The A to Z of Patient Registries

What are patient registries: The Ultimate 2025 Guide
What are Patient Registries and Why Do They Matter?
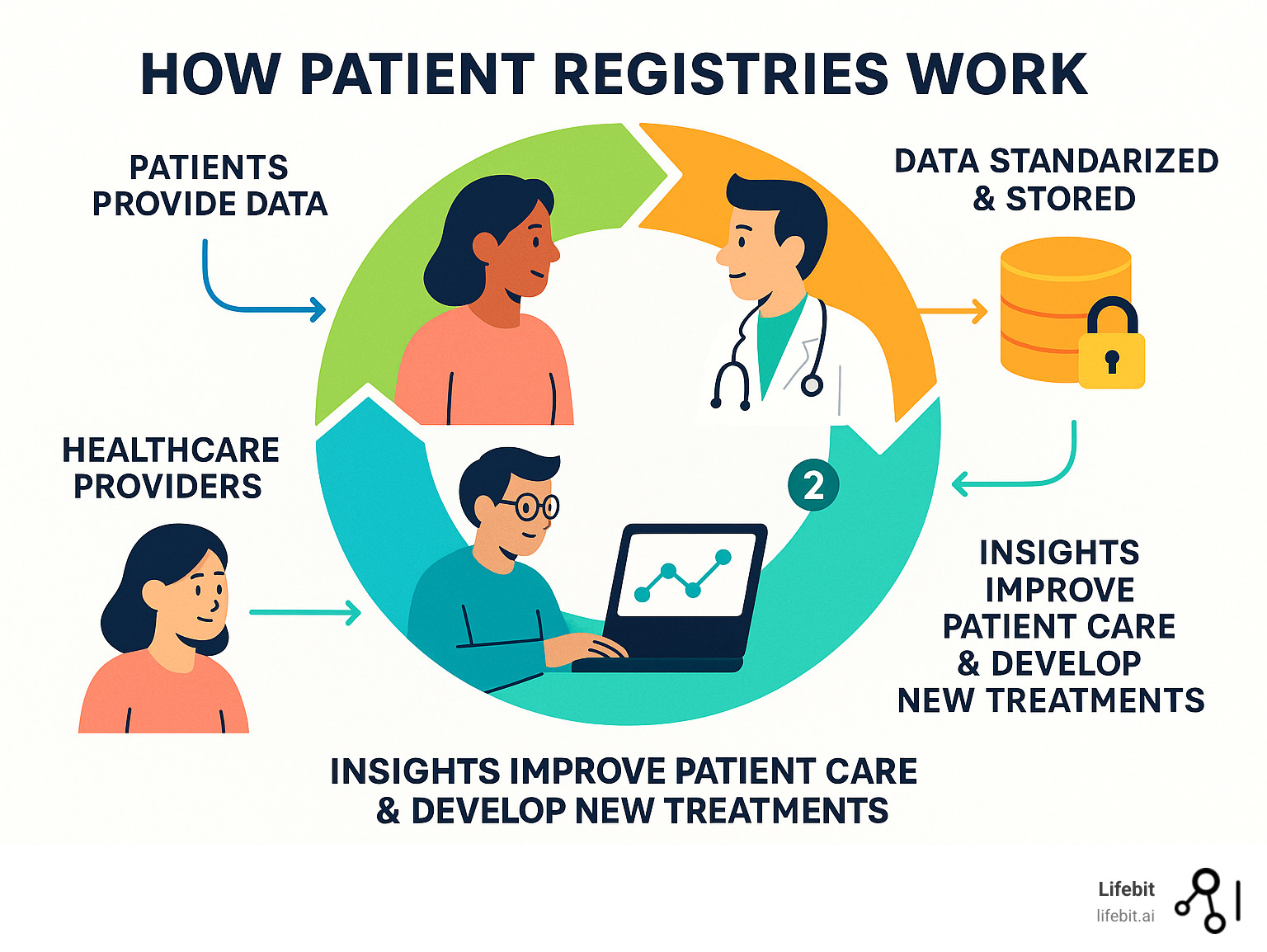
What are patient registries and how do they transform healthcare research? A patient registry is an organized system that collects uniform data about patients with specific diseases, conditions, or treatments to improve medical care and advance research.
Quick Answer:
- Definition: Databases that systematically collect standardized health information from patients
- Purpose: Track disease progression, monitor treatment safety, and improve patient outcomes
- Types: Disease registries (cancer, rare diseases), product registries (drugs, devices), and health services registries
- Data: Demographics, symptoms, treatments, quality of life, and patient-reported outcomes
- Benefits: Enable real-world research, connect patients to clinical trials, and accelerate drug development
Patient registries are the backbone of modern healthcare research, turning individual experiences into collective insights. Unlike clinical trials, which test treatments under controlled conditions, registries capture real-world data from everyday medical practice. This makes them invaluable for understanding rare diseases, tracking long-term treatment effects, and identifying safety signals missed in shorter studies.
For example, the British Thoracic Society’s registry on over 5,700 patients helps doctors compare treatments and researchers understand disease patterns. This data empowers patients to contribute to science, potentially gaining access to clinical trials, while helping healthcare systems improve care quality.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. With over 15 years in biomedical data, I’ve seen how well-designed patient registries, supported by federated analysis, can revolutionize precision medicine.
Key what are patient registries vocabulary:
What are Patient Registries and How Do They Work?
Understanding what are patient registries starts with seeing them as sophisticated systems that collect uniform information from specific patient groups over time. Unlike clinical trials, registries use observational study methods to capture what naturally happens during routine medical care. This approach gathers real-world data (RWD), reflecting how diseases and treatments perform in everyday practice, outside the highly controlled environment of an experiment.
A registry is more than a database; it’s a structured system with a predetermined scientific, clinical, or policy purpose, as highlighted in the Official AHRQ Definition. Goals range from understanding a rare disease’s natural history to evaluating treatment safety, assessing the quality of care, or informing public health decisions. Every piece of data collected is tied to a specific research question or objective.

For a deeper dive, explore What are Patient Registries and Why Are They Important?.
The Different Types of Patient Registries
Registries are custom-built to answer different questions, generally falling into several key categories:
- Disease registries focus on patients with a specific condition. They are fundamental for understanding a disease’s natural history, identifying risk factors, and tracking outcomes over time. For example, the Cystic Fibrosis Foundation Patient Registry, started in 1966, has been instrumental in tracking the health of individuals with CF, leading to dramatic improvements in life expectancy. Other examples include the British Thoracic Society’s IPF registry and the CoRDS Ataxia Patient Registry.
- Product registries (or exposure registries) follow patients exposed to specific drugs, biologics, or medical devices. These are vital for post-market safety monitoring, allowing regulators and manufacturers to identify rare or long-term side effects that may not have appeared in pre-market clinical trials. For instance, a registry for a new joint replacement device could track thousands of patients for decades to monitor device failure rates.
- Health services registries track patients undergoing specific procedures or receiving care within a particular healthcare system. Their goal is often quality improvement. By collecting data on processes and outcomes, they help organizations compare performance against benchmarks and identify best practices. The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) is a prime example, helping hospitals reduce surgical complications.
- Patient-Powered Registries (PPRs) represent a paradigm shift, placing patients at the center of the research process. In these registries, like PatientsLikeMe, patients not only contribute their data but also help govern the registry and set research priorities. This model ensures that the research is relevant to the patient community’s needs and fosters a strong sense of engagement and ownership.
Patient Registries vs. Clinical Trials: A Key Distinction
While both are crucial for medical advancement, their methodologies and purposes differ significantly. Clinical trials are controlled experiments designed to test a specific intervention (like a new drug) against a control group to establish cause and effect. They are the gold standard for proving a treatment’s safety and efficacy for regulatory approval. Patient registries are typically observational, documenting routine medical care to capture Real-World Evidence (RWE) on how treatments work across diverse, unselected populations.
| Feature | Patient Registries | Clinical Trials |
|---|---|---|
| Purpose | Observe outcomes, monitor safety, and assess real-world effectiveness | Test specific interventions to establish safety and efficacy |
| Data | Real-world data from routine clinical practice | Highly structured data collected according to strict protocols |
| Setting | Diverse real-world environments (hospitals, clinics) | Controlled research settings |
| Population | Broad, heterogeneous patient populations | Narrow, highly selected patient populations |
| Intervention | None – reflects existing care | Introduction of a specific intervention |
The two are not mutually exclusive; they are highly complementary. Registries can be used to identify eligible and willing participants for clinical trials, dramatically speeding up recruitment. Data from a registry can also provide crucial context for interpreting trial results, showing how a drug’s performance in a controlled setting translates to the real world. In some cases, particularly for rare diseases where a placebo-controlled trial may be unethical or infeasible, a well-curated patient registry can even serve as an external or synthetic control arm, providing a comparison group for a single-arm trial.
The Core Purposes and Widespread Uses of Patient Registries
In practice, what are patient registries? They are dynamic engines for healthcare improvement. They bridge individual patient experiences and broader medical understanding by describing the natural history of disease, determining real-world clinical effectiveness, measuring quality of care, and conducting pharmacovigilance (monitoring drug safety). Their applications are vast, influencing everything from basic research to national health policy.

The Core Purposes of Patient Registries: What are they and why do they matter?
The primary goals of patient registries address key healthcare challenges:
- Understanding the Natural History of Disease: Especially for rare diseases, registries are often the only way to gather enough data to understand how a condition progresses over time without treatment. By pooling data from patients globally, researchers can achieve the statistical power needed to identify disease patterns, risk factors, and prognostic indicators. It’s no surprise that 45% of disease advocacy organizations support a registry. For more, see Four Benefits of Patient Registries for Rare Diseases.
- Tracking Long-Term Outcomes and Effectiveness: Clinical trials are typically short-term. Registries can follow patients for years or even decades, capturing invaluable insights about the long-term effectiveness and durability of treatments. For example, a registry for patients with joint replacements can track device performance over 20 years, identifying models with higher-than-expected failure rates long after they hit the market.
- Improving Quality of Care: Health services registries are powerful tools for quality improvement. They operate on an audit-and-feedback loop: hospitals and clinics contribute data on their procedures and outcomes, which is then benchmarked against national or regional averages. This allows institutions to identify areas for improvement, adopt best practices from top performers, and ultimately enhance patient safety. The British Thoracic Society’s registry, with data on 5,759 patients, is a prime example of this in action.
- Supporting and Accelerating Research: Registries are a foundational resource for the entire research ecosystem. They generate hypotheses for new studies, provide a pre-screened pool of potential participants for clinical trials, and supply the real-world data needed to validate findings from basic science.
How Registries Accelerate Research and Drug Development
Patient registries actively speed up the journey from scientific question to patient treatment in several key ways:
- Streamlining Clinical Trial Recruitment: Finding and enrolling eligible patients is one of the most time-consuming and expensive parts of a clinical trial. A patient registry provides a ready-made, engaged cohort of potential participants who have already consented to be contacted for research, drastically reducing recruitment timelines and costs.
- Enabling Real-World Control Arms: For rare diseases or orphan drugs, conducting a traditional placebo-controlled trial can be unethical or logistically impossible. High-quality registry data can be used to create a historical or synthetic control arm. This allows researchers to compare the outcomes of patients receiving a new therapy against a carefully matched group of patients from the registry representing the natural course of the illness.
- Critical Post-Market Safety Monitoring (Pharmacovigilance): A drug’s safety profile is never fully known at the time of approval. Registries act as an essential early warning system, tracking how drugs and medical devices perform in a large, diverse population after they are on the market. They can detect rare side effects, identify risks in specific patient subgroups (e.g., the elderly), and provide the evidence needed for regulatory actions like label updates or market withdrawals.
Informing Healthcare Policy and Clinical Guidelines
Beyond research, registry data provides the real-world evidence necessary to shape healthcare policy and clinical practice. Payers, including government bodies like Medicare and private insurers, use registry data to make coverage decisions, assessing whether a new treatment provides value in a real-world setting. Furthermore, professional medical societies rely on evidence from registries to develop and update their clinical practice guidelines, ensuring that recommendations for patient care are based on the most current and comprehensive data available on treatment outcomes across the population.
Navigating the Patient Registry Ecosystem: From Participation to Protection
Joining a patient registry is a significant contribution to medical science, but it’s natural to have questions about privacy and data use. The patient registry ecosystem is built on a foundation of trust, supported by four pillars: patient empowerment, regulatory oversight, robust data security, and clear informed consent. These elements work in concert to protect participants while maximizing the research impact of their contributions.

The Patient’s Role: Benefits and How to Get Involved
Participating in a registry is an act of empowerment. By sharing your health journey, you transform personal experience into powerful data that can help researchers uncover hidden disease patterns, identify effective treatments, and move closer to a cure. The benefits extend beyond altruism; participants often gain access to the latest research findings, learn about clinical trial opportunities, and connect with a supportive community of others facing similar health challenges.
Getting involved is often straightforward. A great first step is to talk to your healthcare provider or a specialist involved in your care. Patient advocacy groups are also invaluable resources, as they frequently sponsor or partner with registries. You can also search major databases to find a relevant registry:
- OrphaNet for a comprehensive directory of resources for rare diseases.
- TREAT-NMD for a global network of registries for neuromuscular conditions.
- NIH Registries for a broad, U.S.-focused list maintained by the National Institutes of Health.
The Regulatory Landscape: FDA and EMA Oversight
Reputable registries operate within a robust framework of regulatory oversight. In the United States, the Food and Drug Administration (FDA) increasingly relies on registries as a source of Real-World Evidence (RWE), a shift accelerated by the 21st Century Cures Act. The European Medicines Agency (EMA) has similar initiatives, providing formal guidance on how registry data can be used to support regulatory decision-making, from initial drug approvals to post-approval safety assessments.
Initiatives like the FDA’s Patient-Focused Drug Development (PFDD) use registry data to ensure the patient’s lived experience is a core component of the drug development process. After a product is approved, registries become vital for post-approval safety monitoring, tracking long-term effects in diverse populations that were not fully represented in clinical trials. For more details, see the EMA guidance on patient registries and learn More info about Disease Registers.
Ensuring Data Privacy, Security, and Quality
Your trust is the bedrock of any successful registry. To earn and maintain that trust, registries employ a multi-layered strategy to protect sensitive health information.
1. Data Privacy and Informed Consent
Privacy protection is paramount. Before any data is collected, you must go through an informed consent process. This involves a clear, easy-to-understand explanation of the registry’s purpose, how your data will be used, who might access it, and the risks and benefits of participating. It also affirms your right to withdraw at any time. To protect your identity, data is de-identified by removing personal details like your name and address, a process governed by strict regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in Europe.
2. Data Security and Governance
Robust technical and administrative safeguards protect the data itself. Secure databases use state-of-the-art encryption (both for data at rest and in transit) and strict access controls to prevent unauthorized viewing. Modern platforms, like Lifebit’s Trusted Research Environment, are designed to meet the highest global security standards (e.g., ISO 27001, SOC 2). A formal data governance framework, overseen by a Data Access Committee (DAC), establishes clear rules for who can access the data and for what purpose, ensuring every research request is vetted and aligned with the registry’s mission.
3. Ensuring High-Quality Data
For research to be reliable, the underlying data must be accurate, complete, and consistent. Registries ensure high-quality data through several mechanisms. They use standardized data collection forms and Common Data Elements (CDEs) to ensure every site collects the same information in the same way. Automated validation checks are built into the data entry system to catch errors in real-time. Data managers also perform regular quality checks and curation to produce a research-ready dataset. Learn more about the technical needs in Four Key Patient Registry Software Requirements.
The Future of Registries: Overcoming Challenges with Technology
The world of patient registries is evolving rapidly. While their value is undisputed, traditional registries face significant operational challenges. The future lies in leveraging emerging technologies to make registries more sustainable, interoperable, and capable of advanced analytics, all while strengthening patient privacy and engagement.

What are the challenges and concerns associated with patient registries?
Understanding what are patient registries up against is key to appreciating new solutions. Major hurdles include:
- Funding and Sustainability: Establishing and maintaining a high-quality registry is expensive. Many rely on short-term academic or government grants, leading to a constant struggle for funding. The future requires a shift toward sustainable models, such as public-private partnerships or industry consortia.
- Data Standardization and Interoperability: Historically, registries have used different data formats and definitions. This creates data silos, making it difficult or impossible to combine insights from multiple sources. Without interoperability, the potential for large-scale, global research is severely limited.
- Patient Recruitment and Retention: Finding eligible patients and keeping them engaged for long-term follow-up is a persistent challenge. Participant burden from lengthy surveys and clinic visits can lead to high dropout rates, compromising the registry’s long-term value.
- Data Quality: The principle of “garbage in, garbage out” is highly relevant. Ensuring that data collected from multiple sites is accurate, complete, and consistent requires significant investment in training, data curation, and quality control processes.
These challenges highlight the need for smarter, more technologically advanced approaches. For more, see Challenges Facing Patient Registries in the US.
The Future is Federated: AI, Big Data, and Global Collaboration
The future of what are patient registries can accomplish is being reshaped by federated data networks, artificial intelligence, and global collaboration.
Federated Networks: This technology is a game-changer for privacy and collaboration. Instead of pooling sensitive patient data into a central database, the federated model “brings the analysis to the data.” Researchers can run analyses across multiple registries located in different hospitals or even different countries, but the data itself never leaves its secure, local environment. This approach maximizes security, respects data privacy laws like GDPR, and enables unprecedented global collaboration.
AI and Machine Learning: By applying AI and ML algorithms to the vast, connected datasets made accessible through federation, researchers can uncover complex patterns that are invisible to the human eye. These tools can be used to build predictive models for disease progression, identify novel patient subgroups (phenotypes), and discover new biomarkers for diagnosis or treatment response.
Linking Diverse Data Sources: The true power of a registry is unlocked when its data is linked with other information. The future involves connecting registry data with Electronic Health Records (EHRs), genomic and proteomic data, medical imaging, and even real-time data from wearables. This creates a rich, multi-dimensional view of the patient journey, enabling a more holistic understanding of health and disease.
Global Collaboration: For rare diseases, no single country has enough patients for a meaningful study. Federated technology makes it possible to pool data virtually from multiple countries, achieving the statistical power needed for groundbreaking research. Initiatives like Data Saves Lives are building the public trust and policy frameworks needed for these collaborations. The technology to enable this future exists today, creating smarter, more connected systems that turn patient experiences into life-changing findings. Learn more about High-Quality Patient Registries: Establishment and Best Practices.
Frequently Asked Questions about Patient Registries
Here are straightforward answers to common questions about what are patient registries.
What kind of information is collected in a patient registry?
Registries collect comprehensive information to create a detailed picture of a health journey. This typically includes:
- Demographics: Age, gender, and ethnicity to understand how diseases affect different populations.
- Clinical data: Diagnosis details, symptoms, medical history, and test results.
- Treatment history: Medications, surgeries, and other therapies.
- Quality of life and patient-reported outcomes (PROs): Data captured directly from you about your well-being, symptoms, and how a condition impacts daily life.
Secure contact information may also be collected with your permission to share updates or research opportunities.
Is my data safe in a patient registry?
Yes. Reputable registries prioritize data security. Your information is protected by:
- Strict privacy rules: Registries must comply with laws like HIPAA in the U.S. and GDPR in Europe.
- De-identification: Your personal identifying information (name, address) is removed or encrypted before being used for research.
- Informed consent: You receive a clear explanation of how your data will be used and protected before you agree to participate.
- Secure technology: Data is stored in encrypted databases with strict access controls. Federated platforms like Lifebit’s add another layer of security by allowing analysis without moving the data.
Can I withdraw from a patient registry after joining?
Absolutely. Your participation is always voluntary. You have the right to withdraw consent at any time, for any reason, without needing to provide an explanation. The informed consent document you sign at the beginning will explain the simple process for withdrawal. Once you withdraw, your data will not be used in any future research.
Conclusion
Understanding what are patient registries reveals one of healthcare’s most powerful tools for turning individual patient experiences into collective wisdom. They capture the real-world data that tells the true story of how diseases progress and how treatments work outside of a lab.
This evidence is already helping to develop safer drugs and guide better clinical decisions. However, the full potential of registries is still being open uped. Challenges like data silos and funding problems have slowed progress, but technology is providing powerful solutions.
The future is federated. This approach allows data to be analyzed securely in its original location, enabling global collaboration without compromising patient privacy. With federated networks, AI can uncover insights from worldwide data, accelerating the pace of findy.
At Lifebit, we are building this future. Our federated platform enables researchers to securely analyze registry data across continents, turning patient contributions into life-changing therapies faster than ever before.
Ready to see how cutting-edge technology is changing patient registry research? Explore Learn more about Lifebit’s federated data platform and find how we’re helping build a healthier tomorrow, one secure insight at a time.

