AI in Clinical Trials: Smart Solutions for Faster Recruitment

AI clinical trial recruitment: Transform 2025
Why Clinical Trial Recruitment is Healthcare’s Biggest Bottleneck
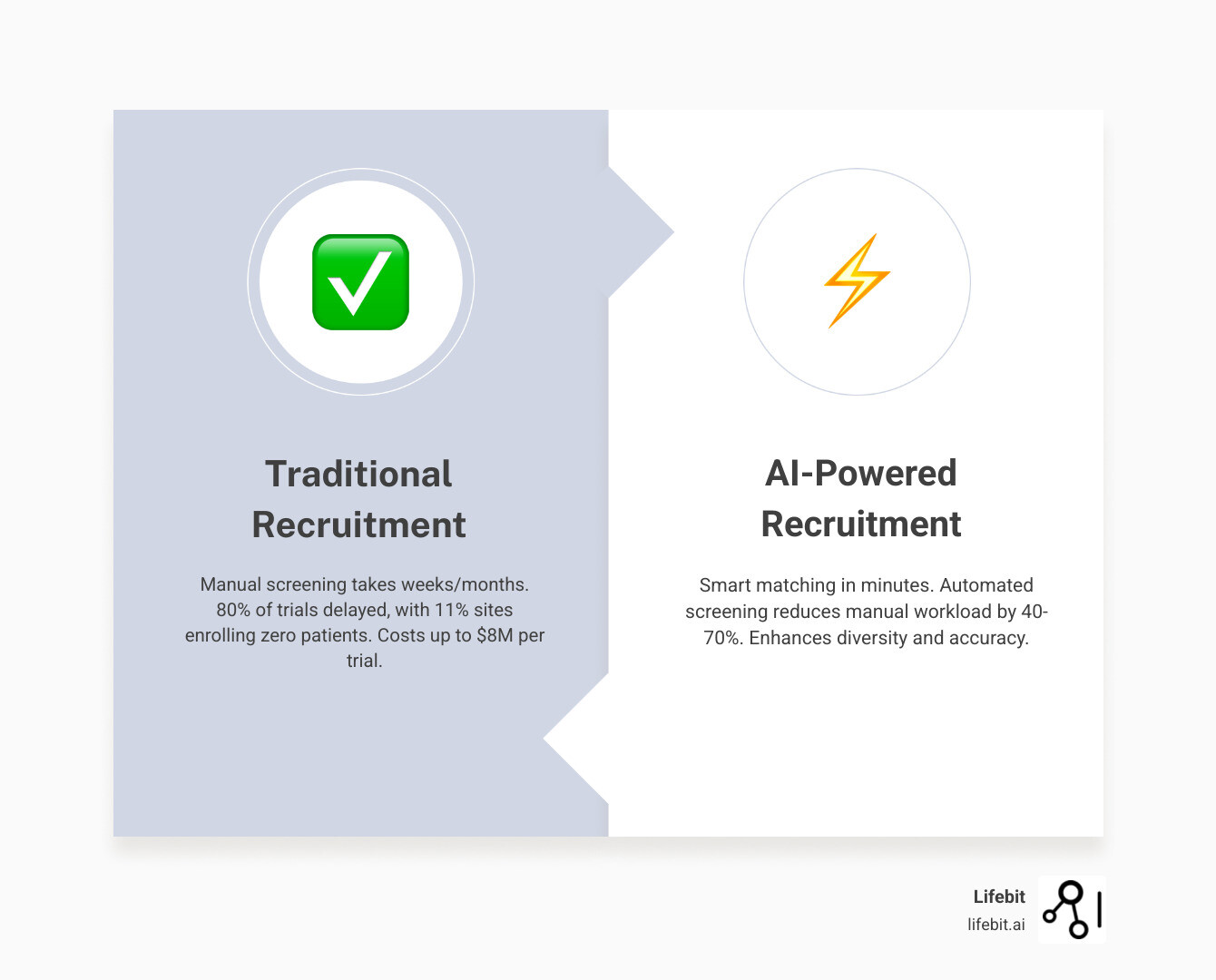
AI clinical trial recruitment is revolutionizing how research institutions identify, match, and enroll patients for clinical studies. Traditional methods are failing, with 80% of trials facing delays and 11% of sites enrolling zero patients. These struggles can cost up to $8 million per trial, delaying life-saving treatments.
Artificial intelligence addresses these challenges by:
- Smart patient matching: Using machine learning to analyze electronic health records.
- Automated screening: Reducing manual workload by up to 70%.
- Predictive modeling: Identifying patients likely to enroll and complete trials.
- Real-time alerts: Notifying research teams of eligible patients instantly.
- Improved diversity: Reaching underrepresented populations with data-driven targeting.
The problem stems from manual processes and limited databases, where research coordinators spend countless hours sifting through records, often missing qualified candidates. AI technologies like machine learning and natural language processing analyze vast datasets—including EHRs, genomic data, and real-world evidence—to find patients with best speed and accuracy. What once took months now happens in minutes.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. For over 15 years, I’ve focused on developing AI-powered platforms for AI clinical trial recruitment. Our federated data analysis platform helps pharmaceutical companies and public health institutions accelerate patient recruitment while ensuring the highest standards of data privacy and security.
AI clinical trial recruitment terms to learn:
- clinical trial recruitment strategies
- digital clinical trial recruitment
- clinical trial recruitment digital results
The Bottleneck in Medical Progress: Why Traditional Clinical Trial Recruitment Fails
Traditional clinical trial recruitment is the single biggest obstacle standing between medical breakthroughs and patients. Outdated methods rely on manual screening processes, where research teams spend countless hours sifting through patient charts. This approach is time-consuming, error-prone, and often misses qualified candidates whose eligibility criteria are buried in unstructured clinical notes.
The numbers tell a sobering story. Eighty percent of clinical trials face delays due to recruitment, with some studies doubling their original timelines. Furthermore, 37% of trial sites miss their enrollment goals, and 11% fail to enroll a single patient. These delays are not just operational hiccups; they are systemic failures. Each delayed day can cost sponsors between $600,000 and $8 million, according to research on trial costs.
Several factors contribute to this bottleneck:
- Complex Protocols: Modern trials have dozens of specific, layered inclusion and exclusion criteria. A single oncology trial, for instance, might require a specific genetic mutation (e.g., EGFR), a certain stage of cancer, a history of specific prior treatments, and lab values within a narrow range. Manually cross-referencing these intricate requirements across thousands of patient records is not just slow; it’s a recipe for human error, leading to high screen failure rates and wasted resources.
- Lack of Diversity: Recruitment traditionally centers around major academic medical centers, inadvertently excluding rural populations and minority ethnic groups who may have less access to these facilities. This creates homogenous trial cohorts that do not reflect the real-world patient landscape. For example, African Americans make up 13% of the U.S. population but only 5% of clinical trial participants. This is not only an ethical failure but a scientific one, as genetic and socioeconomic factors can influence drug efficacy and safety, undermining the generalizability of research findings.
- Low Awareness and Physician Burden: Many eligible patients are simply unaware of trials that could benefit them. Traditional outreach methods like flyers and general advertising are often ineffective. Furthermore, primary care physicians and specialists are often too overwhelmed with clinical duties to stay updated on all relevant trials, meaning they may not refer eligible patients. This communication gap is a major barrier, as organizations still rely on outdated Clinical Trial Recruitment Strategies.
These inefficiencies carry a high cost, both financially and in human terms. Billions are wasted on recruitment efforts, and promising studies may fail before completion. This delayed drug development means patients wait longer for potentially life-saving treatments. For someone with an aggressive cancer or a degenerative condition, these delays can drastically impact quality of life and survival outcomes.
Moreover, the lack of diversity in trial populations creates medical inequality and generalizability issues. Treatments developed from unrepresentative data may be less effective for certain demographic groups, perpetuating health disparities. Physicians need confidence that trial data applies to their diverse patient populations, and a lack of diversity erodes this trust. Innovations in Digital Clinical Trial Recruitment are essential to address these deep-seated problems, paving the way for AI clinical trial recruitment to create a more efficient and equitable future.
How AI Transforms Patient Recruitment: From Manual Searches to Smart Matching

AI clinical trial recruitment shifts the paradigm from reactive searching to proactive, intelligent matching. Instead of waiting for patients to respond to ads, AI actively hunts through vast data repositories to find ideal candidates. This is like having a brilliant research assistant who can read thousands of medical records in minutes and perfectly recall complex trial criteria. Learn more about how we apply AI for Clinical Trials.
Opening up Patient Data with Machine Learning and NLP
Healthcare systems hold vast amounts of patient information, but much of it is locked in unstructured formats. While Electronic Health Records (EHRs) contain structured data like lab results, the real insights often lie in unstructured text: clinician notes, pathology reports, and discharge summaries.
This is where AI’s core technologies make a difference:
- Machine Learning (ML) algorithms act as rapid pattern-recognition systems. They evaluate thousands of variables in seconds to create shortlists of eligible candidates, learning from each match to improve future recommendations.
- Natural Language Processing (NLP) allows computers to “read” and understand the complex, nuanced language in medical notes. It goes beyond simple keyword searching. For example, when a doctor writes, “Patient reports mild fatigue lasting 3 months, but no history of cardiac issues. Father had MI at 55,” a sophisticated NLP model can perform several tasks simultaneously. It extracts the symptom (fatigue), its severity (mild), and its duration (3 months). Crucially, it understands negation (“no history of cardiac issues”) to correctly apply an exclusion criterion. It can also identify and contextualize family history (“Father had MI”), distinguishing it from the patient’s own medical history. This is vital, as a vast majority of trial inclusion and exclusion criteria—up to 80% by some estimates—are documented exclusively in these unstructured narrative notes.
By integrating data from EHRs, genomic databases, and lab systems, AI creates comprehensive patient profiles, revealing candidates missed by siloed data analysis. Our approach to Real-World Data shows how this accelerates chart review. For example, the NIH-developed TrialGPT algorithm helped clinicians spend 40% less time screening patients with the same accuracy, as detailed in NIH research on TrialGPT.
Precision Matching and Engagement
Once AI understands the data, it performs precision matching. This involves two key steps. First, protocol parsing uses AI to automatically read and deconstruct a lengthy, human-readable trial protocol into a set of structured, machine-readable rules. It identifies every inclusion and exclusion criterion, from lab value ranges to specific comorbidities. Second, the AI compares these rules against the comprehensive patient profiles it has built. This process evaluates hundreds of data points for every patient instantly, creating a highly accurate shortlist of potential candidates. This precision dramatically reduces screen failure rates—which can be as high as 50% in traditional recruitment—by ensuring that only the most qualified patients are flagged for review, sometimes improving accuracy by over 70%.
Real-time alerts notify teams the moment an eligible patient is identified, enabling rapid outreach. We are constantly Enhancing Clinical Trial Matching with Lifebit Patient Management to provide these capabilities.
Real-World Impact: AI in Action
The application of these technologies is not theoretical. For example, a major pharmaceutical company running a trial for a new non-small cell lung cancer (NSCLC) drug needed to find patients with a rare ALK mutation who had not responded to a specific first-line therapy. Manually searching through records across multiple hospitals was projected to take over a year. By deploying an AI platform, they were able to:
- Integrate Data: Securely access and harmonize EHR data from three different hospital networks.
- Apply NLP: Scan millions of unstructured pathology reports and clinician notes to identify mentions of ALK testing and prior therapies.
- Execute Precision Matching: Cross-reference the NLP findings with structured data on diagnosis codes and medication history.
The result? The AI system identified a cohort of 75 highly-qualified potential participants in under two weeks, allowing the trial to start six months ahead of schedule. This acceleration directly translates into getting a potentially life-saving therapy to patients faster.
Finding patients is only half the battle. AI also improves engagement and retention. AI-powered communication tools like chatbots provide 24/7 support, while personalized outreach and automated reminders improve compliance. AI can even monitor engagement to identify patients at risk of dropping out, allowing teams to intervene. This is especially valuable for decentralized clinical trials, where AI manages complex data streams and communication to create a seamless patient experience. Our Decentralized Clinical Trials Guidance explores this further.
The Tangible Benefits of Using AI for Clinical Trial Recruitment
The shift to AI clinical trial recruitment delivers immediate and transformative results. It turns a reactive, hit-or-miss process into a precise, data-driven strategy with measurable benefits: recruitment timelines cut by months, screening accuracy improved by 70%, and patient diversity dramatically increased. These Innovations in Clinical Trial Recruitment and Enrollment accelerate the entire drug development pipeline, bringing breakthrough treatments to patients sooner.
Accelerating Timelines and Reducing Costs
AI’s speed is a game-changer. Where manual reviews take weeks, AI analyzes thousands of patient records in minutes. Automated screening is the engine of this efficiency, as algorithms evaluate complex inclusion and exclusion criteria across massive datasets with superior precision. This instantly flags truly eligible candidates for review.
The cost savings are a direct result of this speed. By shortening recruitment timelines, AI attacks the high costs of trial delays, which can reach $8 million per trial. It eliminates the need for expensive, broad-based advertising campaigns and frees up research staff from tedious manual chart reviews. This resource optimization allows teams to focus on high-value tasks like patient engagement and data analysis, ensuring a quicker path to market for new therapies.
Improving Trial Diversity and Data Quality
AI also addresses the long-standing diversity problem in clinical research. Traditional methods often recruit from a convenient but limited pool of patients. AI casts a much wider net, analyzing patient populations across multiple healthcare systems to identify eligible participants from diverse backgrounds, including those in rural or underserved communities.
This broader recruitment approach directly improves the generalizability of research findings. When trial populations reflect the real world, the results are more robust and applicable across different groups. This leads to reduced bias and higher data quality, which is critical for ensuring new treatments are safe and effective for everyone. AI’s ability to identify patients with very specific profiles—genetic, clinical, or demographic—allows researchers to build cohorts that are both diverse and precisely targeted, as seen in our work on AI-Powered Biomarker Findy.
Navigating the New Frontier: Ethical Considerations and Future Trends
As AI clinical trial recruitment enters the mainstream, it’s crucial to steer this new frontier ethically and responsibly. The power of AI brings incredible possibilities, but it requires a thoughtful approach to protecting patients and ensuring fairness.
Upholding Ethics in AI-Driven Recruitment
Protecting patients is about honoring the trust they place in medical research. Data privacy is central to this, and our platforms operate within secure environments that adhere to strict regulations like HIPAA. There is no room for shortcuts with personal health information.
Another key challenge is algorithmic bias. AI systems learn from historical data, which unfortunately reflects decades of systemic healthcare inequities. For example, if a certain demographic has historically been undertested for a specific biomarker due to socioeconomic factors, an AI model trained on this data might learn to deprioritize that group for trials requiring that marker, even if they are otherwise eligible. This would not only perpetuate the bias but also make it invisible and seemingly objective. To combat this, fairness and transparency are essential. This involves more than just good intentions; it requires proactive measures like conducting regular bias audits, using fairness-aware machine learning techniques that can adjust for data imbalances, and ensuring that the algorithms’ decision-making processes are explainable to clinicians and ethics boards. We continuously test and adjust our algorithms to ensure they promote equity, not just efficiency.
Our Trusted Research Environments are designed with this philosophy in mind. They allow researchers to gain insights from sensitive data without directly accessing individual patient information. This approach, combined with robust Clinical Data Governance, ensures that innovation and privacy go hand in hand.
The Future of AI Clinical Trial Recruitment
The future of AI clinical trial recruitment will reshape medical research entirely. Several emerging technologies are leading the way:
- Digital twins: These are not just static models but dynamic, virtual simulations of an individual patient’s physiology, built from their integrated health data (genomic, clinical, imaging). In the context of recruitment, a digital twin could be used to pre-screen a patient’s likely response to an investigational drug, helping to select candidates who are most likely to benefit and least likely to experience adverse effects. This could revolutionize trial design, especially for rare diseases where every participant is precious.
- Generative AI: Beyond systems like TrialGPT that analyze data, generative AI will create new content to improve the patient experience. Imagine an AI that generates a personalized video explaining a complex trial protocol in simple terms, tailored to a patient’s specific language and health literacy level. It could also power interactive chatbots that can answer complex, context-specific questions about the trial, improving informed consent and patient engagement.
- Federated Data Analysis: This is a critical long-term trend for scaling AI recruitment globally. Instead of pooling sensitive patient data into a central repository—a major privacy and logistical hurdle—federated learning allows AI models to be sent to the data. The model trains locally on the hospital’s data behind its firewall, and only the anonymous insights and model updates are shared. This enables AI to learn from diverse, international datasets without compromising patient privacy, unlocking a truly global patient pool.
The ultimate goal is true AI for Precision Medicine, matching the right patient to the right trial based on their unique genetic and clinical profile. Continuous learning models will evolve from static tools into dynamic partners that get smarter with every interaction, creating a feedback loop that accelerates medical breakthroughs. To learn more, explore our insights on Emerging Trends and Technologies in Clinical Trial Design.
Frequently Asked Questions about AI in Clinical Trial Recruitment
As this technology becomes more widespread, many researchers and healthcare professionals have questions. Here are answers to some of the most common ones about AI clinical trial recruitment.
How does AI find patients for clinical trials?
AI algorithms analyze vast datasets, particularly electronic health records (EHRs), to find individuals matching a trial’s specific criteria. The key is Natural Language Processing (NLP), which allows AI to “read” and understand unstructured data like doctors’ notes and pathology reports. This open ups critical information not found in standard database fields, identifying eligible patients who would otherwise be missed by manual searches.
Can AI help recruit for rare diseases?
Yes, this is one of AI’s most powerful applications. Recruiting for rare diseases is incredibly challenging due to small, geographically dispersed patient populations. AI clinical trial recruitment excels here by scanning large, multi-source health datasets simultaneously. By analyzing unstructured clinical notes where nuanced symptoms are often recorded, AI can identify these hard-to-find patients far more effectively than traditional methods, making previously difficult trials feasible.
Is using AI for patient recruitment safe and private?
Absolutely. Patient privacy and data security are non-negotiable. Reputable AI solutions operate within secure, compliant frameworks like Trusted Research Environments that strictly adhere to regulations like HIPAA and GDPR. A key technique is data federation, which allows AI to analyze data without it ever leaving its secure source location. This provides powerful insights while ensuring sensitive patient information remains protected. Furthermore, algorithms are continuously audited to prevent bias and ensure fair, equitable patient selection.
Conclusion
The future of medical research is here, powered by artificial intelligence. AI clinical trial recruitment is solving one of healthcare’s most persistent bottlenecks, changing how we find, match, and engage patients for clinical studies.
We have moved from an era of manual reviews and missed enrollment targets to one of smart, data-driven precision. AI makes recruitment faster and fundamentally better. By analyzing vast datasets with machine learning and NLP, AI uncovers eligible patients within electronic health records and reaches underrepresented populations, creating more diverse and representative trial cohorts.
The results are clear: AI accelerates timelines, reduces costs, and brings life-saving treatments to patients faster. This is more than an efficiency gain; it’s building a more equitable future for medical research by ensuring treatments work for everyone.
At Lifebit, we are at the forefront of this revolution. Our federated AI platform allows researchers to harness the power of AI while upholding the highest standards of data privacy and security. Through our Trusted Research Environments, we help organizations open up the potential of global biomedical data safely and responsibly.
The path forward is intelligent, diverse, and patient-centered. Together, we are making that future a reality.


