Click, Recruit, Succeed – Understanding Digital Clinical Trial Recruitment Results

The Recruitment Crisis and the Digital Solution
Clinical trials are stalling: 80 % miss enrollment targets and every delayed day can cost millions. Yet patients are more connected than ever. By moving outreach online—and coupling it with federated data analytics—we can match the right volunteers to the right studies faster, more affordably and with far less burden on participants and sites alike.
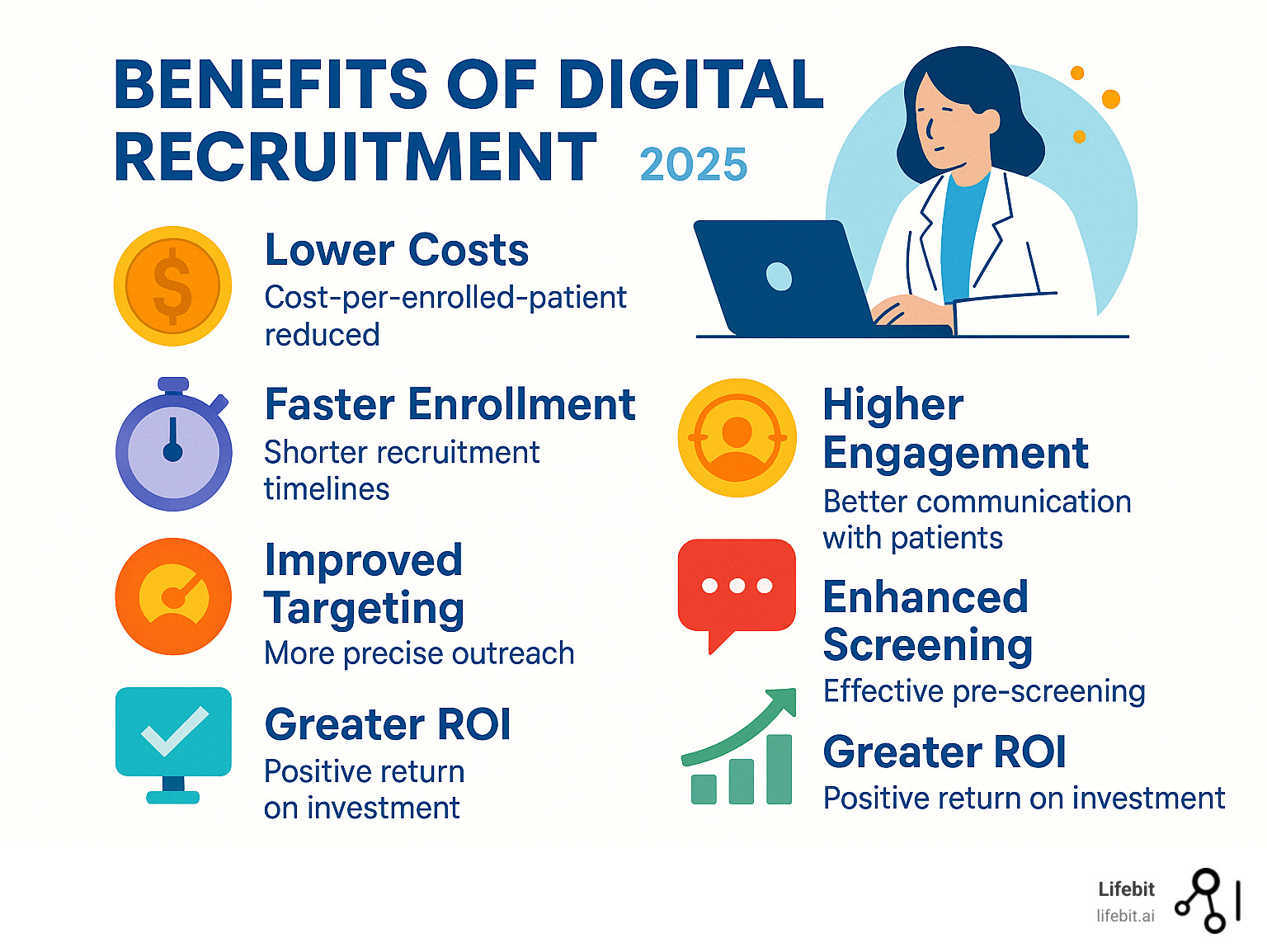
The Digital Advantage: Quantifying the Impact on Recruitment Timelines and Costs
Digital recruitment is no longer experimental—it consistently delivers measurable gains. Trials that blend digital and traditional outreach report a 156 % jump in qualified inquiries, shave an average 4.2 months off enrollment timelines, and cut cost-per-referral by roughly 30 %. In an industry where each day of delay can cost millions, those numbers matter.
Peer-reviewed studies, including work published in npj Digital Medicine, confirm that the most successful teams use a hybrid model: broad digital reach combined with the personal credibility of physicians. The result is faster activation, lower budgets and—most importantly—earlier patient access to life-changing therapies.
Real-World Case Studies: Digital Success Stories
The impact of digital recruitment becomes even clearer when examining specific case studies across different therapeutic areas:
Oncology Trial Success: A Phase III cancer study struggling with traditional recruitment methods implemented a comprehensive digital strategy combining Facebook advertising, Google Ads, and patient advocacy group partnerships. Within six months, they achieved 120% of their enrollment target, reducing their recruitment timeline from 18 months to 11 months. The cost per enrolled patient dropped from $8,500 to $5,200, representing a 39% cost reduction.
Rare Disease Breakthrough: A study for a rare genetic disorder affecting fewer than 10,000 people globally leveraged specialized online communities and patient registries. By creating targeted content in multiple languages and partnering with international patient advocacy organizations, they successfully enrolled 85% of their target population across 12 countries—something that would have been nearly impossible through traditional site-based recruitment alone.
Mental Health Innovation: A depression study used social media advertising with carefully crafted messaging that reduced stigma while encouraging participation. The digital approach not only doubled their enrollment rate but also attracted a more diverse participant pool, with 40% higher representation from underserved communities compared to their previous traditional recruitment efforts.
Measuring Digital Results: Key Metrics for Success
We track a focused set of KPIs to keep progress transparent and to course-correct in real time:
- Cost-per-lead (CPL) – spend to generate one qualified inquiry
- Cost-per-enrolled-patient (CPEP) – total spend to randomize one participant
- Enrollment rate – percentage of qualified leads that progress to consent
- Screen-fail rate – proportion of prescreened candidates ultimately ineligible
- Timeline reduction – months saved versus historical averages
- Return on Investment (ROI) – financial impact of all the metrics above
- Digital engagement metrics – click-through rates, time spent on study materials, and social media engagement
- Geographic reach – expansion of recruitment beyond traditional site catchment areas
- Demographic diversity – representation across age, ethnicity, and socioeconomic groups
Monitoring these indicators ensures we are not only filling trials, but doing so efficiently and with the right participants. Advanced analytics platforms now allow real-time dashboard monitoring, enabling recruitment teams to pivot strategies within days rather than months when certain channels underperform.
The Economics of Digital Change
The financial implications of digital recruitment extend far beyond simple cost-per-patient calculations. Consider the broader economic impact:
Reduced Site Burden: Traditional recruitment places enormous pressure on clinical sites, with staff spending up to 40% of their time on recruitment activities. Digital pre-screening and automated qualification processes can reduce this burden by 60%, allowing sites to focus on patient care and protocol compliance.
Faster Time-to-Market: Every month saved in recruitment translates to earlier drug approval and market entry. For a blockbuster drug with potential annual sales of $1 billion, each month of accelerated timeline represents approximately $83 million in additional revenue opportunity.
Scalability Benefits: Digital campaigns can be rapidly scaled across multiple sites and countries with minimal additional infrastructure investment. A successful campaign template can be adapted and deployed globally within weeks, compared to the months required to establish traditional recruitment networks.
Traditional vs. Digital: A Head-to-Head Comparison
Patients still trust clinicians—about 60 % prefer to hear about research from their doctor—yet only 0.2 % are actually enrolled that way. Legacy tactics struggle with limited reach, slow manual workflows and imprecise targeting.
Digital channels fix those gaps. With three-billion-plus users on Facebook alone, campaigns can pinpoint relevant demographics, interests and geographies within minutes. Meanwhile, online content encourages people to discuss opportunities with their own physicians, uniting technology and trusted medical advice rather than pitting them against each other.
Traditional Recruitment Limitations:
- Limited geographic reach constrained by site locations
- High dependency on physician referrals with inconsistent results
- Manual screening processes prone to delays and errors
- Difficulty reaching specific patient populations
- Limited ability to track and optimize recruitment performance
- High per-patient costs due to inefficient targeting
Digital Recruitment Advantages:
- Global reach with precise demographic and geographic targeting
- Automated pre-screening reduces manual workload
- Real-time performance tracking and optimization
- Multi-channel approach maximizes patient touchpoints
- Cost-effective scaling across multiple studies and sites
- Improved patient education and engagement tools
The Modern Recruiter’s Toolkit: A Guide to Digital Platforms

The landscape of clinical trial recruitment has been transformed by an array of digital tools and platforms. For us, selecting the right tools is crucial for achieving optimal clinical trial recruitment digital results. Each platform offers unique strengths and weaknesses, making a custom approach essential for every study. Let’s explore the primary digital tools currently used and their respective pros and cons.
Social Media Advertising: Reaching Patients Where They Are
Social media platforms like Facebook, Instagram, and Twitter have become indispensable in our digital recruitment toolkit. Their massive user bases offer unparalleled reach, allowing us to connect with potential participants precisely where they spend much of their online time.
- Pros:
- Best Reach: With Facebook alone boasting over 3 billion active users, the sheer volume of potential participants is enormous.
- Advanced Targeting: These platforms excel at demographic and interest-based targeting. We can pinpoint specific age groups, geographic locations, interests (e.g., support groups for certain conditions), and even behaviors, ensuring our ads reach highly relevant audiences.
- Engaging Content Formats: We can use videos, patient testimonials, interactive polls, and engaging graphics to tell compelling stories and build trust, humanizing the trial experience.
- Community Building: Social media allows for the creation of online communities where potential and current participants can find support and information.
- Cons:
- Ad Fatigue: Users can become desensitized to ads, requiring constant creativity and optimization.
- Platform Algorithms: Algorithms can be unpredictable, affecting ad visibility and cost.
- Privacy Concerns: While platforms offer targeting, navigating data privacy expectations and regulations is crucial.
- Public Perception: Some users may be wary of health-related ads on social media, necessitating a focus on transparency and credibility.
Search Engine Marketing (SEM): Capturing Patient Intent
Search Engine Marketing, primarily through platforms like Google Ads, allows us to capture the intent of individuals actively searching for health information. This is a powerful strategy because we are reaching people at the moment they are seeking answers related to their health.
- Pros:
- High Intent: People searching for health information are often highly motivated. Six in ten Americans searched for health information online in the last year, and millions of Google searches occur daily for disease-related questions. This means we’re connecting with individuals already seeking solutions.
- Keyword Targeting: We can bid on specific health-related keywords (e.g., “clinical trials for diabetes,” “symptoms of [condition]”).
- Direct Engagement: Ads can link directly to trial-specific landing pages with pre-screeners, streamlining the initial inquiry process.
- Cons:
- High Competition: Popular health keywords can be expensive due to high competition.
- Budget Waste: Without careful keyword management and negative keywords, budget can be wasted on irrelevant searches.
- Limited Specific Targeting: Unlike social media, SEM doesn’t offer as many specific demographic or interest-based targeting features beyond keyword intent.
Patient Registries and Online Health Communities
Leveraging existing patient registries and engaging with online health communities provides a highly targeted approach to recruitment. These platforms often consist of individuals already diagnosed with a specific condition and actively seeking information or support.
- Pros:
- Highly Targeted Populations: These communities are pre-segmented by condition, allowing for very precise outreach.
- Established Trust: Members often trust information shared within their community, leading to higher engagement and conversion rates.
- Direct Engagement: We can engage directly with potential participants, answer questions, and build long-term relationships.
- Cost-Effective: Once relationships are established, this can be a more cost-effective method for patient referral.
- Cons:
- Access Barriers: Gaining access or permission to engage with some private or moderated communities can be challenging.
- Smaller Scale: While highly targeted, the sheer volume of potential participants might be lower compared to mass advertising platforms.
- Ethical Considerations: Requires careful navigation to ensure community guidelines are respected and promotional efforts are transparent and non-intrusive.
[TABLE] Comparing Digital Recruitment Platforms
| Platform | Primary Strength | Targeting Capability | Typical Cost Structure | Best For |
|---|---|---|---|---|
| Social Media (e.g., FB) | Broad reach, engaging content | Demographics, interests, behaviors, lookalike audiences | Cost-per-click (CPC), Cost-per-impression (CPM) | Raising awareness, building communities, reaching niche populations with specific interests, engaging with visual and interactive content. |
| Search Engine Marketing | Capturing high intent | Keywords, geographic location | CPC | Reaching individuals actively searching for solutions, conditions, or clinical trials; capturing immediate interest. |
| Patient Registries/Communities | Highly targeted, built-in trust | Specific medical conditions, patient demographics | Fee-based access, partnership models | Recruiting for rare diseases, highly specific inclusion criteria, or when trust and direct engagement are paramount. |
Analyzing Clinical Trial Recruitment Digital Results to Overcome Core Challenges
Digital metrics illuminate—and help solve—three perennial problems: eligibility, retention and diversity.
Streamlining Eligibility and Retention
- Automated pre-screeners immediately exclude ineligible candidates, cutting manual effort and keeping sites focused on high-value contacts.
- eConsent and remote follow-ups improve comprehension and convenience, lowering the industry-wide 30 % dropout rate.
- Wearables and eDiaries collect data at home, trimming site visits and improving participant experience.
Advanced Screening Technologies
Modern digital platforms employ sophisticated screening algorithms that go far beyond simple questionnaires. These systems can:
Multi-Stage Qualification: Progressive screening that starts with basic demographic questions and gradually introduces more complex medical history inquiries. This approach maintains engagement while efficiently filtering candidates, reducing screen failure rates from industry averages of 40-60% down to 15-25%.
Natural Language Processing: AI-powered systems can analyze free-text responses to identify potential red flags or qualifying conditions that might be missed in traditional checkbox screening. For example, when a patient describes their symptoms in their own words, NLP can detect patterns that suggest eligibility for specific therapeutic areas.
Integration with Health Records: Where permitted and with proper consent, digital screening can interface with electronic health records to verify medical history, current medications, and recent lab values. This reduces the burden on patients to remember complex medical details while improving screening accuracy.
Predictive Scoring: Machine learning algorithms can assign likelihood scores to potential participants based on their screening responses, demographic data, and historical enrollment patterns. This allows recruitment teams to prioritize follow-up efforts on the most promising candidates.
A More Patient-Centric Journey
Personalised multimedia education, secure two-way messaging and telemedicine make participation easier to understand and complete—key ingredients for sustained engagement and trust.
Improved Patient Education Strategies:
Digital platforms enable sophisticated educational approaches that traditional methods cannot match:
Interactive Learning Modules: Instead of static informed consent documents, patients can engage with interactive modules that explain study procedures, potential risks and benefits, and what to expect at each visit. These modules can include videos, animations, and knowledge checks to ensure comprehension.
Personalized Communication Pathways: AI-driven systems can tailor communication frequency, timing, and content based on individual patient preferences and engagement patterns. Some patients prefer detailed scientific information, while others respond better to simple, visual explanations.
Multi-Language and Cultural Adaptation: Digital platforms can instantly provide materials in multiple languages and adapt content for different cultural contexts, removing barriers that traditionally excluded diverse populations from clinical research.
Peer Support Networks: Online communities and forums allow current and former trial participants to share experiences, provide encouragement, and answer questions from prospective participants. This peer-to-peer support significantly improves retention rates.
Retention Through Digital Engagement
Retaining participants throughout lengthy clinical trials remains one of the industry’s greatest challenges, with dropout rates averaging 30% across all therapeutic areas. Digital tools are proving instrumental in addressing this issue:
Gamification Elements: Progress tracking, achievement badges, and milestone celebrations help maintain engagement during long-term studies. Participants can visualize their contribution to medical research and feel a sense of accomplishment.
Flexible Scheduling Systems: Online portals allow participants to schedule, reschedule, and receive reminders for study visits, reducing the friction that often leads to dropouts. Automated reminder systems can send personalized messages via patients’ preferred communication channels.
Remote Monitoring Capabilities: Wearable devices and smartphone apps enable continuous data collection between visits, reducing the burden of frequent site visits while providing researchers with richer, more comprehensive data.
Real-Time Support: Chatbots and virtual assistants can provide immediate responses to common questions, while escalation protocols ensure that urgent concerns reach human staff quickly.
Driving Diversity & Inclusion
Regulators now require diversity action plans, and digital outreach is the fastest route to deliver them:
- Target ads by geography, language or cultural interest groups.
- Craft culturally relevant creatives that resonate with under-represented communities.
- Use decentralised models to reach individuals who cannot travel, whether they are rural, mobility-limited or socio-economically constrained.
COVID-19 highlighted the need: Black Americans accounted for 21 % of deaths yet only 3 % of vaccine-trial volunteers. Smart digital tactics close that gap and create study populations that reflect real-world patients.
Comprehensive Diversity Strategies
Achieving meaningful diversity requires more than just broader outreach—it demands systematic approaches that address historical barriers and build trust within underserved communities:
Community Partnership Programs: Successful diversity initiatives often involve partnerships with community health centers, faith-based organizations, and local advocacy groups. Digital platforms can facilitate these partnerships by providing co-branded materials, shared dashboards for tracking referrals, and streamlined communication channels.
Addressing Historical Mistrust: Educational content must acknowledge and address historical medical research abuses while highlighting current ethical safeguards. Transparency about study funding, oversight, and participant rights helps build trust with communities that have been historically exploited.
Economic Accessibility: Digital tools can streamline reimbursement processes, provide transportation vouchers, and connect participants with childcare resources. Mobile-friendly platforms ensure that participants without traditional computer access can still engage fully.
Cultural Competency Training: Digital platforms can deliver cultural competency training to study staff, ensuring that interactions with diverse participants are respectful and effective. This training can be customized based on the specific communities being recruited.
Language Accessibility: Beyond translation, true language accessibility involves cultural adaptation of concepts, use of appropriate health literacy levels, and availability of bilingual staff for complex discussions.
Measuring Diversity Success
Digital platforms provide unprecedented ability to track and optimize diversity efforts:
Real-Time Demographics Monitoring: Dashboards can show enrollment demographics in real-time, allowing teams to adjust outreach strategies before diversity targets are missed.
Channel Effectiveness Analysis: Teams can track which outreach channels are most effective for reaching specific demographic groups, optimizing budget allocation for maximum diversity impact.
Geographic Heat Mapping: Visual representations of enrollment patterns can identify geographic gaps in recruitment, enabling targeted campaigns in underrepresented areas.
Longitudinal Retention Tracking: Monitoring retention rates across different demographic groups helps identify and address factors that disproportionately affect certain populations.
The Future is Now: AI, Data Analytics, and Decentralized Trials

The rapid advancement of digital technologies is not just improving current recruitment methods; it’s ushering in a new era for clinical trials entirely. The integration of advanced analytics, Artificial Intelligence (AI), and the proliferation of decentralized and virtual trial models are redefining how we identify, recruit, and engage participants. These innovations are crucial for achieving optimal clinical trial recruitment digital results.
The Role of AI and Data Analytics in Precision Recruitment
Artificial Intelligence (AI) and Machine Learning (ML) are becoming indispensable in optimizing digital clinical trial recruitment, particularly in patient matching and predictive modeling. We can now process vast amounts of data to identify the most suitable candidates with unprecedented precision.
- Automated Patient Matching: AI algorithms can analyze Electronic Health Record (EHR) data, claims data, and Real-World Data (RWD) to identify potential participants who meet complex inclusion and exclusion criteria. This significantly speeds up the identification process. For example, an AI screening tool improved enrollment rates by increasing patients per screening day from 0.17 to 0.32.
- Predictive Modeling: AI can predict which recruitment channels are likely to be most effective for a specific trial, optimizing resource allocation and reducing wasted effort. This data-driven approach helps us refine our strategies in real-time.
- Improved Data Integration: Platforms like Lifebit’s federated AI platform can securely access and analyze global biomedical and multi-omic data. This allows for real-time insights and advanced AI/ML analytics, providing a powerful capability for patient matching and identifying hard-to-find patient cohorts while maintaining data privacy and security.
By leveraging AI and data analytics, we move beyond broad outreach to precision recruitment, ensuring we connect with the right patients, at the right time, with the right message.
Decentralized Trials (DCTs): Expanding Access and Redefining Participation
Decentralized and virtual trial models, enabled by digital technologies like telemedicine and wearable devices, are fundamentally impacting accessibility and participation in clinical trials. They are breaking down traditional geographical and logistical barriers.
- Increased Accessibility: DCTs allow patients to participate from the comfort of their homes, reducing the burden of travel to distant study sites. This is particularly beneficial for individuals in rural areas, those with limited mobility, or who have demanding schedules. Studies have shown that 60-85% of respondents would be more likely to participate in a trial if remote technology reduced travel.
- Remote Monitoring: Wearable devices and remote monitoring tools continuously collect vital data, reducing the need for frequent in-person visits. This provides a more comprehensive and accurate picture of a patient’s health and response to treatment.
- Telemedicine: Virtual consultations replace many in-person appointments, making it easier for patients to connect with study staff and receive medical advice.
- Electronic Patient-Reported Outcomes (ePRO): Patients can easily submit their symptoms, experiences, and quality of life data through apps or web portals, providing real-time insights.
While traditional studies recruit 13 participants per month, virtual studies can enroll an average of 51 participants per month. This not only accelerates recruitment but also broadens the demographic and geographic diversity of trial populations, leading to more representative and generalizable research findings.
Navigating the Digital Landscape: Compliance, Security, and What’s Next
Data privacy and regulatory alignment are non-negotiable when handling sensitive health records. Frameworks such as HIPAA (US) and GDPR (EU) mandate encrypted storage, audit trails and explicit consent. Lifebit’s Trusted Research Environment and Trusted Data Lakehouse deliver these safeguards by design, enabling researchers to analyse federated data without the data ever leaving its owner’s control.
Emerging Trends Changing Recruitment
- Blockchain – creates immutable, auditable data exchanges that strengthen trial integrity.
- Hyper-personalisation – AI tailors message, channel and timing to each candidate.
- Gamification – reward systems that sustain engagement through long protocols.
- Digital twins – virtual patient models that predict eligibility and refine protocol design before first contact.
Careful governance paired with innovation ensures future clinical trial recruitment digital results remain both compliant and competitive.
Conclusion: Using Digital Power for Recruitment Success
Well, we’ve certainly been on quite a journey, haven’t we? From the challenges facing clinical trials to the incredible power of digital solutions, it’s clear that the landscape of patient recruitment is being completely transformed. The clinical trial recruitment digital results we’ve seen speak volumes: more patient inquiries, quicker study timelines, and a much more efficient use of resources. Digital tools are truly empowering us to tackle those stubborn issues like finding the right patients, keeping them engaged, and ensuring our trials are wonderfully diverse.
Think back to the versatile digital toolkit we explored. Whether it’s connecting with patients on social media, capturing their intent through search engines, or engaging within trusted patient communities, these platforms allow us to meet people right where they are. This approach isn’t just about technology; it’s about making the entire clinical trial experience more patient-centric and accessible.
And the best part? The future is already here! With the incredible leaps in AI and data analytics, we’re moving towards precision recruitment, finding exactly the right patients with unprecedented accuracy. And decentralized trial models? They’re literally expanding access, allowing more people than ever to participate from the comfort of their own homes.
Of course, this exciting journey isn’t without its important considerations. Navigating the critical aspects of data privacy, security, and regulatory compliance is absolutely essential. It means we need robust technology and an unwavering commitment to ethical practices every step of the way.
The true magic lies in data analytics. It’s the engine that drives everything forward, allowing us to continuously learn, adapt, and refine our recruitment strategies for even better outcomes. By wholeheartedly embracing these digital advancements, we’re not just improving clinical trials; we’re building a future that’s faster, more efficient, more inclusive, and ultimately, far more successful in bringing life-changing treatments to patients all around the world.
To securely leverage federated data and advanced AI for optimizing your recruitment strategy, explore how platforms like Lifebit’s Real-time Evidence & Analytics Layer can provide real-time insights across global biomedical data.

