data is vast but fragmented, locked away in isolated systems. Lab results, imaging studies, wearable readings, and genomic data all live in different places. This fragmentation is the biggest barrier to achieving real-time patient insights. A clinician in the ER at 2 AM needs a complete, unified view of a patient’s history now, not after logging into six different systems.
The journey to real-time insights begins with data aggregation and harmonization, bringing together information from Electronic Health Records (EHRs), wearable technology, digital pathology, and multi-omic data into a single source of truth. For instance, digital pathology transforms physical slides into high-resolution digital images that can be analyzed by AI to detect cancer with greater accuracy. Multi-omic data—including genomics, proteomics, and metabolomics—provides a deep, molecular-level view of a patient’s health, unlocking insights into disease mechanisms and potential personalized therapies. This requires a robust framework of interoperability standards. While FHIR (Fast Healthcare Interoperability Resources) is the modern standard for API-based data exchange, a comprehensive strategy must also account for legacy standards like HL7v2, which still powers much of the internal messaging within hospitals, and DICOM for medical imaging. True interoperability involves creating a flexible data layer that can ingest, translate, and normalize data from all these formats, ensuring that a patient’s complete longitudinal record is available. Scientific research on real-time data capture shows how modern platforms can turn data chaos into clinical clarity.
How to Harness Electronic Health Records (EHRs)
Your EHR stores data well, but it struggles with real-time analysis, especially when patient information is spread across multiple facilities in data silos. To open up real-time patient insights from EHRs, we must connect to disparate systems and standardize information using frameworks like FHIR. This allows for the aggregation of data from multiple sources—like different pharmacies, labs, and hospitals—into a single, actionable patient profile. An emergency physician can instantly see a complete medication history, avoiding potentially dangerous prescribing errors and making informed, life-saving decisions. Beyond emergencies, this unified view helps manage chronic conditions. A primary care physician can see notes and prescriptions from a patient’s cardiologist and endocrinologist in one place, identifying conflicting treatments or tracking the progression of comorbidities over time without manual record requests.
At Lifebit, our platform handles this data harmonization behind the scenes, turning disconnected records into a cohesive patient story. Learn more about our approach to clinical data insights.
Integrating Patient-Generated Health Data
Patients generate continuous health data daily through wearable technology like smartwatches and remote monitoring devices. This data—heart rate, activity levels, sleep patterns—provides an unprecedented, real-time window into patient health outside the clinic, revealing patterns that might otherwise go unnoticed.

For example, a 12-year-old girl’s Apple Watch detected an unusually high heart rate, leading to an early diagnosis of a rare tumor. This is the power of patient-generated data: it catches problems early and provides context a 15-minute office visit cannot. This includes data from not just smartwatches but also continuous glucose monitors (CGMs) for diabetic patients, smart scales, connected blood pressure cuffs, and even smart pill bottles that track medication adherence. The challenge is integrating this high-velocity data stream securely so clinicians can use it. However, integrating this data comes with challenges of validation and context. A platform must be able to distinguish a true arrhythmia from a sensor error caused by vigorous exercise and present this information to clinicians with appropriate context to avoid alert fatigue. Our platforms harmonize these diverse data streams, ensuring clinicians see the complete picture and can shift from reactive to proactive care.
Step 2: Use AI to Generate Real-Time Patient Insights
Having unified data is the first step; applying Artificial Intelligence (AI) and Machine Learning (ML) is what brings real-time patient insights to life. While traditional analysis is retrospective, AI enables predictive analytics, helping healthcare teams anticipate health crises and identify at-risk patients before they occur. This proactive capability is the core of modern, data-driven healthcare.
The results are transformative. AI’s role in improving sepsis detection has shown that real-time analytics can improve detection rates by up to 32%, saving thousands of lives. At Lifebit, our platform uses advanced AI/ML to turn raw data into actionable intelligence, creating systems that tell you what’s about to happen and what to do about it.
The Machine Learning Engines Behind the Insights
The term ‘predictive model’ encompasses several types of machine learning, each suited for different clinical questions:
- Classification Models: These models answer ‘yes/no’ questions, such as ‘Is this patient at high risk for sepsis?’ or ‘Is this lesion malignant?’ They are the workhorses behind many diagnostic and risk-stratification tools.
- Regression Models: These models predict a continuous value, such as ‘What is the patient’s likely length of stay?’ or ‘What will this patient’s blood glucose level be in three hours?’ This is crucial for resource planning and proactive management of chronic conditions.
- Clustering Models: These models are used for unsupervised learning, identifying natural groupings or ‘phenotypes’ within a patient population. For example, clustering can reveal previously unknown subtypes of a disease, which can lead to more targeted treatment strategies.
How Predictive Models Identify At-Risk Patients
AI-powered predictive models analyze vast amounts of patient data—EHR records, labs, vitals, and genetics—to flag individuals at risk of adverse events. For sepsis, which claims 350,000 adult lives annually in the U.S., early detection is critical. The Medical University of South Carolina (MUSC) successfully uses machine learning to monitor patients and improve detection rates by 32%.
The impact goes beyond sepsis. Predictive models have helped reduce hospital readmissions by 32% and identified 95 times more undiagnosed rare disease patients than traditional methods. For uncontrolled asthma, models have shown 86% accuracy, and for treatment efficacy, some models have demonstrated a 16-fold conversion rate compared to controls. Other critical applications include:
- Predicting Patient Deterioration: In the ICU, models can analyze real-time streams of vital signs, lab results, and ventilator data to predict the onset of Acute Respiratory Distress Syndrome (ARDS) hours before it becomes clinically apparent.
- Forecasting Hospital ‘No-Shows’: By analyzing patient demographics, appointment history, and even external factors like weather or traffic, health systems can predict which patients are likely to miss appointments. This allows schedulers to proactively engage these patients with reminders or offer telehealth options, improving clinic efficiency and continuity of care.
- Identifying Chronic Disease Risk: Machine learning can sift through years of EHR data to identify individuals on a trajectory toward developing chronic conditions like Type 2 diabetes or hypertension, enabling early lifestyle interventions.
These are not abstract numbers; they represent real patients getting the right care at the right time.

Using Generative AI for On-Demand Real-time patient insights
Generative AI is making real-time patient insights accessible to everyone on the care team, not just data scientists. Imagine asking your patient data a question in plain English: “Show me all patients over 65 with heart failure who’ve been readmitted in the last 30 days.” You get an instant, comprehensive answer.
This technology democratizes data access, allowing a busy physician to get information in seconds without knowing SQL. It also powers “smart patient profiles,” which consolidate all relevant clinical information into a single, interactive view. These profiles are dynamic summaries that go beyond static lists. For a patient with multiple chronic conditions, the profile might automatically highlight the most urgent issue, summarize the treatment history for that specific problem, and display relevant lab trends on a single graph. AI-powered “Smart Suggestions” can automatically surface issues like conflicting medications or concerning trends, accelerating medical review. Furthermore, Generative AI can assist in clinical documentation by listening to a patient-doctor conversation and generating a structured clinical note draft, freeing the clinician from the keyboard and allowing them to focus entirely on the patient.
Step 3: Apply Insights to Revolutionize Care and Operations
The real magic of real-time patient insights happens when you put them to work, changing data into action and shifting healthcare from reactive to proactive. Organizations using these insights are seeing an 80% increase in care gap closure rates, a 32% reduction in hospital readmissions, and a 5% increase in revenue capture.
When Community Health Network implemented real-time analytics, their care teams could instantly see which patients needed attention. The result was a 32% reduction in readmissions and teams focused on high-value activities instead of hunting for information. A single platform can help a nurse identify a patient at risk of sepsis, an administrator optimize staffing, and a care coordinator close documentation gaps. This was invaluable during the COVID-19 pandemic, allowing hospitals to manage resources in real-time.
Improve Patient Safety and Clinical Outcomes
Patient safety is where real-time patient insights deliver their most profound impact. The Medical University of South Carolina’s machine learning approach to sepsis detection is a prime example. By spotting subtle patterns that humans might miss, their system catches the deadly condition early, which is critical when sepsis claims 350,000 adult lives annually in the U.S. You can explore MUSC’s use of machine learning in their case study.
Beyond sepsis, AI-assisted monitoring prevents adverse events by identifying medication interactions and flagging patients at risk of falls or deterioration. For uncontrolled asthma, predictive models identify at-risk patients with 30% greater precision than traditional methods. For rare disease patients, real-time monitoring has led to a 500% greater rate of successful transition to appropriate treatments.
Enabling True Precision Medicine
Real-time patient insights are the engine of precision medicine, moving beyond one-size-fits-all treatments to care tailored to an individual’s unique genetic makeup, lifestyle, and environment. By integrating genomic data with real-time clinical information, clinicians can make highly personalized treatment decisions.
A key application is pharmacogenomics, which analyzes how a person’s genes affect their response to drugs. For example, before prescribing a common blood thinner like warfarin, a real-time platform can check the patient’s genomic data for variants in the CYP2C9 and VKORC1 genes. If a variant associated with slower metabolism is found, the system can recommend a lower starting dose, drastically reducing the risk of life-threatening bleeding. This moves prescribing from a trial-and-error process to a precise, data-driven science, applied at the point of care.
Streamline Hospital Operations and Reduce Costs
The operational benefits of real-time patient insights create efficiencies that make healthcare more sustainable.
Hospitals can now predict admission surges up to 90 minutes in advance, allowing them to adjust staffing proactively and avoid burnout. Resource optimization becomes more effective, as seen during the pandemic when hospitals with real-time visibility managed PPE and bed capacity strategically. This extends to optimizing patient flow throughout the entire hospital journey. Real-time dashboards can identify bottlenecks—such as delays in patient transport or slow room turnover—and alert managers to resolve them. Operating rooms can be scheduled more efficiently by predicting surgery durations based on historical data, minimizing downtime. Supply chain management is also transformed; instead of relying on manual inventory counts, AI can predict demand for critical supplies like medications and surgical kits based on patient case mix and upcoming procedures, preventing stockouts and reducing waste.
The financial benefits are also significant, with organizations seeing a 5% improvement in revenue capture. This improvement also comes from enhanced revenue cycle management. AI tools can analyze clinical documentation in real-time to suggest more accurate and complete medical codes (a process known as Computer-Assisted Coding), ensuring that the hospital is reimbursed appropriately for the care provided. By flagging missing documentation or potential compliance issues before a claim is submitted, these systems reduce claim denials and the administrative costs associated with appeals.
Step 4: Implement a Platform and Overcome Data Challenges
Implementing a platform for real-time patient insights is a strategic journey that requires navigating technical complexity and ethical responsibility. The core challenge is handling a constant flow of sensitive data from multiple sources securely and at scale. Scalability, data consistency, and security are foundational requirements.
Research confirms that while real-time data offers immense benefits, it also raises valid concerns about security, privacy, and infrastructure, which demand sophisticated, ongoing solutions.
Key Features for a Real-Time Insight Platform:
- Comprehensive Data Integration: Must include robust connectors for various source systems and support for batch and streaming data ingestion.
- Advanced AI/ML Capabilities: Should offer a library of pre-built healthcare models and an MLOps framework for developing, validating, and deploying custom models.
- Customizable Alerts and Dashboards: Users should be able to configure alerts based on specific clinical or operational thresholds and build role-specific dashboards.
- Interoperability Standards Support: Native support for FHIR, HL7v2, and DICOM is essential for seamless integration into existing health IT ecosystems.
- Robust Security and Privacy Controls: This includes granular, role-based access controls (RBAC), comprehensive audit trails, and data masking capabilities.
- Scalability: The architecture must be cloud-native and horizontally scalable to handle exponential growth in data volume and user concurrency.
- Federated Capabilities: The ability to train models across distributed datasets without centralizing sensitive data is critical for multi-institutional collaboration.
- User-Friendly Interface: Must include intuitive data exploration tools, natural language query interfaces, and visualization builders for non-technical users.
Choosing the Right Technology Stack
The right technology stack is the engine that powers a real-time patient insights platform. At Lifebit, we use a next-generation federated AI platform built on cloud-based infrastructure. This provides the elasticity and power to process massive amounts of data in real-time, scaling from ten patients to ten million.
The architecture relies on seamless connectivity through modern APIs and a publish-subscribe model for instant notifications. Our platform includes built-in capabilities for data harmonization and advanced AI/ML analytics, handling the complex work of translating data from dozens of sources into a unified, meaningful view. This infrastructure delivers insights rapidly and reliably when clinicians need them most.
Navigating Security, Privacy, and Compliance
Patient data requires the highest level of security and privacy, governed by regulations like HIPAA and GDPR. Balancing immediate data access with these protections is paramount.
Our strategy involves multiple layers of protection:
- De-identification: Personal identifiers are removed from data before analysis to protect patient privacy.
- Federated Governance: We bring algorithms to the data, so raw, sensitive information never leaves its secure location. Only aggregated, de-identified results are returned, ensuring data sovereignty.
- Stringent Access Controls: Only authorized personnel can access specific data, with every interaction logged and audited.
- End-to-End Encryption: Data is encrypted both in transit and at rest, making it unreadable if intercepted.
- Compliance Adherence: Our solutions are designed to meet and exceed industry standards for data protection.
Our commitment is to provide secure, real-time access for groundbreaking research and improved care within a framework of uncompromising privacy and compliance.
Overcoming Ethical Challenges and AI Bias
Beyond technical security, implementing a real-time insights platform requires a deep commitment to ethical AI. Predictive models are trained on historical data, and if that data reflects existing biases in healthcare delivery, the models can perpetuate or even amplify them. For example, if a certain demographic has historically had less access to care, a model trained on that data might incorrectly learn that they are ‘less sick,’ leading to under-resourcing their future care.
Overcoming this challenge involves a multi-pronged approach:
- Bias Detection and Mitigation: Actively auditing datasets for demographic imbalances and using advanced statistical techniques to re-weight or augment data to ensure fairness.
- Model Explainability (XAI): Using ‘explainable AI’ techniques to understand why a model made a particular prediction. A ‘black box’ model that simply flags a patient as high-risk is not enough; clinicians need to understand the contributing factors (e.g., ‘risk is high due to rising lactate and low blood pressure’) to trust and act on the insight.
- Human-in-the-Loop Governance: Establishing a clinical oversight committee to review model performance, investigate anomalous predictions, and ensure that AI-driven recommendations are always used as a tool to support, not replace, clinical judgment.
A truly responsible platform doesn’t just deliver insights; it delivers them in a way that is fair, transparent, and ethically sound.
Frequently Asked Questions about Real-Time Patient Insights
You’ve made it this far, so you probably have some practical questions about how real-time patient insights actually work in the real world. Let’s address the most common ones we hear from healthcare organizations.
What is the difference between real-time insights and a standard EHR?
Think of your EHR as a digital filing cabinet for storing and retrieving patient information. A real-time patient insights platform is different. It actively analyzes data from your EHR plus other sources like wearables and genomics as it flows in.
For example, an EHR shows a patient’s liftd white blood cell count. A real-time insights platform cross-references that with vital signs, medication history, and data from similar cases to generate a predictive alert: this patient has a 78% probability of developing sepsis in the next four hours. The EHR stores the data; the insights platform tells you what it means and what to do next.
How is patient privacy protected with constant data analysis?
Patient privacy is protected through multiple layers of security. Data de-identification is the first line of defense, stripping personal identifiers before analysis. We also use federated learning, where algorithms travel to the data, so sensitive patient information never leaves its secure home. Only aggregated insights are returned.
Combined with robust access controls, end-to-end encryption, and strict adherence to HIPAA and GDPR regulations, our platform is designed from the ground up with privacy as a non-negotiable foundation. At Lifebit, our federated model ensures your data sovereignty remains intact.
How quickly can a healthcare system start seeing benefits?
Unlike traditional enterprise technology projects that take years, benefits from modern real-time patient insights platforms can appear in weeks. A hospital can deploy predictive models for sepsis or readmission risk in a single department and see measurable improvements in patient outcomes within the first few months.
The 32% improvement in sepsis detection or 32% reduction in readmissions we mentioned are real results organizations have achieved relatively quickly. The key is that ROI grows over time as you integrate more data and deploy more models. You start with quick wins and build momentum, with benefits accumulating from day one.
Conclusion: The Future of Healthcare is Happening in Real-Time
The future of healthcare isn’t on the horizon; it’s being built today, powered by real-time patient insights. This shift from reactive to proactive care is a complete reimagining of what’s possible.
By unifying fragmented data and applying AI, we can predict problems before they become crises. By putting these insights directly into the hands of clinicians, we give them the ability to act on information that matters, precisely when it matters most. The results—an 80% increase in gap closure rates, a 32% reduction in readmissions, and a 32% improvement in sepsis detection—represent real people receiving better care.
This creates a cultural shift toward data-driven decision-making, empowering every member of the care team and creating a healthcare system that’s finally working the way it should.
At Lifebit, our next-generation federated AI platform provides the foundation for this future. Through our Trusted Research Environment (TRE), Trusted Data Lakehouse (TDL), and R.E.A.L. (Real-time Evidence & Analytics Layer), we deliver the real-time insights and AI-driven safety surveillance that make proactive, efficient healthcare possible at scale.
The future is here. We’d love to help you be part of it.

