AI in Diagnostics: A Doctor’s New Best Friend

AI powered diagnostics: Your Best Ally 2025
Why AI Powered Diagnostics Matters Now
AI powered diagnostics is revolutionizing disease detection, diagnosis, and treatment, marking a fundamental turning point for a healthcare industry grappling with unprecedented challenges. By analyzing vast, complex collections of medical data—including images, electronic health records (EHRs), genomic sequences, and lab results—AI operates with a speed and precision that far surpasses traditional methods. The urgency for this transformation is clear, driven by a perfect storm of data overload, persistent diagnostic errors, and a growing shortage of medical specialists.
The modern hospital is drowning in data. With an estimated 3.6 billion imaging procedures performed globally each year, the resulting information overwhelms manual processing capabilities. Shockingly, it’s estimated that 97% of all hospital data, particularly from imaging, goes unused for broader analysis after the initial diagnostic read. This is a colossal missed opportunity, a digital graveyard of insights that could predict disease outbreaks, refine treatment protocols, and save lives. AI provides the tools to finally mine this valuable resource at scale.
This data deluge contributes to a critical patient safety issue: diagnostic errors. Affecting an estimated 12 million Americans annually, these errors are a leading cause of patient harm and are implicated as the third leading cause of death in the United States. They often stem not from a lack of knowledge, but from cognitive biases, fatigue, and the sheer complexity of interpreting ambiguous information under pressure. AI, with its ability to tirelessly and objectively analyze data, acts as a crucial safety net, flagging subtle anomalies that the human eye might miss.
Compounding this issue is a worldwide shortage of specialists. Many regions face a critical lack of radiologists, pathologists, and other diagnostic experts, leaving millions without access to timely, high-quality care. AI powered diagnostics helps bridge this gap, acting as a force multiplier that brings specialist-level insights to underserved communities and general practitioners. It democratizes expertise, ensuring a patient’s location doesn’t determine their outcome.
Key benefits of this technological shift include:
- Unprecedented Speed: AI algorithms can analyze a complex medical scan or a patient’s entire medical history in seconds, not hours or days, accelerating the entire diagnostic workflow.
- Enhanced Accuracy: In fields like cardiology, AI systems have demonstrated up to 93% accuracy in classifying heart disease, reducing dangerous false negatives and costly false positives.
- Proactive Early Detection: By identifying faint disease markers long before they become symptomatic, AI dramatically improves outcomes. For breast cancer, survival rates can jump from a grim 14% for late-stage diagnosis to over 90% when caught early.
AI is not replacing doctors; it is augmenting them, freeing them from repetitive, data-intensive tasks to focus on what humans do best: complex decision-making, patient communication, and empathy. By learning from millions of anonymized cases, these algorithms provide consistent, evidence-based support, working 24/7 to elevate the standard of care. The momentum is undeniable: nearly 400 FDA-approved AI algorithms are already in use for radiology, and over 48% of hospital CEOs expect their systems to be fully AI-ready by 2028. However, this revolution also brings challenges—ensuring AI is unbiased, protecting patient privacy, and creating regulatory frameworks that foster innovation while guaranteeing safety.
I’m Dr. Maria Chatzou Dunford, CEO and Co-founder of Lifebit. We build federated AI platforms for secure, compliant analysis of genomic and biomedical data—including AI powered diagnostics—across siloed systems. My work in computational biology and precision medicine has shown me how AI can open up insights from complex datasets while respecting data sovereignty and patient privacy.
How AI Boosts Diagnostic Speed and Accuracy
Imagine a patient arriving in a busy emergency room with acute chest pain. The traditional diagnostic pathway is a race against time, fraught with uncertainty. It involves a physical exam, an electrocardiogram (ECG) that requires expert interpretation, a series of blood tests to measure cardiac enzymes like troponin, and a chest X-ray to rule out other conditions. This process can take hours, with each step representing a potential delay while the patient’s heart muscle could be sustaining irreversible damage. With AI powered diagnostics, this entire workflow is supercharged. An AI algorithm can analyze the ECG in seconds, immediately flagging signs of a heart attack with high accuracy. Simultaneously, another algorithm can scan the chest X-ray, prioritizing it on the radiologist’s worklist if it detects a life-threatening issue like an aortic dissection. By integrating these findings with the patient’s EHR data and incoming lab results, AI provides a comprehensive risk score in minutes, enabling clinicians to act with unprecedented speed and confidence.
This is not a futuristic scenario; it is happening now in hospitals worldwide. AI is fundamentally shifting healthcare from a reactive model, which primarily responds to symptoms, to a proactive and predictive one that catches diseases before they become life-threatening. The benefits are tangible and measurable: increased operational efficiency as AI handles the initial review of thousands of scans, freeing up radiologists to focus on the most complex cases; a significant reduction in diagnostic errors, which affect 12 million Americans annually; and faster, more informed decision-making that leads directly to earlier treatment and better patient outcomes.
Crucially, AI’s power comes from its ability to process and learn from massive datasets. A single physician, over a lifetime, may see thousands of cases. An AI model can be trained on millions, allowing it to recognize incredibly subtle patterns and correlations across lab results, imaging data, and genetic information that are simply impossible for a human to perceive.
Improving on Traditional Methods
For decades, clinicians have relied on scoring systems like the Modified Early Warning Score (MEWS) to predict a patient’s risk of sudden deterioration. MEWS is a simple but effective tool that calculates a risk score based on five basic vital signs: heart rate, blood pressure, respiratory rate, temperature, and level of consciousness. It has undoubtedly saved lives by providing a standardized method for flagging at-risk patients.
However, MEWS is inherently limited. It is a manual, point-in-time calculation that fails to capture trends. It uses a very small number of data points and is not personalized to a patient’s specific comorbidities or medical history. Its simplicity also leads to a high rate of false alarms, contributing to “alarm fatigue” where busy clinical staff may begin to ignore alerts. It’s like predicting a hurricane by looking at a single barometer reading—helpful, but dangerously incomplete.
AI completely changes the game. An AI-powered system can analyze hundreds of variables simultaneously in real-time. It processes both structured data (like hourly vital signs, lab test results, and medication logs) and unstructured data (like the nuanced text in a doctor’s or nurse’s notes). By tracking these variables over time, it learns a patient’s unique physiological baseline and can detect subtle deviations that signal impending crisis.
The results are striking. Scientific research has shown that AI models consistently outperform traditional scoring systems like MEWS in predicting patient deterioration, often providing warnings hours earlier and with fewer false alarms. The AI doesn’t just calculate faster—it achieves superior pattern recognition. It’s the difference between a single weather station and a global network of satellites, ocean buoys, and atmospheric sensors, all feeding into a sophisticated predictive model.
The Accuracy Advantage in Numbers
In cardiology, AI powered diagnostics has achieved 93% accuracy rates in heart disease classification. Algorithms can analyze an ECG to detect atrial fibrillation, a common and dangerous heart rhythm abnormality, with a precision that often exceeds that of general practitioners. In echocardiography, AI can automatically calculate a patient’s ejection fraction—a key measure of heart function—freeing cardiologists from a time-consuming manual task and reducing inter-observer variability.
This level of precision is critical. It reduces false positives, which lead to patient anxiety, unnecessary follow-up procedures, and wasted healthcare resources. More importantly, it reliably catches true positives, ensuring that patients who need urgent care receive it promptly.
The impact is perhaps most profound in cancer survival. For diseases like breast or colorectal cancer, early detection can mean a 90% five-year survival rate, a figure that plummets to as low as 14% if the cancer is not found until it has metastasized. AI powered diagnostics excels at this early detection. In the field of digital pathology, AI algorithms can scan high-resolution images of tissue biopsies, identifying tiny clusters of cancer cells (micrometastases) that a human pathologist, under time pressure and facing a heavy caseload, might overlook. It’s like having a tireless specialist with a photographic memory of millions of cases working alongside every doctor.
Evidence from cardiology research confirms that AI doesn’t just match human accuracy—in many specific, well-defined tasks, it surpasses it, and does so with perfect consistency, 24 hours a day, without fatigue. The bottom line is faster, more accurate diagnoses, earlier detection, and demonstrably better patient outcomes. AI in diagnostics is no longer a theoretical promise; it is a clinical reality.
Key Applications of AI in Medical Diagnostics Today
In the modern hospital, AI powered diagnostics is no longer an experimental technology but an essential clinical tool, working behind the scenes across a growing number of specialties. Doctors are actively using these tools to diagnose diseases earlier, more accurately, and more efficiently. From the radiology reading room to the oncology clinic, AI is augmenting human expertise and, most excitingly, democratizing access to specialist-level care, extending it from elite academic centers to rural clinics and underserved communities worldwide.
Revolutionizing Medical Imaging and Radiology
Hospitals perform 3.6 billion imaging procedures annually, yet an estimated 97% of this data goes unused for secondary analysis. AI is unlocking the life-saving insights hidden in this vast, untapped resource. With nearly 400 FDA-approved AI algorithms for radiology now on the market, AI is transforming the workflow. These tools act as a first-line reader, automatically analyzing X-rays for signs of pneumonia or a collapsed lung (pneumothorax), scanning head CT images for intracranial hemorrhage, and reviewing mammograms for suspicious lesions. A key application is worklist prioritization. The AI can triage the entire queue of scans, pushing images with critical findings to the top of the radiologist’s list, ensuring that the sickest patients get attention first. This dramatically reduces turnaround times for urgent diagnoses. These algorithms, trained on millions of scans from diverse populations, provide a second set of eyes that never gets tired, helping to catch subtle abnormalities and improve diagnostic consistency across the board.
At Lifebit, our federated AI platform is designed to securely unlock the value in this unused data. By allowing hospitals to collaborate on training AI models without ever moving or exposing sensitive patient images, we enable the creation of more robust and accurate algorithms from globally diverse datasets, directly improving diagnostic accuracy for all. Learn more about how leveraging unused imaging data can transform healthcare.
Early Disease Detection and Personalized Oncology
In the race against cancer, AI powered diagnostics provides a game-changing advantage. The field of digital pathology is a prime example. AI algorithms can analyze gigapixel-sized whole-slide images of tumor biopsies with meticulous detail, identifying and counting cancer cells, grading tumor aggressiveness, and even spotting micrometastases that might be missed by the human eye. Beyond just detection, AI is enabling radiogenomics—the ability to predict a tumor’s molecular profile and genetic mutations directly from its appearance on a medical image. An AI model from Harvard Medical School, for instance, achieved nearly 94% accuracy in detecting 11 different cancer types and could predict patient survival from pathology images alone. This offers a rapid, low-cost alternative to genomic sequencing. The impact on survival is profound: early detection of breast or colorectal cancer can push five-year survival rates from as low as 14% to over 90%. The real revolution, however, is in personalized oncology. By analyzing a tumor’s unique genetic and microenvironmental characteristics, AI can help predict which therapies—including chemotherapy, targeted drugs, or immunotherapies—will be most effective for a specific patient, ushering in an era of true precision medicine. For more on this, see research on AI’s role in transforming oncology.
Transforming Cardiology and Neurology
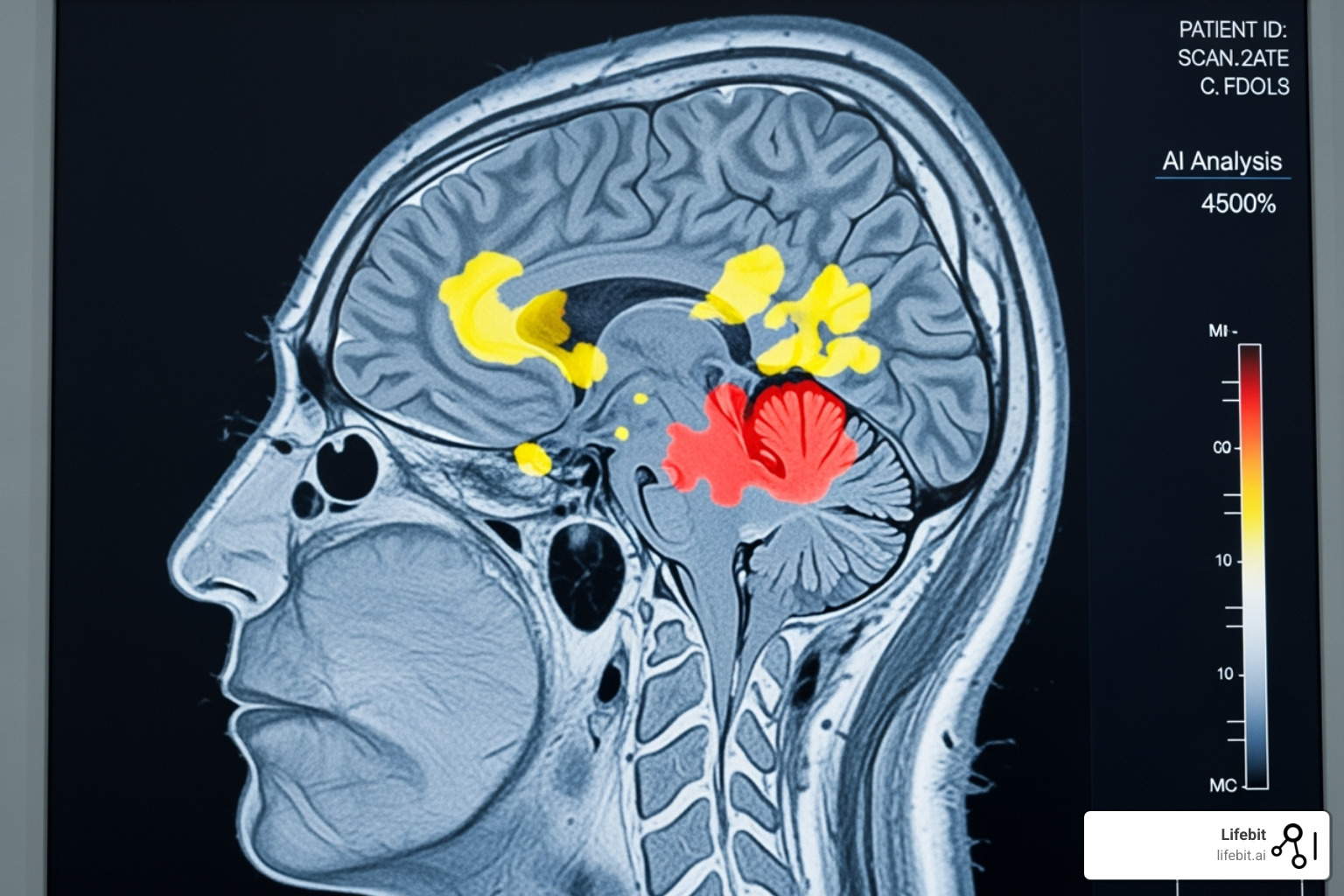
AI’s impact extends deep into other complex specialties. In cardiology, AI is being deployed in consumer-grade wearables to provide real-time ECG analysis for detecting arrhythmias like atrial fibrillation. In the hospital, it automates the analysis of echocardiograms, providing fast and reproducible measurements of cardiac function, such as ejection fraction. In neurology, AI algorithms are analyzing brain MRIs to detect the subtle, early signs of neurodegenerative diseases like Alzheimer’s (by measuring hippocampal volume) or to track the progression of lesions in multiple sclerosis. This allows for earlier intervention and more precise monitoring of treatment efficacy. Furthermore, AI is moving beyond imaging, analyzing speech patterns, gait, and even typing cadence to identify early markers of conditions like Parkinson’s disease, long before significant clinical symptoms emerge.
AI Powered Diagnostics for Underserved Communities
Perhaps AI’s most profound potential lies in its ability to bring world-class diagnostics to the most remote and underserved corners of the globe. In regions with few or no specialists, people often die from easily treatable diseases due to a lack of timely diagnosis. AI powered diagnostics democratizes this expertise. For example, a mobile app using AI in Liberia can help predict malaria outbreaks, protecting vulnerable communities. In India and Thailand, AI-powered systems are providing free diabetic retinopathy screenings to millions, using a simple fundus camera to detect the condition and prevent blindness. A community health worker in a rural village, equipped with an AI-guided portable ultrasound device, can now perform obstetric scans that once required a highly trained sonographer, helping to ensure safer pregnancies and deliveries. This isn’t about replacing doctors—it’s about extending their reach and impact, making healthcare more equitable for everyone. Lifebit’s federated approach is crucial for this global effort, enabling the development of AI models trained on diverse populations without compromising local data privacy. For an inspiring example, check out this AI-powered app for malaria prediction in Liberia.
Overcoming the Problems to Widespread AI Adoption
While the potential of AI powered diagnostics is transformative, its journey from promising algorithm to standard clinical practice is fraught with significant obstacles. Widespread adoption hinges on overcoming a complex web of technical, regulatory, and ethical challenges. Successfully navigating these issues will determine whether AI fulfills its promise to revolutionize healthcare or remains a niche technology.

Navigating Technical and Regulatory Roadblocks
Implementing AI in a clinical setting is far more complex than simply installing new software. It requires a fundamental overhaul of data infrastructure and workflows.
- Data Quality and Interoperability: An AI model is only as good as the data it’s trained on. Healthcare data is notoriously fragmented, inconsistent, and siloed in proprietary Electronic Health Record (EHR) systems. Data standards like FHIR (Fast Healthcare Interoperability Resources) and DICOM (Digital Imaging and Communications in Medicine) exist to promote interoperability, but their adoption is far from universal. Without standardized, high-quality data, AI models can produce unreliable or even dangerous results. Building the infrastructure to clean, standardize, and securely exchange this data is a massive but essential undertaking.
- Infrastructure and Integration: Hospitals need significant investment in IT infrastructure, including robust computing power, high-speed networks, and secure cloud storage, to support AI applications. Furthermore, these tools must be seamlessly integrated into existing clinical workflows (like the radiologist’s picture archiving and communication system, or PACS) to be effective. A clunky or disruptive tool, no matter how accurate, will not be adopted by busy clinicians.
- The Evolving Regulatory Landscape: Traditional regulatory pathways, like those of the FDA, were designed for static medical devices, not for AI algorithms that can continuously learn and evolve. Regulators are working to adapt, creating new frameworks like the “Software as a Medical Device (SaMD)” category and pathways for a “predetermined change control plan,” which allows developers to pre-specify how their algorithm will learn over time. However, striking the right balance between fostering rapid innovation and ensuring rigorous patient safety remains a major challenge.
Despite these hurdles, the commitment from healthcare leaders is strong. More than 48% of hospital CEOs are confident that by 2028, their systems will have the necessary infrastructure to fully integrate AI into clinical decision-making.
Addressing the Ethical Dilemmas of AI Powered Diagnostics
Beyond the technical problems, a series of profound ethical dilemmas must be addressed to build and maintain trust in AI among both clinicians and patients.
- Patient Data Privacy and Security: AI models require access to vast amounts of sensitive patient information. Ensuring robust cybersecurity and strict adherence to privacy regulations like HIPAA and GDPR is non-negotiable. Technologies like federated learning, which Lifebit champions, are critical. In this model, the AI algorithm is sent to train on data locally within a hospital’s secure firewall. Only the anonymous, aggregated mathematical learnings are sent back to improve a central model, meaning the sensitive patient data never leaves the hospital’s control.
- Algorithmic Bias and Equity: If an AI model is trained on data from a predominantly white, male population, it may perform poorly when used on women or people of color. For example, a dermatology AI trained on light skin tones may fail to accurately identify melanoma on darker skin, thereby exacerbating existing health disparities. Mitigating this requires a conscious effort to build and validate models on diverse, representative datasets and to conduct regular fairness audits.
- The “Black Box” Problem and Explainability: Many of the most powerful deep learning models are considered “black boxes,” meaning even their creators cannot fully explain how they arrive at a specific conclusion. This is a major barrier to clinical trust. The field of Explainable AI (XAI) is working to create models that can provide their reasoning (e.g., by highlighting the specific pixels in an image that led to its diagnosis), making the AI’s output transparent and auditable.
- Accountability and Liability: If an AI system contributes to a misdiagnosis, who is responsible? The software developer, the hospital that implemented it, or the clinician who accepted its recommendation? Clear legal and professional frameworks for this new shared-responsibility model are urgently needed to define liability and ensure accountability.
- Automation Bias: This is the well-documented human tendency to over-rely on and trust automated systems. A clinician, fatigued at the end of a long shift, might be tempted to accept an AI’s recommendation without a proper critical review. The goal of AI is to augment human intelligence, not replace it. Proper training and a culture of critical engagement with AI tools are essential to prevent this.
At Lifebit, our federated AI platform is built from the ground up to address these challenges, enabling secure, compliant, and ethical analysis across siloed systems while respecting data sovereignty and patient privacy. We are committed to making AI powered diagnostics not just powerful, but also trustworthy.
The Future of Diagnostics: What’s on the Horizon?
The story of AI powered diagnostics is just beginning. We are on the cusp of a healthcare paradigm shift toward a system that is hyper-personalized, predictive, and proactive. The focus is moving beyond simply diagnosing existing illness to anticipating disease before symptoms ever appear and crafting therapies customized to an individual’s unique biology. This future is being built today on a foundation of generative AI, ambient intelligence, and the long-term promise of quantum computing.
Generative AI, Digital Twins, and Beyond
Generative AI (GAI), the technology behind tools like ChatGPT, is already making a significant impact. One of its most powerful applications is the creation of high-fidelity synthetic patient data. Using techniques like Generative Adversarial Networks (GANs), GAI can create realistic but entirely artificial medical data—from MRI scans to EHRs. This solves two major problems: it protects patient privacy and it helps overcome data scarcity for training models on rare diseases. GAI is also powering sophisticated conversational diagnostic tools that can engage in nuanced dialogue, triage patients, and even demonstrate superior empathy and communication skills in simulations, promising to vastly expand access to quality healthcare advice.
Another emerging concept is Ambient Clinical Intelligence. These systems use AI to listen to and analyze the natural conversation between a doctor and patient during a visit. The AI then automatically generates clinical notes, populates the EHR, and queues up orders for tests and prescriptions. This technology promises to alleviate a major source of physician burnout—the hours spent on administrative data entry—and return the doctor’s focus to the patient.
Perhaps the most ambitious vision is the Digital Twin: a dynamic, virtual model of a specific patient. This digital twin would be continuously updated with data from their EHR, genomic profile, real-time physiological data from wearables, and lifestyle factors. Clinicians could use this model to simulate the progression of a chronic disease over decades, identify the optimal points for intervention, and test the efficacy and potential side effects of different drug regimens in silico before ever administering them to the real patient. It represents the ultimate in personalized, predictive medicine.
Further on the horizon is Quantum AI (QAI). While still in its infancy, quantum computing’s unprecedented power could solve problems currently intractable for even the most powerful supercomputers. This could include simulating the complex folding of proteins to discover new drugs, or instantly analyzing massive, multi-omic datasets to find previously invisible disease patterns.
Here’s how these technologies compare across key diagnostic capabilities:
| Technology | Current AI Capabilities in Diagnostics | Future GAI Potential in Diagnostics | Future Digital Twin / Quantum AI Potential |
|---|---|---|---|
| Data Analysis | Pattern recognition in structured/unstructured data; Image analysis (X-rays, MRI); Basic predictive models. | Generate synthetic patient data for training; Create comprehensive patient profiles from EHRs; Power conversational diagnostic agents. | Digital Twin: Longitudinal, multi-modal patient simulation. Quantum: Real-time analysis of massive, multi-omic datasets; Complex molecular modeling. |
| Accuracy & Speed | High accuracy for specific tasks (e.g., 93% for heart disease); Faster than manual review. | Improved diagnostic accuracy through conversational AI; Reduced data bias in training datasets; Automated report generation. | Digital Twin: Predictive accuracy for individual patient trajectories. Quantum: Near-perfect accuracy for complex diseases; Instantaneous processing. |
| Applications | Radiology assistance; Early cancer detection; Cardiovascular risk assessment; Sepsis prediction. | Ambient clinical intelligence (automated notes); Personalized patient education; Pre-consultation triage. | Digital Twin: Proactive disease prevention; In silico clinical trials. Quantum: Novel biomarker discovery; Design of new diagnostic tests. |
| Challenges | Data quality; Algorithmic bias; Regulatory hurdles; Explainability. | Ensuring clinical validity of synthetic data; Ethical use of conversational AI; Hallucination and factuality. | Digital Twin: Massive computational cost; Data integration. Quantum: Hardware immaturity; Algorithm development. |
The Rise of Personalized Treatment Plans
Accurate diagnosis is just the first step. The ultimate goal is to deliver the right treatment to the right patient at the right time. AI powered diagnostics is the engine of this personalization. AI-driven therapy selection is already a game-changer. By analyzing a patient’s medical history, genetic profile, and tumor characteristics, AI can help predict their likely response to different treatments. Advanced AI software can now predict disease-causing genetic mutations with high accuracy by learning from genetic variants across millions of years of evolution. This enables the creation of polygenic risk scores that work across diverse ancestries, a crucial step toward making precision medicine equitable for all populations.
This represents a fundamental shift from diagnosis to prognosis, and from reactive medicine to proactive, preventative care. We are moving away from one-size-fits-all protocols and toward treatments that are exquisitely customized to a person’s unique molecular and digital signature.
At Lifebit, we build the secure, federated infrastructure for this future. Our platform enables the complex analysis of genomic and multi-omic data across siloed systems, allowing researchers to build and validate the next generation of predictive models and digital twins while respecting data sovereignty and patient privacy. We create the trusted research environments where AI powered diagnostics can safely and ethically reach its full potential.
Conclusion
Healthcare is undergoing a profound transformation, with AI powered diagnostics at its very core. AI is not a threat to clinicians, but rather their most powerful collaborator. It is an assistant that works tirelessly, analyzes millions of data points in the blink of an eye, and identifies subtle, complex patterns that even the most experienced human expert might miss. By shouldering the burden of data processing and preliminary analysis, AI gives providers their time back, allowing them to focus on the uniquely human aspects of medicine: critical thinking, building patient rapport, and making nuanced, empathetic decisions. This collaborative future, merging the computational power of AI with the wisdom of human experience, will create a healthcare system far more powerful than the sum of its parts.
Realizing this vision requires concerted effort. We must continue to break down technical barriers like data silos and build the interoperable infrastructure AI needs to thrive. We must work with regulators to create agile frameworks that ensure safety without stifling innovation. Most importantly, we must confront the ethical questions head-on: actively working to eliminate algorithmic bias, fortifying patient privacy through technologies like federated learning, and establishing clear lines of accountability. Building trust and ensuring that the benefits of AI are distributed equitably are the cornerstones of democratizing these powerful technologies.
At Lifebit, we are dedicated to building this future responsibly. Our federated AI platform is designed to unlock insights from the world’s most sensitive biomedical datasets while keeping them secure, private, and in the control of their owners. Our platform, including our Trusted Research Environment and R.E.A.L. technology, enables advanced AI powered diagnostics and analytics across global datasets without compromising data sovereignty. With built-in data harmonization, advanced AI/ML analytics, and robust federated governance, we provide the secure, compliant, and scalable infrastructure for biopharma, governments, and public health organizations to turn the promise of AI into a clinical reality.
The result is actionable intelligence that respects both data and patients. The future of medicine will be more precise, more predictive, more accessible, and, ultimately, more human. By embracing these advancements with foresight and integrity, we can build a healthcare system that not only treats illness but actively predicts and prevents it, all while upholding the principles of human dignity and health equity.
Learn how our Trusted Research Environment enables secure AI innovation.

