Cancer Explained – From Cells Gone Wild to Treatment Options

Understanding Cancer: From Basics to Hope
Cancer is a group of diseases defined by the uncontrolled growth of abnormal cells that can spread to other parts of the body. While it affects 1 in 3 people in their lifetime and caused nearly 10 million deaths worldwide in 2020, there is significant reason for hope.
Key Cancer Facts:
- Global Impact: A leading cause of death, accounting for 1 in 6 deaths globally.
- Common Types: Breast, lung, colorectal, and prostate cancers are the most prevalent.
- Causes: A mix of genetic, lifestyle, and environmental factors.
- Prevention: 30-50% of cancers are preventable through lifestyle changes.
- Survival: The average 5-year survival rate in the U.S. is 66%, reflecting major progress in detection and treatment.
Fewer people are dying from cancer today than 20 years ago. This guide explains how cancer develops, the risk factors you can control, and the latest breakthroughs in treatment and research.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. With over 15 years in computational biology and genomics, my work focuses on powering cancer research through secure, federated data analysis, connecting researchers with the data needed to treat cancer more effectively.
Cancer helpful reading:
- Cancer Moonshot
- Defense Health Agency
What is Cancer and How Does It Develop?
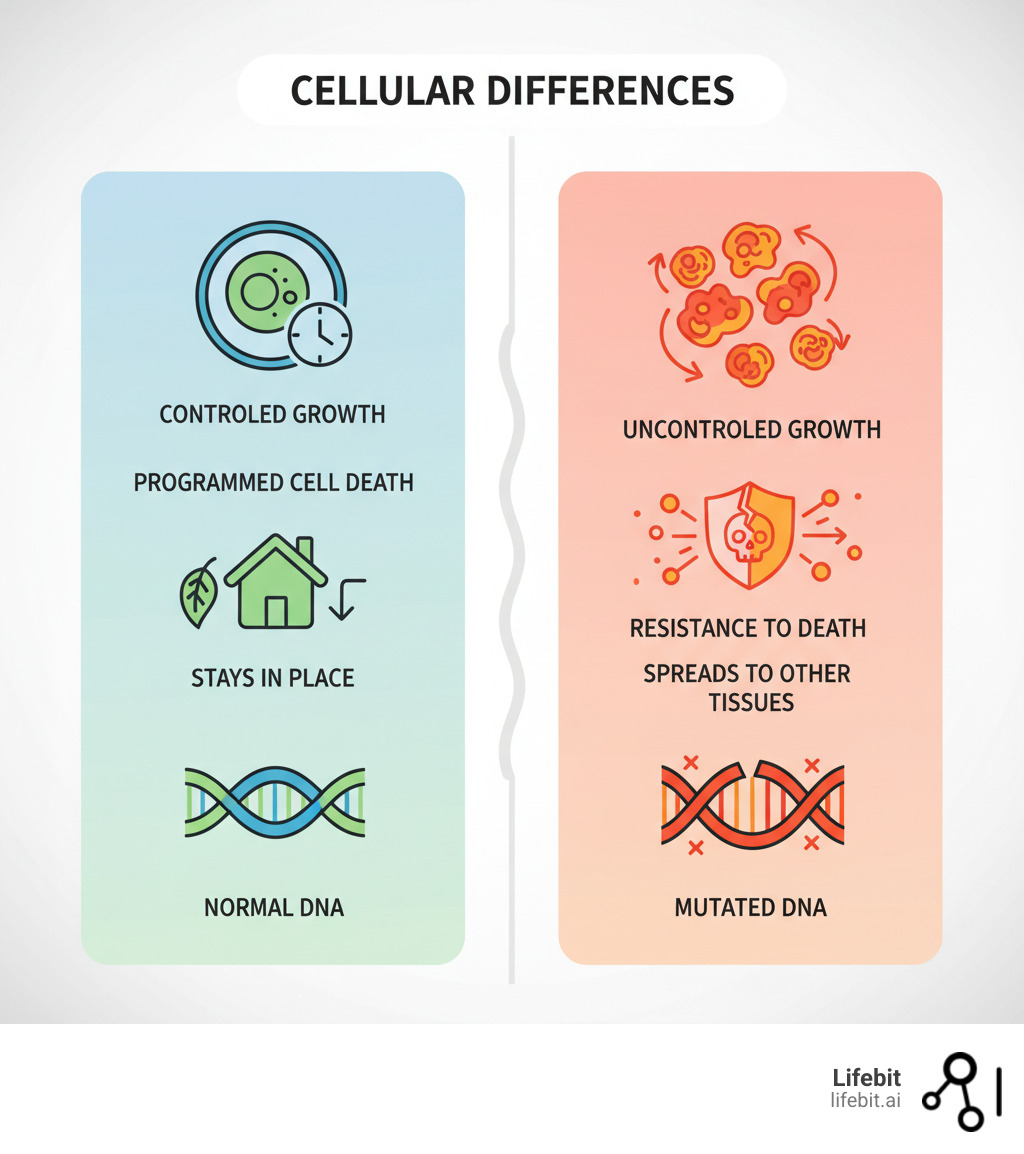
Your body contains trillions of cells that normally grow, divide, and die in a controlled process. Cancer begins when this process breaks down. Cells start growing uncontrollably, ignoring the body’s “stop” signals and creating chaos.
This cellular rebellion is caused by changes or damage—called mutations—to our DNA, the instruction manual in every cell. These mutations can affect key genes that control cell behavior:
- Oncogenes act like gas pedals for cell growth. Mutations can get them stuck in the “on” position.
- Tumor suppressor genes are the brakes. When damaged, they fail to stop abnormal cell division.
- DNA repair genes fix errors in our genetic code. When they’re faulty, mutations accumulate faster, increasing cancer risk.
As these mutated cells multiply, they can form a mass called a tumor. Not all tumors are cancerous. Benign tumors grow slowly and stay in one place. They don’t invade nearby tissues and can often be removed completely.
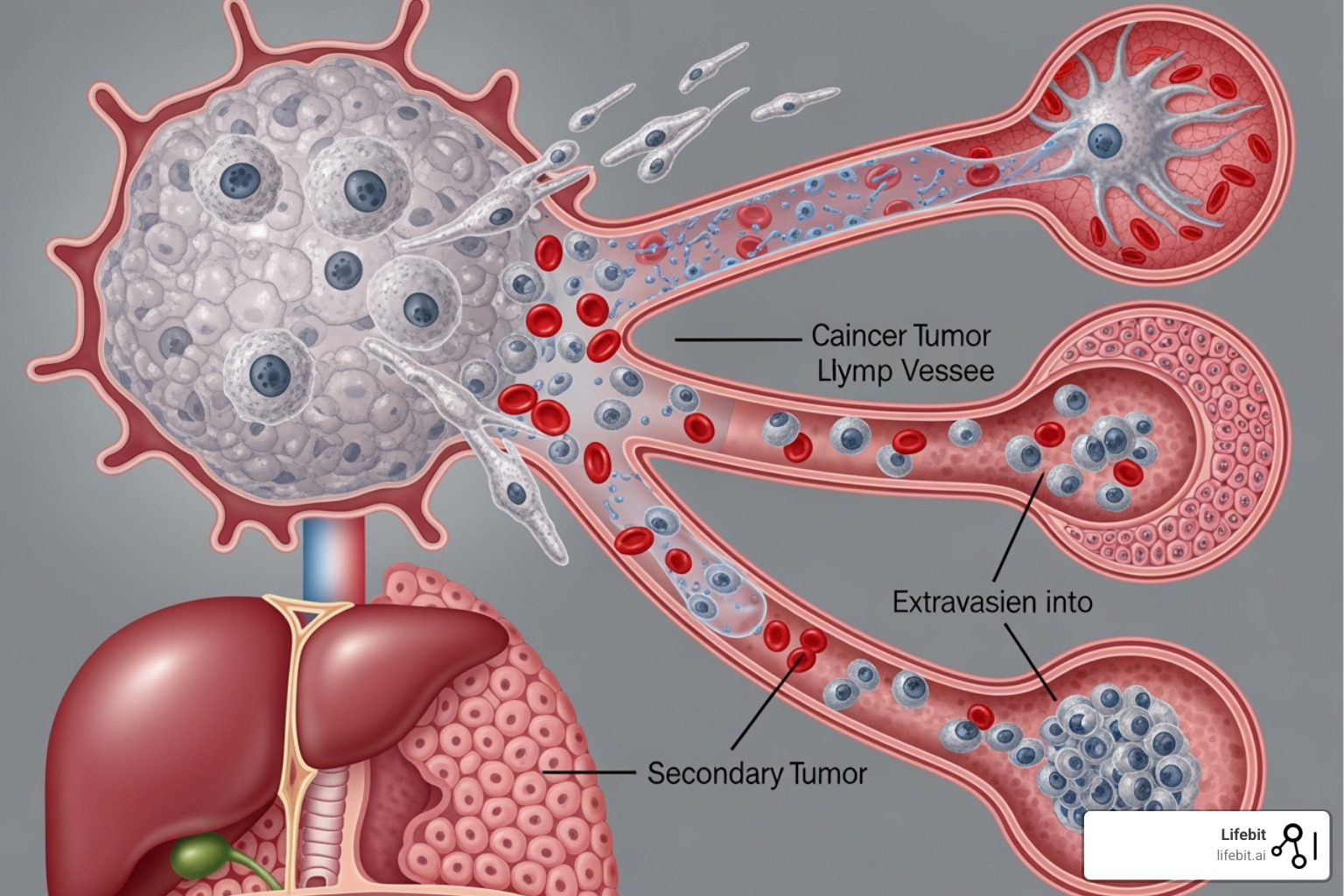
Malignant tumors, however, are cancerous. They are aggressive, invading surrounding healthy tissues. To fuel their rapid growth, they trick the body into growing new blood vessels to supply them with nutrients, a process called angiogenesis. The most dangerous trait of malignant tumors is metastasis: cancer cells break away, travel through the bloodstream or lymphatic system, and form new tumors in distant parts of the body. Most cancer deaths are due to this metastatic spread.
The Hallmarks of Cancer
All cancers share a set of fundamental abilities that transform normal cells into malignant ones. These are known as the “Hallmarks of Cancer.”
- Sustaining proliferative signaling: Constantly telling themselves to grow and divide.
- Evading growth suppressors: Ignoring the body’s natural “stop” signals.
- Resisting cell death: Bypassing the normal process of programmed cell death (apoptosis).
- Enabling replicative immortality: Dividing indefinitely, unlike normal cells which have a limited lifespan.
- Inducing angiogenesis: Stimulating the growth of new blood vessels to get nutrients.
- Activating invasion and metastasis: Gaining the ability to spread to other parts of the body.
- Genome instability and mutation: Accumulating more genetic errors, which fuels their evolution.
- Tumor-promoting inflammation: Using the body’s immune response to support their own growth.
Classifying Different Types of Cancer
Cancer is classified based on the type of cell it originates from. There are over 100 types, but most fall into several main categories:
- Carcinomas: The most common type (80-90% of cases), arising from epithelial cells that line organs and glands. Examples include breast, lung, colon, and prostate cancers.
- Sarcomas: Cancers of connective tissues like bone, muscle, and fat.
- Leukemias: Cancers of blood-forming tissues, like bone marrow, that lead to abnormal white blood cells.
- Lymphomas: Cancers that start in the immune system’s lymphocytes, typically in lymph nodes.
- Multiple Myeloma: Cancer of plasma cells, another immune cell in the bone marrow.
- Central Nervous System Cancers: Tumors that begin in the brain and spinal cord.
Globally, the four most common types are breast cancer, lung cancer, colorectal cancer, and prostate cancer.
Primary Causes and Risk Factors
Cancer is a genetic disease, caused by changes to the DNA inside our cells. These changes can be inherited, but the vast majority are acquired over a lifetime through a complex interplay of our behaviors, environment, and biology.
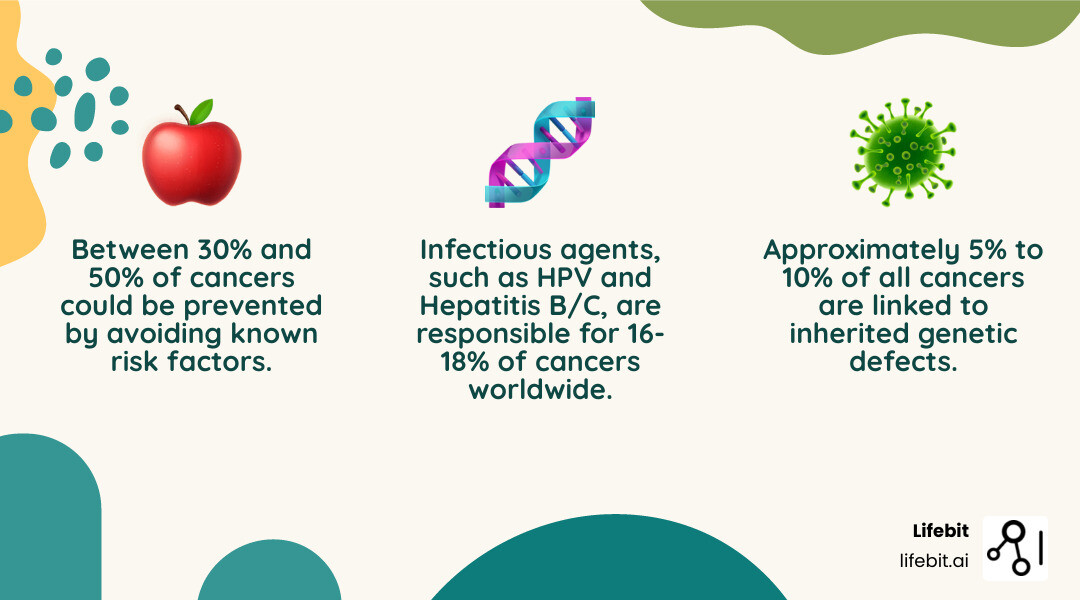
- Acquired (or somatic) mutations are responsible for 90-95% of cancers. They are not passed down to children and result from factors like lifestyle choices, exposure to carcinogens, and random errors during cell division.
- Inherited (or germline) mutations account for 5-10% of cancers. These are genetic defects present in every cell, passed down from a parent, which significantly increase an individual’s lifetime risk.
Age is the single biggest risk factor for cancer, as our cells have more time to accumulate genetic damage. However, this is not just a disease of the elderly. Research shows that 30-50% of cancers are preventable by avoiding known risk factors and adopting healthier habits. Scientific research on cancer prevention highlights our power to reduce risk through informed choices.
Lifestyle and Behavioral Risk Factors
Daily choices have a profound and cumulative impact on cancer risk.
- Tobacco use is the leading preventable cause of cancer death, responsible for about 30% of all cancer fatalities. It is linked to cancers of the lung, mouth, throat, esophagus, bladder, and many other organs. Exposure to secondhand smoke also significantly increases risk.
- Alcohol consumption is a known carcinogen. The body converts alcohol into acetaldehyde, a chemical that damages DNA. This increases the risk of mouth, throat, liver, colorectal, and breast cancers, with risk rising alongside consumption levels.
- A poor diet contributes significantly to cancer risk. Diets high in processed foods and red meat (classified as a Group 1 carcinogen by the IARC) are linked to higher rates of colorectal cancer. Conversely, a diet rich in fruits, vegetables, and fiber is protective, as these foods contain antioxidants that help protect cells from damage.
- Physical inactivity is an independent risk factor for colon, breast, and endometrial cancers. Regular activity helps maintain a healthy weight, regulates hormones like insulin, and supports healthy immune function.
- Obesity is a major risk factor for at least 13 types of cancer. Excess body fat is metabolically active, producing excess hormones and proteins that can fuel inflammation and cancer growth.
- Excessive sun and UV exposure from the sun or tanning beds is the primary cause of most skin cancers, including melanoma. UV radiation directly damages the DNA in skin cells, leading to cancer-causing mutations.
Environmental and Infectious Agents
Our surroundings and certain infections also play a critical role.
- Infectious agents cause about 16-18% of cancers worldwide. Key examples include Human Papillomavirus (HPV) (cervical/throat cancer), Hepatitis B and C (liver cancer), and the bacterium Helicobacter pylori (stomach cancer). The Epstein-Barr virus (EBV) is also linked to certain lymphomas.
- Radiation exposure, including ionizing radiation from natural sources like radon gas (a leading cause of lung cancer in non-smokers) and medical sources like CT scans, can damage DNA and increase risk over time.
- Chemical carcinogens are substances in the environment and workplace known to cause cancer. Well-known examples include asbestos (mesothelioma), benzene (leukemia), formaldehyde, and arsenic.
Genetic and Hereditary Risk Factors
While most cancers aren’t directly inherited, genetics can create a strong predisposition. About 5-10% of cancers are linked to inherited genetic defects.
- Family history is a key clue. A pattern of multiple relatives with cancer, cancers at unusually young ages, or an individual with multiple cancer types may suggest an inherited risk.
- BRCA1 and BRCA2 are well-known tumor suppressor genes. Inherited mutations in these genes dramatically increase the lifetime risk of breast, ovarian, prostate, and pancreatic cancers.
- Hereditary cancer syndromes, like Lynch syndrome, are specific genetic conditions that dramatically raise the risk for certain cancers, primarily colorectal, endometrial, and ovarian cancers.
Genomic technologies can now identify these high-risk mutations, allowing for personalized screening schedules and preventive strategies. A genetic predisposition does not mean cancer is inevitable; it provides crucial information for proactive health management.
Diagnosis, Staging, and Prognosis of Cancer
Early detection saves lives. Many cancers are curable when caught and treated promptly. It’s vital to pay attention to your body and follow recommended screening guidelines.
General warning signs can include persistent fatigue, unexplained weight loss, new lumps, skin changes, abnormal bleeding, or unexplained pain. If a symptom lasts for more than two weeks, consult a healthcare provider. While most symptoms have benign causes, it’s always best to check.
How Cancer is Diagnosed
A diagnosis typically involves several steps to get a clear picture of what’s happening.
- Physical exams: A doctor checks for lumps, skin changes, or other abnormalities.
- Laboratory tests: Blood and urine tests can detect tumor markers or other signs of disease.
- Imaging tests: CT scans, MRIs, PET scans, X-rays, and ultrasounds help visualize tumors and suspicious areas inside the body.
- Biopsy: This is the definitive step. A small tissue sample is removed and examined by a pathologist to confirm the presence of cancer, identify its type, and assess its aggressiveness.
- Genomic testing: Genetic tests on the biopsy sample identify specific mutations in the cancer cells, which helps guide personalized treatments.
Understanding Cancer Staging
After a diagnosis, doctors determine the cancer’s stage—a map of how large the tumor is and how far it has spread. Staging is crucial for planning treatment and understanding the prognosis.
The most common system is TNM staging:
- T (Tumor): Describes the primary tumor’s size and extent.
- N (Node): Indicates if the cancer has spread to nearby lymph nodes.
- M (Metastasis): Shows if the cancer has spread to distant parts of the body.
Based on the TNM values, an overall stage from 0 to IV is assigned:
- Stage 0: Abnormal cells are present but have not spread.
- Stages I-III: Cancer has grown into nearby tissue or spread to lymph nodes. Higher numbers indicate more extensive disease.
- Stage IV: Metastatic cancer, meaning it has spread to distant organs.
Doctors also consider the cancer grade, which describes how abnormal the cells look and how quickly they are likely to grow.
Determining the Prognosis for Individuals with Cancer
A prognosis is the likely course and outcome of the disease. It’s an estimate, as every person’s journey is unique. Key factors include:
- Cancer type and location: Some cancers are more aggressive or harder to treat than others.
- Stage at diagnosis: Early-stage cancers generally have much better outcomes. The average 5-year survival rate for all cancers in the U.S. is 66%, but this varies widely by type and stage.
- Age and overall health: Younger, healthier individuals may tolerate treatment better.
- Response to treatment: How well the cancer shrinks or disappears during therapy is a critical indicator.
Navigating Cancer Treatment and Prevention
Today’s cancer care is highly advanced and increasingly personalized. A multidisciplinary team of specialists—including surgical, medical, and radiation oncologists, pathologists, and specialized nurses—collaborates to create a treatment plan tailored to your specific cancer type, stage, and genetic profile.
An essential component of modern cancer care is palliative care. Contrary to a common misconception that it is only for end-of-life situations, palliative care is focused on improving quality of life by managing the symptoms and stresses of a serious illness. It can and should be integrated early in the cancer journey, alongside curative treatments, to help manage side effects like pain, nausea, and fatigue.
Main Treatment Options
Your treatment plan may involve one or more of the following approaches:
- Surgery: A primary treatment for solid tumors, surgery can be used for diagnosis (biopsy), complete removal of a localized tumor (curative surgery), or to relieve symptoms (palliative surgery). When cancer is caught early, surgery alone can often be curative.
- Chemotherapy: This systemic treatment uses drugs to kill rapidly dividing cells. Because cancer cells divide faster than most normal cells, they are more susceptible. However, other fast-growing cells (hair follicles, digestive tract) are also affected, leading to common side effects. It can be used before surgery (neoadjuvant), after surgery (adjuvant), or for metastatic cancer.
- Radiation Therapy: This treatment uses high-energy beams (e.g., X-rays) to damage the DNA of cancer cells in a specific area. Modern techniques precisely target the tumor while sparing surrounding healthy tissue, reducing side effects.
- Immunotherapy: A revolutionary approach that helps the body’s own immune system fight cancer. Checkpoint inhibitors, a common type, block signals that cancer cells use to hide from the immune system, effectively “releasing the brakes” and allowing immune cells to attack.
- Targeted Therapy: These drugs are designed to zero in on specific molecular abnormalities within cancer cells that drive their growth. A classic example is imatinib (Gleevec) for chronic myeloid leukemia (CML), which targets the specific protein causing the cancer.
- Hormone Therapy: Used for cancers fueled by hormones (like many breast and prostate cancers), this therapy works by blocking hormone production or interfering with their effects on cancer cells.
- Stem Cell Transplants: Primarily for blood cancers, this procedure replaces a patient’s diseased bone marrow with healthy blood-forming stem cells after high-dose chemotherapy or radiation.
Prevention: How to Reduce Your Cancer Risk
An estimated 30-50% of cancers are preventable. You can significantly lower your risk with these evidence-based strategies:
- Maintain a healthy diet and stay active: Eat plenty of fruits, vegetables, and whole grains. Limit red and processed meats. Aim for at least 150 minutes of moderate exercise per week.
- Avoid tobacco and limit alcohol: Quitting smoking is the single most important step. If you drink, do so in moderation.
- Protect your skin: Use broad-spectrum sunscreen, wear protective clothing, and avoid peak sun hours.
- Get vaccinated: The HPV vaccine prevents cancers caused by the human papillomavirus, and the Hepatitis B vaccine prevents a major cause of liver cancer.
- Follow screening guidelines: Regular mammograms, colonoscopies, and Pap tests can detect cancer early when it’s most treatable.
Support Systems for Patients and Families
Cancer affects entire families. Comprehensive care includes emotional, psychological, and practical support.
- Counseling and support groups provide a safe space to share experiences and learn coping strategies.
- Patient navigators and social workers are professionals who help guide patients through the complex healthcare system, assisting with appointments, insurance, and financial aid.
- Involving family and caregivers in the process creates a stronger support system. Many cancer centers offer resources specifically for caregivers.
- Community events like Relay For Life offer connection and a sense of purpose. You can Join a community support event.
You are not alone in this journey. With advanced treatments and strong support systems, there is genuine reason for hope.
The Future of Cancer Research and Cures
We are in an extraordinary era for cancer research, with the pace of findy accelerating rapidly. Precision medicine is moving from a concept to a reality, shifting treatment from one-size-fits-all approaches to therapies custom to each person’s unique cancer.
Big data and artificial intelligence (AI) are revolutionizing the field by processing vast amounts of genetic, clinical, and imaging data to find patterns that lead to faster drug findy and more accurate diagnoses. At the same time, innovative clinical trial designs are getting promising treatments to patients faster than ever before.

Innovations in Treatment and Technology
- Genomic sequencing allows us to map a cancer cell’s genetic blueprint, revealing its specific weaknesses for targeted treatment.
- Liquid biopsies detect tumor DNA in the bloodstream, enabling earlier detection, treatment monitoring, and tracking of resistance without invasive surgery.
- CAR T-cell therapy reprograms a patient’s own immune cells to recognize and attack cancer. It has produced remarkable remissions in some blood cancers.
- Cancer vaccines are being developed as treatments to train the immune system to destroy existing cancer cells.
- AI in cancer research is changing drug findy, improving radiological diagnoses, and predicting treatment responses. Read more about AI in cancer research.
- Federated learning for secure data analysis is a key technology that allows AI models to learn from data across multiple institutions without sensitive patient data ever leaving its source. This enables large-scale, collaborative research while protecting privacy.
The Role of Global Collaboration in Finding Cures
The fight against cancer is a global effort. International research initiatives and data-sharing platforms are breaking down silos, allowing scientists to analyze diverse datasets from around the world. This is crucial, as cancer affects populations differently based on genetics and environment.
Public health policies, guided by research, translate findies into real-world impact through vaccination programs and regulations that reduce exposure to carcinogens. The World Health Organization (WHO) aims to make cancer prevention and treatment accessible to everyone. This global perspective drives innovation and ensures that breakthroughs benefit patients everywhere.
Frequently Asked Questions about Cancer
When people learn about cancer, many questions arise. Here are clear, honest answers to the most common ones.
Can cancer be cured completely?
Yes, many cancers can be cured, especially when detected early. Doctors often use the term “remission,” where all signs of cancer have disappeared. If a person remains in complete remission for five years or more, they are often considered cured.
Early detection is key. For example, early-stage breast, colorectal, and many skin cancers have very high cure rates. Some cancers, like testicular cancer, have cure rates above 90% even when advanced.
For more advanced cancers, treatment may focus on long-term management, controlling the disease and allowing people to live well for many years. The average five-year survival rate for all cancers in the U.S. is now 66%, a testament to decades of progress.
Is cancer contagious?
No, cancer is not contagious. You cannot catch it from another person through casual contact, sharing meals, or kissing. Cancer arises from changes within a person’s own cells.
The confusion often comes from the fact that some viruses and bacteria that increase cancer risk are contagious. For example, Human Papillomavirus (HPV), which can lead to cervical cancer, is spread through sexual contact. Hepatitis B and C, which can cause liver cancer, are also transmissible. However, it is the infectious agent that is contagious, not the cancer itself. Most people with these infections will not develop cancer, and vaccines are available to prevent HPV and Hepatitis B.
What is the difference between benign and malignant tumors?
This distinction is critical for treatment and prognosis.
Benign tumors are non-cancerous.
- They grow slowly and are contained within a clear boundary.
- They do not invade nearby tissues or spread to other parts of the body (metastasize).
- Their cells look relatively normal.
- They are usually removed with surgery and rarely return.
Malignant tumors are cancerous.
- They grow rapidly and aggressively, invading surrounding healthy tissue.
- They can metastasize, meaning cells break away and form new tumors in distant organs.
- Their cells look abnormal and disorganized.
- They require comprehensive treatment like surgery, chemotherapy, or immunotherapy to destroy cancer cells throughout the body.
A pathologist can easily distinguish between benign and malignant cells by examining a biopsy sample, which is why a biopsy is essential for a definitive diagnosis.
Conclusion
Cancer is a complex challenge, but the story of our fight against it is one of inspiring scientific progress and hope. We have learned to combat this disease with precision, compassion, and a deep commitment to understanding its every detail.
The progress is undeniable. The average five-year survival rate of 66% in the United States reflects millions of individual victories, thanks to treatments that didn’t exist a decade ago. We are moving beyond one-size-fits-all approaches and designing personalized therapies that target the unique genetic fingerprint of each tumor.
Technologies like genomic sequencing, liquid biopsies, and artificial intelligence are accelerating this progress. At Lifebit, we see how federated learning enables secure global collaboration, open uping insights from diverse datasets while keeping patient data safe. This collaborative approach is essential for finding solutions that benefit everyone.
Prevention also remains one of our most powerful tools. Knowing that up to half of all cancers are preventable through lifestyle choices—like maintaining a healthy weight, avoiding tobacco, and getting regular screenings—is incredibly empowering.
The future of cancer research is bright. The combination of advanced genomics, AI-driven insights, and global collaboration is creating a world where cancer can become a manageable condition rather than a feared diagnosis. Together, we are not just fighting cancer—we are winning.
To learn more about how our federated AI platform is empowering secure, real-time insights for cancer research and beyond, please visit Lifebit’s federated AI platform.

