The Amazing AI-Powered Clinical Trial Examples You Need to See Today

Stop Missing Trial Deadlines: AI Cuts Timelines 30–50% and Costs 40%
AI-Powered Clinical Trials: Real-World Examples Changing Research in 2025 are delivering measurable results that are changing how drugs reach patients. Here’s what’s happening:
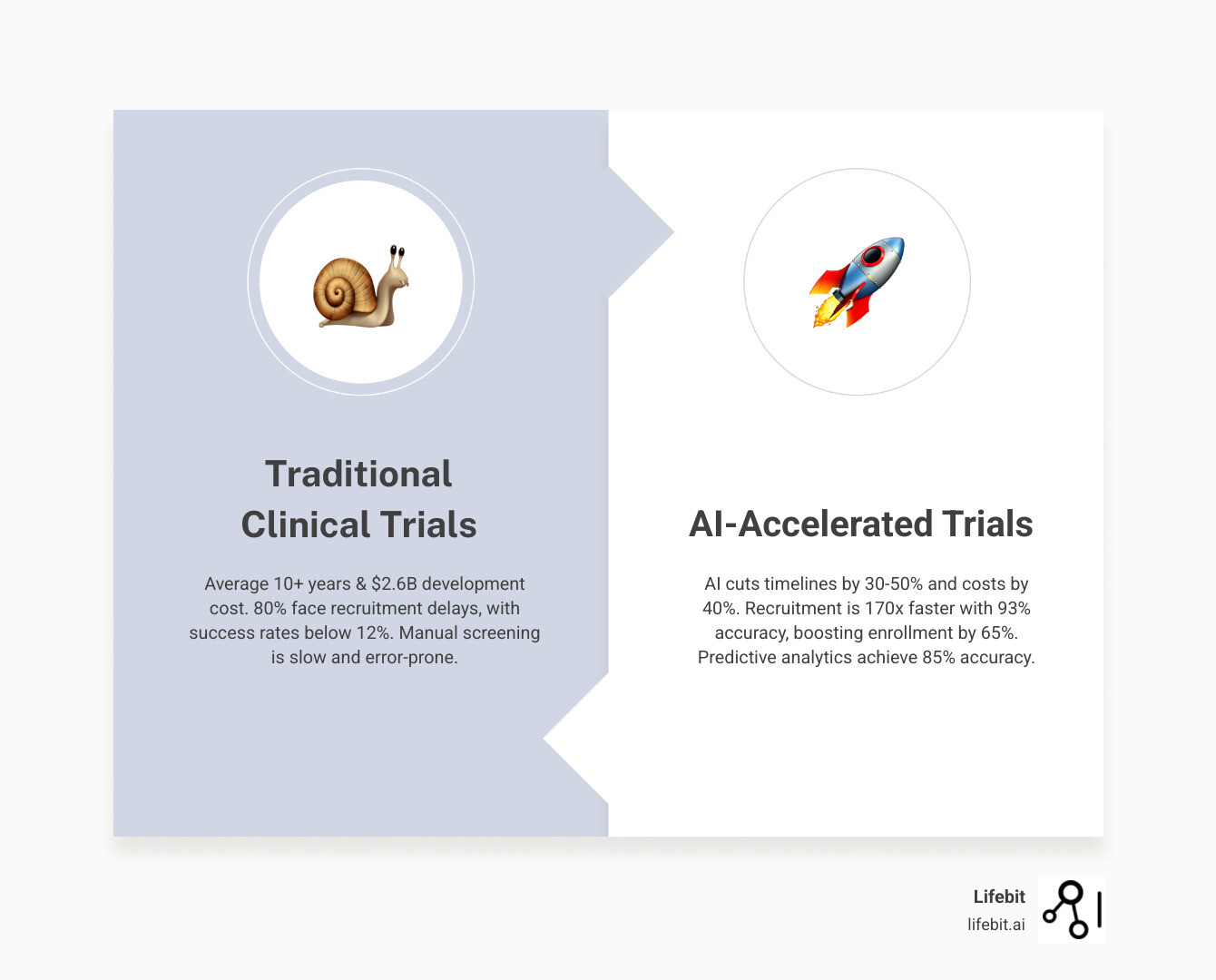
- Patient recruitment accelerated by 170x at Cleveland Clinic using AI to scan health records
- Eligibility screening with 93% accuracy using AI tools that read unstructured doctor’s notes
- Trial timelines reduced by 30-50% through predictive analytics and virtual control arms
- Costs cut by up to 40% by automating data management and protocol optimization
- 90% sensitivity for adverse events using digital biomarkers and continuous monitoring
- 65% improvement in enrollment rates with AI-powered patient matching platforms
Right now, 80% of clinical trials miss enrollment deadlines. Manual screening of health records takes hours per patient, protocol design relies on guesswork, and data is trapped in disconnected systems. This makes finding eligible patients or learning from past trials nearly impossible.
AI is solving these problems today. Natural language processing reads doctor’s notes to find candidates in minutes, not weeks. Predictive analytics simulate trial outcomes to prevent costly failures, and large language models screen patients with higher accuracy than manual review.
The pharmaceutical industry spends over $200 billion on R&D annually, but success rates are below 12%, and it takes a decade to bring a drug to market. AI is compressing these timelines, cutting costs, and getting life-saving treatments to patients faster.
As Maria Chatzou Dunford, CEO and Co-founder of Lifebit, I’ve spent over 15 years at the intersection of AI and health-tech. I’ve seen AI-Powered Clinical Trials: Real-World Examples Changing Research in 2025 move from theory to practice, delivering measurable improvements in speed, cost, and patient outcomes. Let me show you how.
Slash Recruitment from Months to Minutes: 170x Faster, 93% Accurate AI Screening
The biggest challenge for trial coordinators is finding the right patients. They exist, but are often hidden in hospital records. This is why 80% of clinical trials miss their enrollment deadlines. The culprit is manual screening of electronic health records (EHRs) a process so slow it can take hours to evaluate a single patient.
AI changes this by scanning thousands of patient records in minutes, reading through years of doctor’s notes, lab results, and medical histories to identify ideal trial candidates instantly.
That’s exactly what’s happening in AI-Powered Clinical Trials: Real-World Examples Changing Research in 2025. And the results are nothing short of remarkable.
How AI Reads Doctor’s Notes to Find the Right Patients
Most critical patient information—up to 80% of it—is trapped in unstructured data like physician’s notes, discharge summaries, and pathology reports. This narrative text is nearly impossible to search efficiently with traditional keyword-based methods.
Enter Natural Language Processing (NLP). This branch of AI is trained to read and understand human language, extracting specific clinical concepts (a process called Named Entity Recognition) and understanding their context (e.g., distinguishing a patient’s diagnosis from a family history of the same condition). It acts like a superhuman research assistant, identifying key data points like disease stage, specific symptoms, prior treatments, and lifestyle factors that are crucial for eligibility but rarely found in structured fields.
The numbers tell the story. AI-powered platforms analyzing both structured and unstructured EHR data are identifying protocol-eligible patients three times faster with 93% accuracy. At Cleveland Clinic, one platform demonstrated a 170x speed improvement, changing patient recruitment across oncology, cardiology, and neurology trials. What used to take months now happens in days.
Think about what that means for a patient with aggressive cancer. Every week spent searching for trial participants is a week that patient doesn’t have access to a potentially life-saving treatment. AI isn’t just making research faster it’s giving patients time they desperately need.
More than half of all startups working in clinical AI are now focused on patient recruitment and protocol optimization, according to a recent report on AI in clinical development. This isn’t a future trend it’s happening right now.
Our federated AI platform is designed for this challenge. With built-in harmonization and advanced analytics, it extracts insights from diverse, siloed datasets across institutions, ensuring no eligible patient is overlooked.
Using Advanced AI to Boost Eligibility Screening
Finding potential patients is step one; verifying they meet complex eligibility criteria is step two. This traditionally involves manual chart review against lengthy checklists.
Large Language Models (LLMs) are taking this a step further. Unlike older NLP models that require extensive pre-training on specific clinical tasks, LLMs possess a broader, more nuanced understanding of language. They can interpret complex, multi-part eligibility criteria written in natural language—such as ‘patients with a history of metastatic non-small cell lung cancer who have failed at least one line of platinum-based chemotherapy but have not received immunotherapy’—and directly compare this logic against the narrative text in a patient’s record. This ability to handle complex boolean logic and clinical nuance makes them exceptionally powerful for pre-screening.
The RECTIFIER tool, pioneered by the Accelerator for Clinical Change research group, proved this in practice. In a pilot study, RECTIFIER determined patient eligibility with higher accuracy and specificity than study staff performing manual reviews. Not just faster more accurate.
The follow-up randomized controlled trial (MAPS-LLM) took this further. Researchers found that AI-assisted screening significantly improved both eligibility determination and enrollment rates compared to traditional manual methods. The team using AI could assess twice as many potentially eligible patients, dramatically accelerating enrollment. You can see the pilot study results for AI-driven eligibility tools for yourself.
This isn’t about replacing human expertise. It’s about freeing up study staff from manual chart review to focus on patient interaction, which drives enrollment and retention.
While current LLMs have cost and data processing limitations, the proven benefits of faster, more accurate screening and better enrollment rates show these tools are already worth the investment.
As AI-Powered Clinical Trials: Real-World Examples Changing Research in 2025 continue to evolve, these patient recruitment and screening innovations are laying the foundation for everything that follows. You can’t run a successful trial without patients. AI is finally solving that first, crucial challenge.
Cut Trial Timelines 30–50%: Predictive AI + Digital Twins That Work
After finding the right patients, the next challenge is designing a trial that works. Traditional design relies on guesswork, often leading to costly amendments, delays, or complete failure. AI is eliminating this trial-and-error approach.
We’re watching AI integration accelerate trial timelines by 30-50% and slash costs by up to 40%. These improvements are happening in 2025 through two breakthrough applications: predictive analytics that simulate trial outcomes, and “digital twins” that create virtual control groups.

Building Smarter, Faster Trials with Predictive Analytics
AI-driven predictive analytics allows researchers to run virtual clinical trials before committing millions to a real one.
These models digest massive historical datasets to simulate how different trial designs will perform, achieving up to 85% prediction accuracy for trial outcomes. It’s like having a crystal ball that actually works.
In practice, AI optimizes inclusion/exclusion criteria by identifying patient characteristics that predict success. It also spots potential bottlenecks, like poor site enrollment or overly restrictive criteria, before they derail a trial.
The impact on timelines is substantial. McKinsey data shows AI and machine learning have compressed development timelines by an average of six months per asset. When you’re racing to bring a life-saving therapy to market, six months means everything.
Site selection optimization is another area where predictive analytics shines. By analyzing site capabilities and historical performance, AI recommends optimal locations that can boost enrollment by 10-20%. Oncology trials using these tools have achieved 90% of their enrollment targets within planned timelines a stark contrast to the industry average.
At Lifebit, our platform’s analytics capabilities enable sponsors to simulate trial outcomes, test protocol designs, and compare endpoints. This proactive strategy identifies the most efficient and ethical approach, eliminating costly trial-and-error cycles and accelerating therapy delivery.
Creating ‘Digital Twins’ to Revolutionize Control Groups
The concept of “digital twins” is solving real ethical and practical problems in clinical trials today.
Traditional trials require a control group receiving a placebo, which creates an ethical dilemma. Patients may hesitate to enroll, fearing they won’t get the experimental therapy, which delays trials and increases costs.
Digital twins offer a solution. These are virtual patient profiles built from comprehensive historical trial data, real-world evidence, and genomic information. They are sophisticated replicas that mirror how actual patients would respond based on validated data.
By creating a virtual control arm from these profiles, researchers can dramatically reduce the number of real patients needed in control groups. This makes trials more attractive, accelerates enrollment, and maintains the statistical rigor needed for regulatory approval.
This approach, often called a Synthetic Control Arm (SCA), is gaining traction with regulators like the FDA, particularly for rare diseases. While rigorous validation is required, the agency’s guidance on real-world evidence shows an increasing openness to well-constructed external controls, which can reduce placebo exposure and accelerate development.
The approach has proven its value. Studies have demonstrated how digital twin methodology can reduce the number of participants required in Phase II oncology trial control groups while preserving statistical validity. This is particularly transformative for rare diseases, where patient populations are tiny.
The ethical benefits extend beyond recruitment. Fewer patients receiving placebos means fewer people denied potentially beneficial treatments during the trial. It’s a win for patients and researchers.
As AI-Powered Clinical Trials: Real-World Examples Changing Research in 2025 continue to mature, digital twins represent one of the most patient-centric innovations in clinical research. They prove that faster, cheaper trials don’t require ethical compromises AI is enabling us to design trials that are simultaneously more efficient and more humane.
Catch Adverse Events Early (90% Sensitivity): DCTs Boost Compliance 30%
Clinical trials are undergoing a fundamental shift. Instead of requiring travel to research centers for one-size-fits-all treatments, AI-Powered Clinical Trials: Real-World Examples Changing Research in 2025 are enabling decentralized clinical trials (DCTs) and personalized medicine.
This dual change is making trials more accessible to diverse patient populations while dramatically improving their effectiveness. AI serves as the engine driving both these changes, turning continuous streams of real-world data into actionable insights.

Using Wearables and Digital Biomarkers for 24/7 Oversight
Instead of rigid clinic visits that capture only snapshots of a patient’s health, AI-driven decentralized trials use wearables and sensors to continuously monitor health during daily life.
Wearable devices collect real-world evidence (RWE) around the clock vital signs, activity levels, sleep patterns, and more. AI algorithms analyze this continuous data stream, detecting subtle patterns that might signal an adverse event. These digital biomarkers are objective, quantifiable measures of health state collected by digital devices. For example, in a Parkinson’s trial, subtle changes in gait and tremor frequency detected by a smartwatch can indicate disease progression or a drug’s effect. In a respiratory trial, a sensor’s ability to count coughs per hour provides a more accurate measure of treatment efficacy than a patient’s self-reported diary. This continuous monitoring enables 90% sensitivity for adverse event detection, catching safety concerns far earlier than periodic clinic assessments.
Beyond safety, AI-powered engagement strategies like gamification and personalized reminders improve patient adherence, leading to an over 30% increase in patient compliance rates in remote studies.
Our federated AI platform plays a crucial role in making this possible. It enables secure, real-time access to global biomedical and multi-omic data from these diverse sources, generating real-time insights while maintaining strict privacy protections. This capability is essential for facilitating secure collaboration across hybrid data ecosystems, ensuring that the wealth of real-world data collected through wearables can be analyzed effectively without compromising patient confidentiality.
Tailoring Treatments with AI for Personalized Medicine
The era of one-size-fits-all medicine is ending. AI enables treatments to be precisely matched to a patient’s unique biological profile.
By analyzing vast amounts of multi-omic data (genomics, proteomics, etc.), AI can identify complex biomarkers that predict a patient’s response. Machine learning is essential for integrating these massive, disparate datasets to uncover novel biological signatures that a single data type would miss, creating a holistic profile of each patient. These models forecast individual patient responses, allowing clinicians to customize treatment plans before a single dose is administered.
In oncology, this is already saving lives. Comprehensive genomic profiling (CGP) panels, analyzed with AI, identify actionable mutations in far more tumors (67% vs. 33% for smaller panels). Matching patients to precision therapies based on this data dramatically improves survival rates.
Patient stratification has become far more sophisticated. Instead of broad categories, AI segments patient populations based on detailed biological profiles, ensuring that clinical trials recruit participants most likely to benefit. This targeted approach doesn’t just increase trial success rates it advances precision oncology by connecting each patient with the therapy that gives them the best chance.
Our federated AI platform stands at the forefront of this revolution. With built-in capabilities for harmonization and advanced AI/ML analytics, we provide secure, real-time access to global biomedical and multi-omic data. This empowers researchers to open up the full potential of personalized medicine, moving beyond generalized treatments to therapies that are truly custom to individual patients. More info about our federated AI platform.
The convergence of decentralized trials and personalized medicine represents a fundamental reimagining of clinical research one where patients participate from home while receiving treatments designed for their unique biology.
AI in Trials: Cut Cost, Reduce Risk, Move Faster—Your Key Questions Answered
The integration of AI into clinical trials is transformative, but it also raises important questions. Let’s address the most common concerns from researchers, clinicians, and patients.
What are the biggest challenges AI helps solve in clinical trials?
AI tackles the decades-old problems that delay treatments, drain budgets, and frustrate researchers.
Patient recruitment delays are a critical bottleneck, with 80% of trials missing enrollment deadlines. AI-powered tools are improving enrollment rates by 65% by scanning vast datasets to find candidates in days, not months.
High operational costs burden the pharmaceutical industry. AI integration is reducing these costs by up to 40% through automation, protocol optimization, and improved efficiency.
Data quality issues can plague up to 50% of trial datasets. AI addresses this by standardizing unstructured data, harmonizing information, and performing automated quality checks, resulting in more trustworthy data.
High failure rates remain persistent, with success rates below 12%. AI’s predictive analytics models, which achieve 85% accuracy in forecasting outcomes, help researchers optimize trial design and patient selection, significantly increasing the chances of success.
By addressing these challenges, AI-Powered Clinical Trials: Real-World Examples Changing Research in 2025 make research faster, more affordable, and more successful, getting treatments to patients years sooner.
Is AI replacing doctors and researchers in clinical trials?
No. The future is a hybrid human-AI approach, where AI serves as a powerful co-pilot, not a replacement.
AI excels at tedious, data-intensive tasks: screening thousands of electronic health records, analyzing complex genomic datasets, or monitoring digital biomarker data. This automates repetitive work so doctors and researchers can focus on what they do best making critical decisions, providing care, and advancing medical knowledge.
What AI can’t do is apply clinical judgment, understand a patient’s nuanced situation, or provide compassionate care. Human oversight and interpretation remain essential.
What are the main ethical concerns with using AI in trials?
The rapid adoption of AI brings legitimate ethical concerns that require careful attention.
Algorithmic bias poses a significant risk. AI models trained on historical data can perpetuate or amplify existing healthcare biases if the data underrepresents certain populations. For example, if an AI model for screening cardiology trial candidates is trained primarily on data from white male patients, it may learn to associate symptoms or risk factors with that demographic. As a result, it could fail to identify eligible female patients or patients from minority ethnic groups whose symptoms present differently, effectively locking them out of potentially life-saving research. Preventing this requires not only using inclusive datasets for training but also continuous auditing of the model’s performance across different demographic subgroups to detect and correct for bias.
Data privacy and security are paramount. Analyzing vast, federated datasets requires robust security and compliance with regulations like GDPR and HIPAA. Our federated AI platform is designed with privacy-preserving techniques to ensure data remains secure during large-scale analysis.
Patient autonomy and transparency must be maintained. Patients have a right to understand how their data is used and how AI influences decisions. Clear communication, transparent consent, and explainable AI (XAI) are essential to address the “black box” problem and maintain trust. A “black box” AI model provides a prediction (e.g., “this patient is a good candidate”) without explaining its reasoning. XAI techniques are designed to open that box by showing which patient data points most influenced the model’s decision. This allows a clinician to review the AI’s logic, verify its soundness, and confidently explain the recommendation to the patient, ensuring human oversight and preserving trust.
Regulatory uncertainty adds complexity. Regulatory bodies like the FDA and MHRA are developing frameworks for AI in drug development. These risk-based approaches aim to ensure safety without stifling innovation. We actively engage with these evolving guidelines to ensure our solutions meet the highest standards. The FDA discussion on AI/ML in drug development provides valuable insight into how regulators are thinking about these challenges.
Addressing these ethical concerns requires collaboration among technology developers, clinical researchers, regulators, and patient advocates. We must ensure AI tools are implemented responsibly, equitably, and with patients’ best interests at the center of every decision.
Deploy Federated AI Now: Cut Trial Costs 40% Without Moving Data
As we’ve seen, AI-Powered Clinical Trials: Real-World Examples Changing Research in 2025 are delivering measurable results. From finding patients 170x faster to cutting costs by 40%, AI is changing trial design, patient monitoring, and personalized medicine. These are not future promises; they are happening today.
However, the full potential of AI remains locked behind key challenges: evolving regulatory frameworks, legitimate data security concerns, and pervasive data silos that isolate valuable information.
Federated learning is the solution. It trains AI models across multiple institutions without any raw data ever leaving its secure, private location. The model learns from collective data while the information stays protected. This is what federated learning, including advanced approaches like swarm learning, makes possible today.
The challenge isn’t just technological. Even as AI capabilities advance, adoption often lags due to infrastructural limitations, data harmonization complexity, and the need for robust governance frameworks.
At Lifebit, our federated AI platform solves these problems, enabling secure, real-time access to global biomedical data across biopharma, government, and public health organizations on five continents.
Our platform components, including our Trusted Research Environment (TRE) and R.E.A.L. analytics layer, deliver real-time insights with the highest security and governance standards, ensuring compliance with regulations like GDPR and HIPAA.
The future of clinical trials is a connected, intelligent ecosystem. It’s where data flows securely, AI models learn collectively, and researchers collaborate without compromise. By preserving privacy while accelerating findy, we can cut costs, improve outcomes, and get life-saving treatments to patients faster, everywhere.
The race against time in medical research is one we can win. With secure, collaborative, and ethically sound AI solutions, we’re opening up a new era of medical breakthroughs. Discover how Lifebit’s federated platform is transforming research and helping us all build a healthier future.

