Healthcare’s AI Advantage: Choosing the Best Platform

Why Healthcare Leaders Are Betting Big on AI Platforms
AI platform healthcare solutions are no longer optional—they’re essential infrastructure. Healthcare systems implementing these platforms report 3-5x return on investment, with 93% of health leaders calling AI critical to their facility strategy. But what exactly are these platforms, and how do you choose the right one?
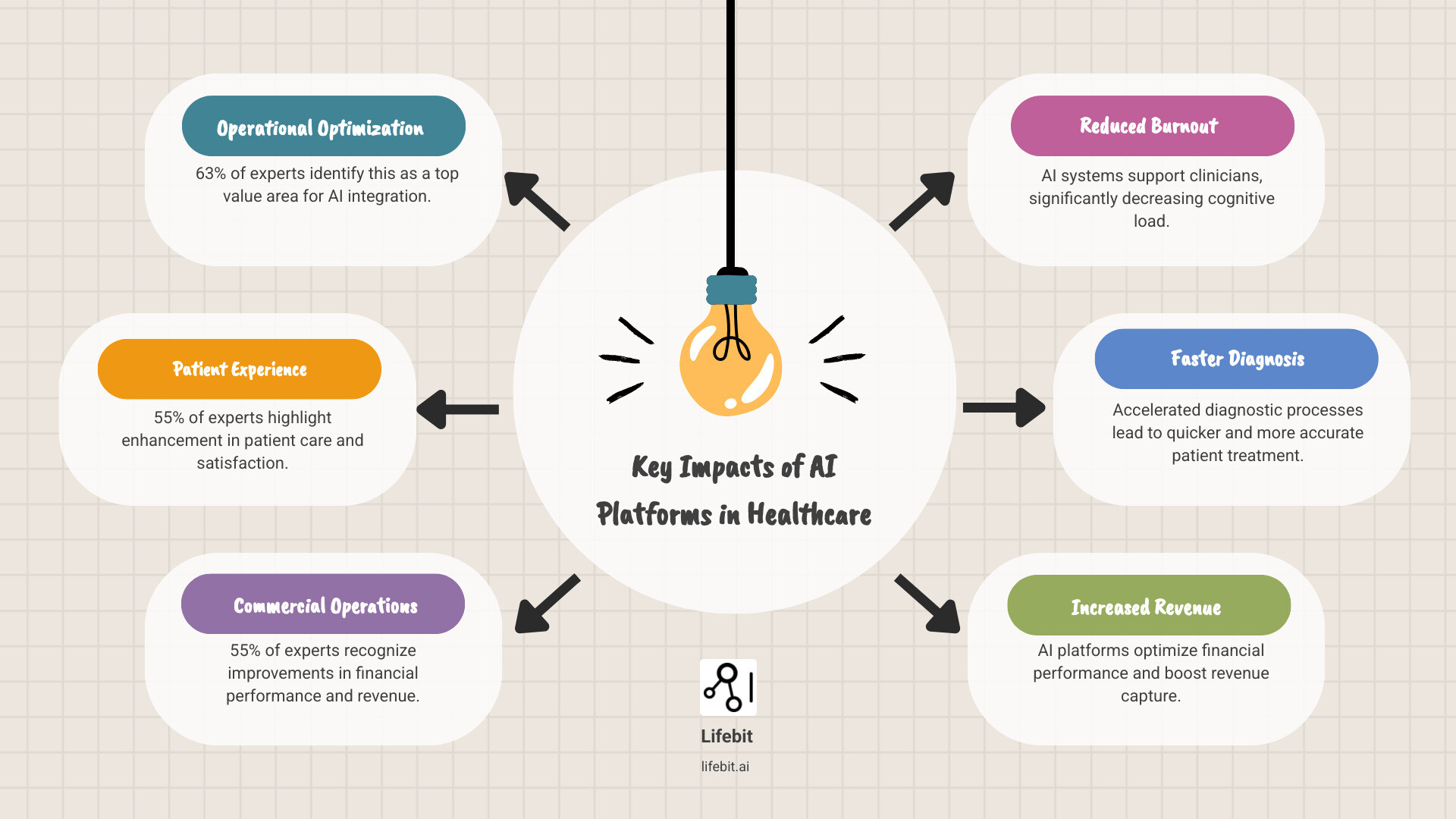
Here’s what an AI platform for healthcare actually delivers:
| Core Function | Real-World Impact |
|---|---|
| Clinical Support | 50+ FDA-cleared algorithms for diagnosis and decision support |
| Operational Efficiency | 32% reduction in no-shows, 5,000+ staff hours reallocated monthly |
| Clinician Wellness | 78% decrease in cognitive load, 86% less after-hours work |
| Financial Performance | $93,360+ increased revenue capture within 3 months |
| Patient Experience | 99% satisfaction rates, 90%+ reduction in check-in time |
The stakes are high. Clinician burnout is accelerating, administrative costs are crushing margins, and patients expect seamless care. AI platforms promise to address all three—but only if you choose wisely.
The market is crowded with specialized tools and enterprise platforms. Some vendors prioritize speed, others clinical validation. A few are pioneering federated approaches that let you analyze data without moving it—a game-changer for privacy and compliance.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. With over 15 years in computational biology, AI, and health-tech, I’ve seen what works—and what doesn’t—when deploying AI at scale in healthcare.
Core Capabilities: What a Healthcare AI Platform Actually Does
An ai platform healthcare solution acts as the central nervous system for a modern medical facility, uniting scattered data into actionable insights. It functions as an intelligent layer that sits across an organization’s entire data ecosystem, enabling advanced analytics and automation that would be impossible with siloed systems.
This works through several key technologies. Data aggregation is the foundational step, pulling together information from disparate sources like electronic health records (EHRs), laboratory information systems (LIS), medical images (PACS), and even real-world evidence from wearables and patient-reported outcomes. Machine learning then learns from this aggregated data to spot complex patterns, predict outcomes, and automate repetitive tasks. Natural Language Processing (NLP) is the component that allows the AI to read and understand unstructured human language. It extracts structured data from unstructured text, such as a physician’s narrative notes, pathology reports, and patient correspondence. This allows systems to identify patient cohorts based on specific phenotypes, track disease progression from narrative descriptions, and flag potential adverse events mentioned in passing. Meanwhile, computer vision gives the AI the ability to analyze medical imaging with superhuman speed and consistency. For example, in radiology, it can highlight suspicious nodules on a chest CT scan that might indicate early-stage lung cancer. In pathology, it can count mitotic figures in digital slides to help grade tumors. This doesn’t replace the radiologist or pathologist but acts as a tireless second reader, flagging areas of interest and reducing the risk of perceptual errors.
Predictive analytics uses these learned patterns to forecast future events, such as which patients are at high risk for readmission, sepsis, or equipment failure. Finally, seamless EHR integration ensures these AI capabilities appear directly within the clinician’s existing workflow, which is absolutely critical for adoption and real-world impact.

From Data to Diagnosis: Clinical Applications
AI platforms excel at helping clinicians make better, faster, and more data-driven decisions.
Clinical decision support (CDS) systems analyze a patient’s complete data profile in real-time against a vast library of medical literature, clinical guidelines, and historical data. This provides real-time recommendations, such as flagging a potential drug-gene interaction, suggesting a differential diagnosis, or recommending a specific diagnostic pathway. It serves as an intelligent co-pilot, augmenting clinical judgment rather than replacing it.
Diagnostic imaging analysis uses computer vision to scan medical images with incredible speed and accuracy. Platforms can leverage over 50 FDA-approved algorithms to auto-detect suspected diseases. These algorithms cover a vast range of specialties. For instance, in neurology, AI can detect early signs of stroke or brain bleeds on non-contrast CT scans, triggering immediate alerts for the stroke team. In cardiology, it can automatically calculate ejection fractions from echocardiograms, a key indicator of heart function. In oncology, it helps delineate tumor boundaries for radiation therapy planning.
AI scribes and ambient documentation are life-changing for burnt-out clinicians. This technology, often called ‘ambient clinical intelligence,’ uses microphones in the exam room to capture the natural conversation between a doctor and patient. The AI then parses this conversation, identifies the relevant clinical information, and structures it into a standard SOAP note format directly within the EHR. This results in a 78% decrease in cognitive load, saves hours of documentation time, and allows 90% more undivided attention for patients, improving the quality of the human interaction during the visit.
Personalized medicine moves beyond one-size-fits-all care by analyzing a patient’s unique genomic data, lifestyle, and medical history to tailor treatment plans. AI platforms can identify which patients are most likely to respond to a particular therapy, minimizing trial-and-error and improving outcomes.
Streamlining the System: Operational Automation
While diagnostics get the headlines, operational AI delivers serious and immediate financial relief.
Administrative automation handles high-volume, repetitive tasks like patient intake, insurance eligibility verification, and referral management. By digitizing and automating these processes, one system achieved a 90%+ reduction in check-in time and effectively automated the work of 80 open roles, allowing staff to be redeployed to more complex, patient-facing responsibilities.
Revenue Cycle Management (RCM) AI optimizes the complex process of coding, billing, and claims submission. AI-powered RCM tools analyze clinical documentation to suggest the most accurate medical codes (ICD-10, CPT), reducing the risk of under-coding (lost revenue) or over-coding (compliance risk). They can also automate the prior authorization process by pre-filling forms and tracking submissions with payers, achieving a 91% successful authorization rate and capturing an additional $93,360 in revenue within three months.
Patient scheduling and no-show reduction uses predictive AI to manage complex schedules and identify which patients are most likely to miss their appointments. The system can then trigger automated, personalized reminders or allow for proactive rescheduling. This has led to a 32% reduction in no-shows and 14,500 avoided missed appointments in some cases, optimizing clinic utilization and revenue.
This frees up significant resources, with some organizations reallocating over 5,000 staff hours per month to more meaningful, patient-facing work.
Accelerating Discovery: Research and Development
The long-term promise of ai platform healthcare is accelerating biomedical research, where federated platforms—like Lifebit’s—are game-changers.
Drug discovery benefits as AI analyzes molecular structures and biological pathways to predict drug efficacy and toxicity exponentially faster than traditional methods. Clinical trial optimization uses AI to design more efficient trials, identify eligible patient cohorts from real-world data, and analyze trial results more effectively.
Multi-omic data analysis is a key frontier, integrating vast and disparate datasets—genomics (DNA), transcriptomics (RNA), proteomics (proteins), metabolomics (metabolites), alongside clinical data from the EHR. An AI platform can identify complex molecular signatures that correlate with disease subtypes or treatment response, paving the way for true precision medicine. For example, it might find that patients with a specific genetic marker and certain protein expression levels respond exceptionally well to a new therapy, a discovery impossible to make by looking at any single data type in isolation. Real-world evidence (RWE) generation taps into de-identified EHRs and wearables to understand how treatments perform in diverse, everyday populations outside the controlled environment of a clinical trial.
Our federated approach supports the Pan-Canadian AI for Health (AI4H) Guiding Principles by enabling secure, cross-institutional collaboration without moving sensitive data.
The Transformative Impact: Benefits for Clinicians, Administrators, and Patients
Adopting an AI platform healthcare solution reshapes how healthcare works for everyone. The benefits cascade through the entire organization, with systems consistently reporting 3-5x return on investment.
But what does this mean for the people on the front lines?

For Clinicians: Reducing Burnout and Enhancing Care
Clinician burnout is a crisis driven by administrative overload. AI platforms make a profound human impact by automating documentation and surfacing relevant information instantly, leading to a 78% decrease in cognitive load.
This is transformative. Imagine finishing your shift on time. 86% of clinicians using AI platforms report less after-hours work, meaning more time for family and rest. By handling the busywork, AI frees clinicians to focus on patients, dedicating 90% more undivided attention to them.
The result is a 53% improvement in professional fulfillment as clinicians can practice at the top of their license instead of wrestling with data entry.
For Administrators: Driving Efficiency and ROI
Administrators must balance costs, quality, staffing, and revenue. AI platforms provide leverage across all these areas. Automation and predictive analytics create substantial cost savings, but the revenue impact is often even more surprising.
Streamlined revenue cycle management achieves a 91% successful prior authorization rate, while a 32% reduction in no-shows means more completed appointments. The combined effect is $93,360+ in increased revenue capture within just three months.
Workforce optimization is another strategic benefit. One system automated 80 open roles, while another reallocated over 5,000 staff hours per month to higher-value work. This isn’t about replacing people; it’s about releasing their potential. Robust analytics also enable data-driven strategic decisions, which is why 93% of health leaders see AI as essential.
For Patients: Improving Experiences and Outcomes
Patients care about results: feeling heard, getting a fast diagnosis, and receiving effective treatment. AI delivers on all three.
Personalized care becomes possible at scale, and faster diagnosis leads to earlier intervention and better outcomes. The patient experience also improves in tangible ways, with a 90%+ reduction in check-in time.
The proof is in the numbers: organizations report 99% patient and caregiver satisfaction with intake and 95% satisfaction with scheduling. These are exceptional scores for healthcare.
AI platform healthcare solutions succeed because they make healthcare work better for everyone. Clinicians refind their purpose, administrators achieve financial sustainability, and patients receive the personalized, efficient care they deserve.
Your Strategic Checklist for Choosing an ai platform healthcare
Choosing the right AI platform healthcare solution is a consequential decision with long-term implications. The right choice unlocks transformative benefits across clinical, operational, and financial domains; the wrong one leads to integration nightmares, poor adoption, and wasted investment.
Based on our experience implementing AI platforms for leading healthcare and research organizations worldwide, we’ve learned what separates platforms that deliver from those that disappoint. Here’s your strategic checklist for evaluating potential solutions.
Integration and Scalability: Will It Fit Your Ecosystem?
Sophisticated AI is worthless if it’s not seamlessly integrated into the clinical workflow. Poor integration is the number one killer of AI adoption in healthcare.
EHR integration is your first checkpoint. Does the platform offer robust, bi-directional integration with your specific EHR (e.g., Epic, Cerner)? Can it pull data and, crucially, push insights, alerts, and structured data back where clinicians work? Look for platforms using modern standards like HL7/FHIR for true interoperability, not just clunky, one-off connections.
Your IT infrastructure strategy also matters. Platforms can be cloud-native, on-premise, or hybrid. The right choice depends on your data governance policies, existing infrastructure, and long-term strategy. Cloud solutions offer faster deployment and scalability, while on-premise or hybrid models may better serve organizations with strict data residency requirements or large existing data centers.
Scalability is where many platforms stumble. A solution must be architected to support enterprise-wide data volumes and user loads without performance degradation. API availability is also critical, as it provides future-proofing, allowing your internal teams to build custom integrations and extend the platform’s functionality as your needs evolve.
Beyond technical integration, consider organizational integration and change management. A new platform changes how people work. The vendor should have a clear methodology for user training, workflow redesign, and stakeholder communication. Ask potential partners how they support clinical champions, manage resistance to change, and measure user adoption and satisfaction post-launch. A technically perfect platform will fail if clinicians see it as a burden rather than a benefit.
Security, Privacy, and Compliance: Is Your Data Safe?
In healthcare, a data breach is a catastrophic event that destroys patient trust and incurs massive regulatory fines. The platform you choose must be built on an uncompromising foundation of security and compliance.
HIPAA compliance is table stakes in the U.S. For organizations in Europe and the UK, GDPR compliance is equally critical. Beyond these, consider other regional regulations like the California Consumer Privacy Act (CCPA) or Canada’s PIPEDA. Demand evidence of a vendor’s compliance framework, including third-party audits and certifications like ISO 27001 or SOC 2 Type II attestations, which provide independent validation of their security controls.
Data encryption—both in transit (using protocols like TLS 1.2+) and at rest (using standards like AES-256)—is non-negotiable. But security is more than just encryption. You need defense-in-depth, including granular role-based access control (RBAC), comprehensive audit logging, and regular vulnerability assessments. A mature vendor will be able to discuss their approach to data minimization, ensuring users only see the minimum data necessary to perform their jobs.
This is where federated governance is transformative. Traditional platforms require centralizing massive amounts of sensitive data, creating a high-value target for attackers and significant privacy risks. A federated approach, like ours, analyzes data in its original secure environment. This enables powerful AI while keeping data behind your firewall, a principle recognized in the European Commission’s guidance on Artificial Intelligence in healthcare.
Trusted Research Environments (TREs), also known as Secure Data Environments, provide secure, audited spaces for researchers to analyze sensitive data without direct exposure. The platform provides the analytical tools within the secure ‘walls’ of the TRE, and only aggregated, non-identifiable results can be exported, subject to an audit. This model is becoming the gold standard for academic and public-private research collaborations. Data sovereignty is also a dealbreaker for many governments and health systems, who require health data to remain within their borders. Federated platforms uniquely address this by enabling global collaboration while keeping data local.
Clinical Validation and Model Governance: Does the AI Actually Work?
The efficacy of an ai platform healthcare solution hinges on the quality of its algorithms. It’s not enough for a vendor to claim their AI is ‘accurate.’ You must demand evidence and a commitment to responsible AI practices.
- Clinical Validation: Has the algorithm been validated in peer-reviewed publications? Was it tested on a patient population that reflects your own in terms of demographics, comorbidities, and disease prevalence? An algorithm validated in one setting may not perform as well in another.
- Regulatory Clearance: For diagnostic tools, is the algorithm FDA-cleared, CE-marked, or approved by other relevant regulatory bodies? This is a baseline requirement for clinical use, indicating a level of safety and efficacy review.
- Model Governance and Bias Monitoring: AI models are not static. Their performance can degrade over time as clinical practices, patient populations, or data inputs change—a phenomenon known as ‘model drift.’ Furthermore, models trained on biased data can perpetuate and even amplify health disparities. Ask vendors about their process for ongoing model monitoring. How do they detect performance degradation? How do they test for and mitigate algorithmic bias across different racial, ethnic, and gender groups? A responsible partner will have a robust framework for AI governance and ethics.
Evaluating the Partnership: Vendor and Pricing
The vendor relationship is a long-term partnership, as important as the technology itself.
Pricing models vary widely, from pay-as-you-go (we offer $50 in free credits for testing) to tiered subscriptions and custom enterprise agreements. Beware of low initial costs that hide expensive add-ons for data storage, API calls, or premium support. Calculate the total cost of ownership (TCO), including integration fees, maintenance, training, and ongoing support.
Implementation support is critical for success. Does the vendor provide a dedicated implementation team and clinical workflow specialists? Ask for case studies and references from organizations similar to yours and inquire about their typical implementation timeline and process.
Training and support determine whether your investment delivers value. Look for vendors who offer comprehensive, role-specific training programs to ensure your staff can leverage the platform effectively. Evaluate their post-launch support model: What are their service-level agreements (SLAs)? Do they offer a dedicated customer success manager?
The vendor’s vision and roadmap are also key. Are they investing in emerging capabilities like federated learning, multi-modal AI, and generative AI? You’re not just buying a product; you’re betting on their ability to innovate and evolve with the market.
The Future is Federated: Emerging Trends in Healthcare AI
Healthcare AI is evolving at a breathtaking pace, with key trends reshaping how we think about AI platform healthcare solutions in terms of scale, security, and collaboration. Staying ahead of these trends is crucial for making a future-proof investment.
Generative AI is moving beyond analysis to creation. It is now being used to create new outputs, like clinical summaries from patient-doctor conversations, or even high-fidelity synthetic patient data. This synthetic data, which mimics the statistical properties of real patient data, is invaluable for training and validating AI models without exposing sensitive patient information, or for augmenting datasets for rare diseases where real-world data is scarce.
Federated learning is the paradigm shift we’re deeply invested in. Instead of centralizing data—a privacy nightmare and logistical headache—it trains AI models where the data lives. The data never moves; only the insights and model parameters do. This is a game-changer for security, data sovereignty, and global collaboration.
AI-driven safety surveillance is another frontier, enabling proactive pharmacovigilance. Instead of relying on passive reporting, these systems can continuously monitor real-world data from EHRs and claims databases to detect potential adverse drug events or device malfunctions much earlier than traditional methods.
Real-time analytics is also becoming standard. The ability to analyze streaming data from patient monitors or EHRs to predict events like the onset of sepsis is critical. Our R.E.A.L. (Real-time Evidence & Analytics Layer) is designed for this, delivering immediate, actionable insights at the point of care.
Underpinning this is the Trusted Data Lakehouse (TDL), a modern hybrid architecture combining a data lake’s flexibility for unstructured data with a data warehouse’s robust governance and performance. Our TDL provides a secure, scalable foundation for analyzing the diverse, multi-modal data that defines modern healthcare.

Why a federated ai platform healthcare is the future
The federated model rethinks data handling to balance the urgent need for innovation with the non-negotiable requirement for ironclad privacy and security.
Secure data access is the primary benefit. By keeping sensitive patient data at its source—inside hospital firewalls or within national data enclaves—federated platforms dramatically reduce the attack surface and the risk of a catastrophic breach. The data stays home. The intelligence travels.
Global collaboration becomes not just feasible, but practical. Consider a researcher studying a rare pediatric cancer. No single hospital has enough patients for a statistically significant study. Traditionally, this would require a years-long effort to create complex data-sharing agreements and physically centralize sensitive data from multiple institutions, a process fraught with legal and privacy hurdles. With a federated network, researchers can push a query or a model to be trained locally at each hospital. Only the anonymized, aggregated results or model updates are returned to the central researcher. This allows for powerful, multi-institutional studies to be conducted in weeks, not years, dramatically accelerating the pace of discovery for rare diseases.
Federated approaches help break down healthcare’s notorious data silos. They facilitate the integration of diverse datasets—EHRs, genomics, imaging—without forcing everything into one giant, monolithic database. A federated architecture can query and analyze these datasets in place, connecting insights across silos without the need for a massive, risky data migration project.
This approach excels at multi-omic data integration. It can combine genomics, proteomics, and clinical records to drive breakthroughs in personalized medicine by building a holistic view of the patient that is essential for developing targeted therapies.
Finally, federated learning leads to improved model accuracy and fairness. Training AI on diverse, real-world data from multiple sources and patient populations produces more robust and generalizable models. This helps ensure that AI innovations are effective for everyone and reduces the risk of building biased algorithms that only work for a narrow subset of the population.
Frequently Asked Questions about AI Platforms in Healthcare
Healthcare leaders consistently ask about the practical challenges of implementing AI platform healthcare solutions. Here are the answers.
What is the typical ROI of an AI platform in healthcare?
Well-implemented AI solutions typically deliver a 3-5x return on investment. This ROI comes from several areas:
- Cost savings from administrative automation and optimized resource allocation.
- Increased revenue from improved billing accuracy and reduced no-shows. Systems have captured an additional $93,360 in revenue within three months and cut no-shows by 32%.
- Operational efficiency through faster diagnoses and streamlined workflows, leading to higher patient throughput.
- Reduced staff turnover, a key but harder-to-quantify benefit, by alleviating clinician burnout (professional fulfillment improved by 53%).
How do AI platforms integrate with existing EHR systems?
Integration with existing EHRs is a valid concern. Modern platforms use several proven methods:
- APIs (Application Programming Interfaces) create communication channels for smooth data flow.
- HL7/FHIR standards are industry protocols that ensure different healthcare systems can communicate reliably.
- Native integration with popular EHRs is often available through vendor partnerships.
Most importantly, workflow embedding is crucial for clinician adoption. The best platforms deliver insights directly within the EHR interface, eliminating the need to switch between systems.
What are the biggest challenges when implementing healthcare AI?
Understanding the biggest implementation challenges helps you plan for success.
- Data quality: Healthcare data is often messy and incomplete. Significant data preparation is usually required before AI can be effective.
- Integration complexity: Connecting modern AI with legacy IT and diverse EHR systems can be technically challenging.
- Staff buy-in: Clinicians need training and clear communication to trust and adopt new AI tools. Overcoming resistance to change is essential.
- Regulatory problems: Navigating HIPAA, GDPR, and other data privacy laws requires robust governance. Federated approaches can minimize this friction.
- Initial investment cost: The upfront cost can be substantial. Organizations must consider the total cost of ownership, not just the purchase price.
These challenges are solvable with thoughtful planning, the right partner, and realistic timelines.
Conclusion: Your Next Step Towards an AI-Powered Future
The evidence is clear: AI platform healthcare solutions are reshaping healthcare delivery, operations, and research. The results are remarkable—clinicians spend 86% less time on after-hours work, organizations capture $93,360+ in new revenue in months, and patients report 99% satisfaction rates. These figures represent thriving organizations and better care.
Choosing the right platform is critical. The market is crowded, and solutions vary widely. Some focus on clinical tasks, others on operations. A select few, like Lifebit, pioneer the federated approach, enabling global data collaboration while keeping sensitive information secure and under your control.
Federated models are the present for organizations serious about data sovereignty, compliance, and research acceleration. Analyzing data across sites without moving it opens up previously impossible research in drug discovery and real-world evidence.
At Lifebit, we’ve spent over 15 years building a next-generation federated AI platform for biopharma, governments, and public health. Our Trusted Research Environment (TRE), Trusted Data Lakehouse (TDL), and R.E.A.L. layer deliver the security, speed, and insights modern healthcare demands—all while keeping your data secure.
Your next step is clear. The question isn’t whether to adopt AI—93% of health leaders have already answered that. The question is which partner will help you do it right.
Ready to see how a federated approach can change your healthcare operations and research? Explore a federated trusted research environment with us. Let’s build the future of healthcare together.

