HIE Definition Guide: When Oxygen Takes a Wrong Turn

Define HIE: Essential 2025 Guide
Understanding HIE: When Your Baby’s Brain Needs More Oxygen
When you need to define HIE, you’re likely dealing with one of the most serious conditions that can affect newborns. Here’s what you need to know:
HIE stands for Hypoxic-Ischemic Encephalopathy—a type of brain injury that occurs when a baby’s brain doesn’t get enough oxygen (hypoxic) and blood flow (ischemic) before, during, or shortly after birth.
Key facts about HIE:
- Affects 1-6 out of every 1,000 births
- Can cause permanent brain damage if untreated
- Leading cause of infant mortality and lifelong disability worldwide
- Treatment with therapeutic hypothermia must begin within 6 hours of birth
HIE occurs when brain cells are starved of oxygen. While some cells recover, others die, releasing toxic substances that damage nearby healthy cells in a secondary wave of injury over hours or days.
The condition can range from mild (with potential for full recovery) to severe (causing lifelong disabilities like cerebral palsy or epilepsy). Early diagnosis and immediate treatment are critical for the best possible outcomes.
As Dr. Maria Chatzou Dunford, CEO of Lifebit, my work in biomedical data analysis has shown me how critical it is to have clear, accessible information about complex medical conditions like HIE.
Define hie vocab to learn:
What Does HIE Stand For? Unpacking the Meanings
When you’re trying to define HIE, you might be surprised to learn that these three letters mean different things depending on the context. While most people searching for this term are looking for information about the serious medical condition affecting newborns, HIE has multiple meanings.
The Archaic Verb: To “Hie”
Before HIE became a medical acronym, “hie” existed as a simple English verb meaning to go quickly or to hasten. Tracing back to Old English, this word was used frequently by writers like Shakespeare (e.g., “Hie you to church”) to mean “hurry.” While not common today, it adds a touch of literary flair. Some synonyms for hie include hasten, rush, and speed. For a complete list, check out Synonyms for hie.
The Healthcare Acronym: Health Information Exchange
In today’s digital healthcare world, HIE more commonly stands for Health Information Exchange.
This refers to the secure electronic sharing of medical data between doctors, hospitals, and other providers. This technology replaces slow, paper-based systems, allowing instant access to a patient’s history, allergies, and medications. HIE improves care quality, reduces costs, prevents duplicate tests, and avoids dangerous medication errors.
At Lifebit, our federated AI platform supports the same principles of secure data access that make HIE so valuable for patient care.
To learn more about how these systems work, read our detailed guide: What is Health Information Exchange (HIE)?. You can also explore More info about Health Data Interoperability and More info about Health Data Standardization to understand the bigger picture of healthcare data sharing.
Define HIE: A Deep Dive into Hypoxic-Ischemic Encephalopathy
Now, we arrive at the primary medical meaning of HIE: Hypoxic-Ischemic Encephalopathy. This is a severe brain injury, primarily affecting newborns, and understanding its nuances is critical for effective diagnosis and treatment.
What is the primary medical definition to define HIE?
When medical professionals define HIE, they are referring to a brain injury that occurs due to a lack of oxygen and/or blood flow to the brain. Let’s break down the term:
- Hypoxic: A reduced supply of oxygen.
- Ischemic: Restricted blood flow, which carries oxygen and nutrients.
- Encephalopathy: A broad term for brain disease or damage.
Together, Hypoxic-Ischemic Encephalopathy (HIE) is brain damage caused by a lack of oxygen and blood flow to the brain, typically around the time of birth. This is not a single event but a complex process that unfolds over time.
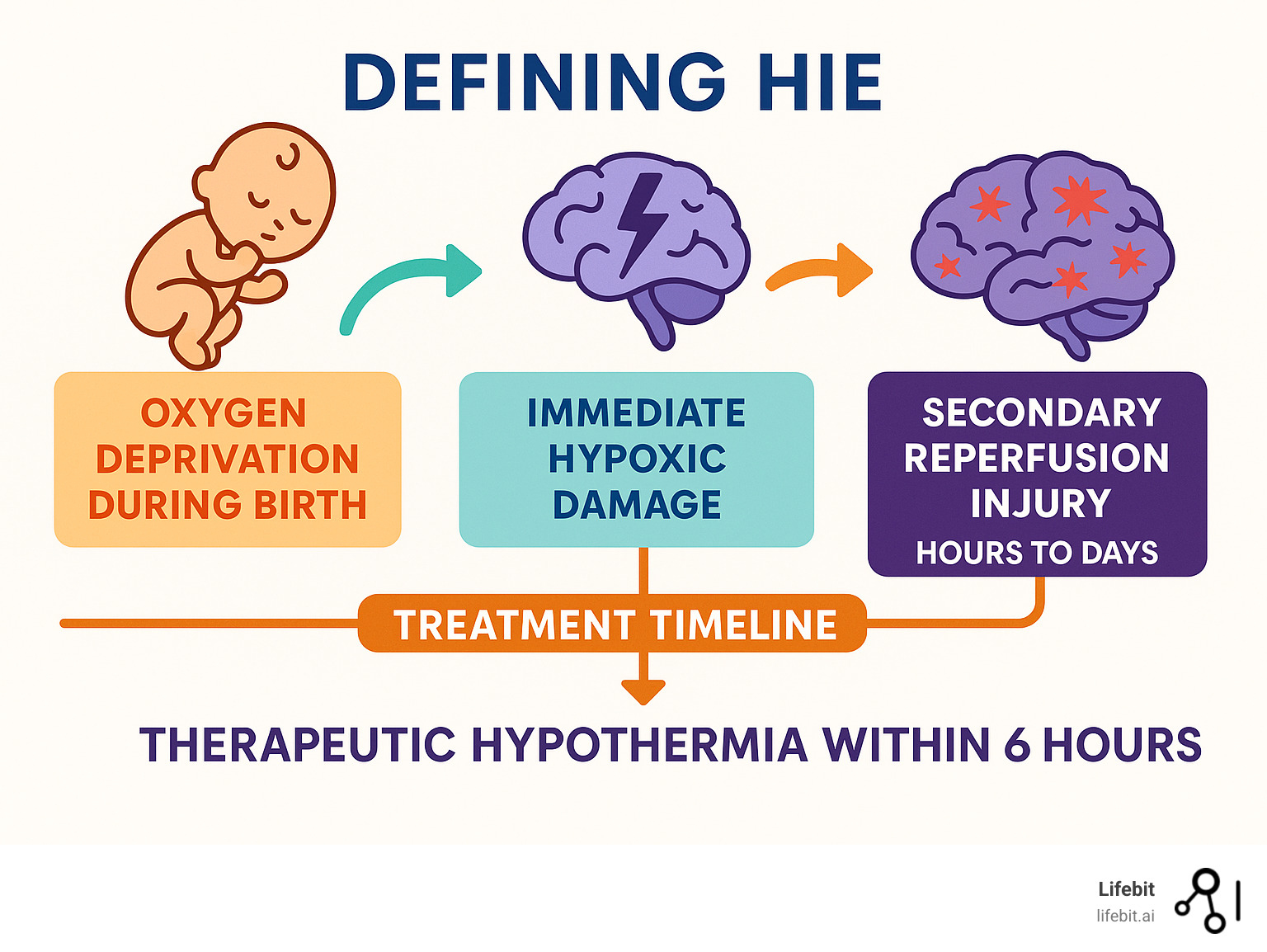
The Pathophysiology of HIE: A Two-Phase Injury
The brain damage from HIE occurs in two distinct phases, which is why the hours and days following the initial insult are so critical.
-
Primary Injury (Initial Energy Failure): This phase occurs during the oxygen and blood flow deprivation itself. Brain cells, which have extremely high energy demands, are starved of oxygen and glucose. This leads to a rapid depletion of energy stores (ATP). Without energy, cell functions fail, leading to immediate cell death (necrosis) in the most severely affected areas of the brain.
-
Secondary Injury (Reperfusion Injury): This second wave of injury begins hours to days after blood flow and oxygen are restored to the brain. While restoring circulation is essential, it paradoxically triggers a cascade of further damage. The initial injury causes dying cells to release toxic substances, including excess glutamate (an excitatory neurotransmitter) and free radicals. This leads to:
- Excitotoxicity: Excessive glutamate overstimulates healthy neighboring cells, causing them to take in too much calcium, which activates destructive enzymes and leads to their death.
- Oxidative Stress: The return of oxygen leads to the production of highly reactive molecules called free radicals, which damage cell membranes, proteins, and DNA.
- Inflammation: The brain’s immune cells are activated, causing inflammation that, while intended to clean up debris, can also damage healthy tissue.
- Apoptosis: A process of programmed cell death is initiated in cells that were damaged but not killed in the initial phase.
This secondary phase is the primary target of treatments like therapeutic hypothermia, which aims to slow down this destructive cascade and preserve as much brain function as possible. For a comprehensive overview, you can consult this Overview of HIE from Cleveland Clinic.
What Causes HIE?
HIE can result from any event that interrupts the supply of oxygen and blood to the brain. These events can occur before, during, or after birth.
-
During Pregnancy (Antenatal Causes – ~20% of cases):
- Maternal Health Issues: Conditions like severe preeclampsia (high blood pressure that can restrict blood flow to the placenta), gestational diabetes, or heart and respiratory disease in the mother.
- Placental Problems: Placental insufficiency, where the placenta doesn’t deliver enough nutrients and oxygen, or a placental abruption, where it detaches from the uterine wall prematurely.
- Maternal Infections: Severe infections like chorioamnionitis can cause an inflammatory response that affects the fetus.
- Fetal Conditions: Severe fetal anemia, a fetal stroke, or congenital malformations of the heart or brain.
-
During Labor and Delivery (Intrapartum Causes – ~50-60% of cases):
- Umbilical Cord Complications: The cord can become compressed, prolapsed (slips down before the baby), or wrapped tightly around the baby’s neck (nuchal cord), cutting off blood flow.
- Prolonged or Difficult Labor: Extremely long labor, abnormal fetal position (breech), or shoulder dystocia can lead to distress and oxygen deprivation.
- Uterine Rupture: A rare but catastrophic event where the wall of the uterus tears, often leading to severe fetal distress.
- Failure to Monitor Fetal Distress: Not recognizing or acting on signs of distress on the fetal heart monitor, such as prolonged decelerations or loss of variability.
-
After Birth (Postnatal Causes – ~10% of cases) and in Childhood:
- Severe Cardiopulmonary Disease: Conditions in the newborn like persistent pulmonary hypertension (PPHN), severe meconium aspiration syndrome, or complex congenital heart disease.
- Serious Infections: Neonatal sepsis or meningitis can lead to systemic collapse (shock) and reduced blood flow to the brain.
- Trauma or Accidents: In older infants and children, events like near-drowning, suffocation, choking, or cardiac arrest from trauma can cause HIE.
In a significant number of cases, the exact cause of HIE remains unknown, which can be incredibly difficult for families.
Signs and Symptoms of HIE
The signs of HIE in a newborn can range from subtle to severe, depending on the extent of the brain injury. Healthcare providers in the delivery room and NICU are trained to look for a specific constellation of symptoms:
- Low Apgar Scores: Apgar scores assess Appearance, Pulse, Grimace, Activity, and Respiration at 1 and 5 minutes after birth. A score below 7, and especially below 5, that persists can be an early indicator of distress.
- Breathing Problems: Apnea (pauses in breathing) or weak/absent respiratory effort, often requiring immediate resuscitation and mechanical ventilation.
- Abnormal Muscle Tone: The baby may be profoundly hypotonic (floppy, like a rag doll) or, less commonly, hypertonic (stiff and rigid).
- Poor or Absent Primitive Reflexes: Weak or absent reflexes like the Moro (startle) reflex, sucking, and grasping.
- Altered Consciousness: The infant may be lethargic, have a weak cry, be difficult to arouse, or be in a stupor or coma.
- Seizures: Seizures are a very common and significant sign of HIE. They may be obvious convulsions, but often they are subtle in newborns, presenting as repetitive facial movements (lip-smacking), eye-gazing, or pedaling/bicycling movements of the legs.
- Feeding Difficulties: A poor or uncoordinated suck-swallow-breathe reflex makes feeding difficult or impossible.
- Organ Dysfunction: The lack of oxygen can also affect other organs, leading to kidney, liver, or heart problems.
- Acidosis: High levels of acid in the umbilical cord blood (a low pH and high base deficit) provide biochemical evidence of significant oxygen deprivation during labor.
In mild cases, symptoms may be subtle, with developmental delays, learning problems, or epilepsy only becoming apparent as the child grows. For more detailed information, you can refer to More info about HIE symptoms.
Diagnosing and Treating HIE
When a baby shows signs that might indicate HIE, every minute counts. A rapid and accurate diagnosis is essential to initiate time-sensitive treatments that can profoundly alter a child’s long-term outcome.

How is HIE Diagnosed?
To define HIE accurately in each case, doctors use a combination of clinical evaluation, biochemical markers, and advanced imaging and monitoring techniques.
- Physical and Neurological Exam: This is the first step. Providers assess the newborn’s level of consciousness, muscle tone (hypotonia or hypertonia), primitive reflexes (sucking, Moro, grasp), and Apgar scores. The presence and type of seizures are also noted.
- Blood Tests: An umbilical cord blood gas analysis performed immediately after delivery is a key piece of evidence. A pH level below 7.0 or a base deficit of 12 mmol/L or more indicates significant metabolic acidosis, a hallmark of oxygen deprivation.
- Brain Wave Monitoring (EEG): An electroencephalogram (EEG) is crucial for detecting seizures. Because many neonatal seizures are subtle and not clinically obvious, continuous EEG monitoring is the gold standard. In the NICU, a simplified version called amplitude-integrated EEG (aEEG) is often used at the bedside for real-time monitoring of brain activity. It helps doctors see the background brain patterns (which can be suppressed in HIE) and identify seizure activity.
- Imaging:
- Cranial Ultrasound: This can be done quickly at the bedside to look for major abnormalities like brain bleeds or severe swelling, but it is not sensitive enough to detect the subtle tissue injury of HIE.
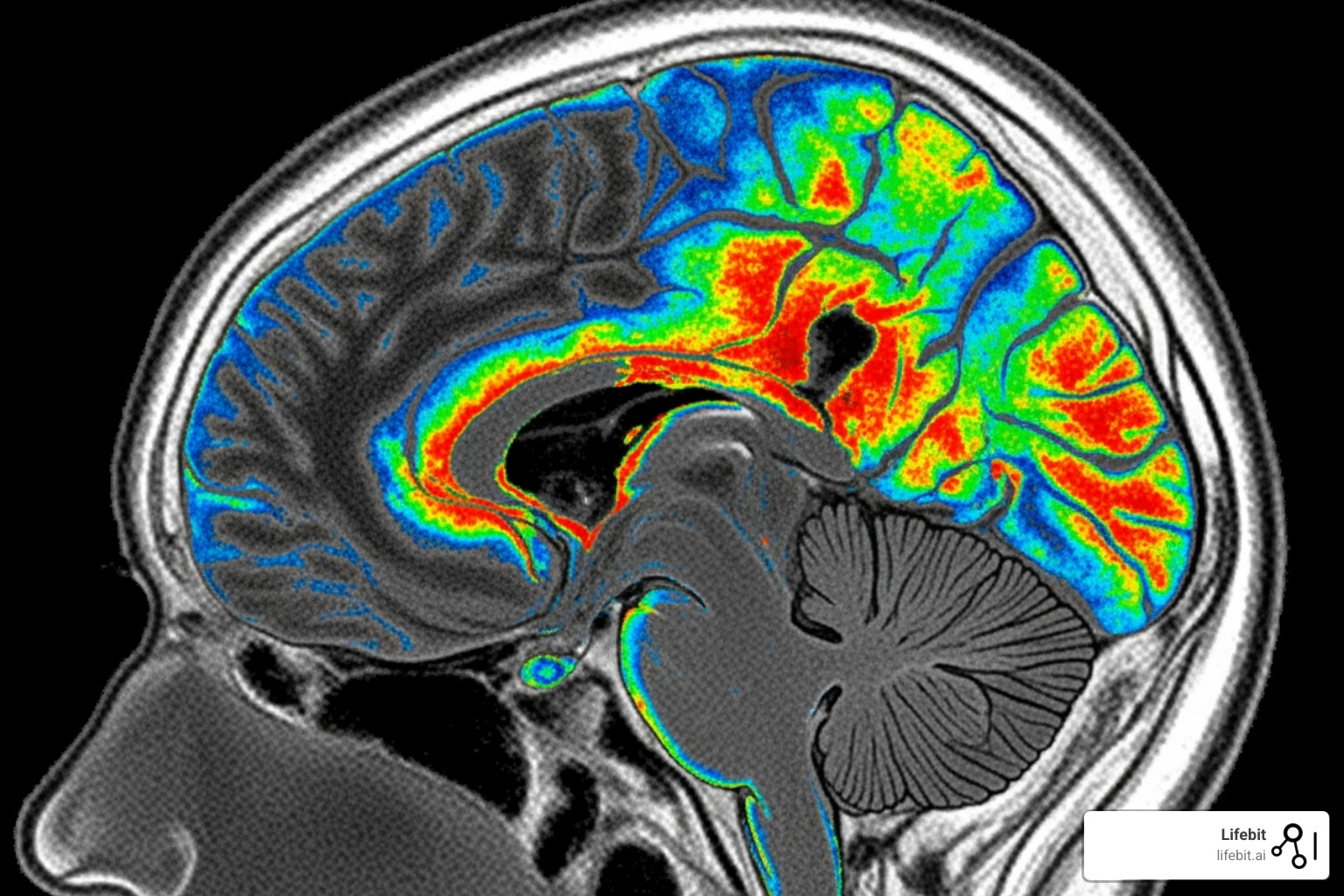
- Magnetic Resonance Imaging (MRI): An MRI is the most important imaging tool for diagnosing HIE, identifying the location and extent of brain injury. It is typically performed between 3 and 7 days of life. Specific sequences, like Diffusion-Weighted Imaging (DWI), are highly sensitive to the cytotoxic edema of the primary injury, while later scans show the full extent of the damage.
The Sarnat Scale or the Thompson Score are clinical grading systems used to classify HIE severity as mild, moderate, or severe based on the neurological exam. This classification, combined with EEG and MRI findings, helps guide treatment decisions and provides information about the likely prognosis.
What are the Treatments for HIE?
While the primary injury from oxygen deprivation is irreversible, modern treatments focus on mitigating the devastating secondary injury.
Therapeutic Hypothermia (Cooling Therapy)
This is the cornerstone of HIE treatment and one of the most significant advances in neonatal care in recent decades. It involves lowering the baby’s core body temperature to about 33.5°C (92.3°F) for 72 hours using a specialized cooling blanket or cap. This treatment is extremely time-sensitive and must begin within 6 hours of birth to be effective.
How it works: Cooling slows the brain’s metabolic rate, which reduces energy consumption and preserves remaining ATP stores. This helps to:
- Reduce the release of toxic neurotransmitters (glutamate).
- Suppress the production of damaging free radicals.
- Decrease inflammation and swelling.
- Inhibit apoptosis (programmed cell death).
By interrupting the secondary injury cascade, therapeutic hypothermia can significantly reduce the risk of death and major neurodevelopmental disability.
Comprehensive Supportive Care in the NICU
Babies with HIE are critically ill and require intensive care to support all their body systems. This includes:
- Seizure Control: Promptly identifying and treating seizures with antiseizure medications (like phenobarbital) is vital, as seizures can cause further brain injury.
- Respiratory Support: Most infants with moderate to severe HIE require a ventilator to help them breathe and to maintain optimal oxygen and carbon dioxide levels.
- Cardiovascular Management: Maintaining stable blood pressure with fluids and medications (vasopressors) is essential to ensure adequate blood flow (perfusion) to the recovering brain and other vital organs.
- Metabolic and Nutritional Support: Careful management of blood glucose, electrolytes, and fluids is critical. Since these infants cannot feed by mouth, they receive nutrition through an IV line or a feeding tube.
Rehabilitative Therapies
Long-term recovery and maximizing potential depend on early and consistent therapy, which often begins in the NICU and continues for years after discharge.
- Physical Therapy (PT): Focuses on improving muscle tone, strength, range of motion, balance, and gross motor skills like rolling, sitting, and walking.
- Occupational Therapy (OT): Helps with fine motor skills (grasping, hand-eye coordination), sensory processing, feeding skills, and activities of daily living.
- Speech-Language Pathology (SLP): Addresses feeding and swallowing problems (dysphagia) and later works on communication, language comprehension, and speech production.
Research continues to bring new hope, with ongoing studies exploring neuroprotective agents, anti-inflammatory drugs, and stem cell therapies as potential adjuncts to cooling. You can learn about the latest developments by checking Information on clinical trials for HIE.
At Lifebit, our federated AI platform helps researchers analyze data from HIE studies worldwide, accelerating the finding of new treatments while keeping patient information secure.
Living with HIE: Complications and Long-Term Outlook
For families facing an HIE diagnosis, the journey is often filled with uncertainty and hope. The long-term outlook depends heavily on the severity of the initial brain injury, the location of the damage, and the timeliness of treatment like therapeutic hypothermia.

How do doctors define HIE severity?
To define HIE severity and predict outcomes, doctors use the Sarnat Scale, which grades the encephalopathy based on a detailed neurological exam. This clinical assessment is then combined with EEG and MRI findings for a more complete picture.
- Mild HIE (Grade I): Infants are often hyper-alert, irritable, and jittery with exaggerated reflexes. They may have mild muscle tone issues but no seizures. Symptoms typically resolve within 24-48 hours, and the prognosis for normal development is excellent.
- Moderate HIE (Grade II): Infants are typically lethargic, with significantly low muscle tone (hypotonia) and suppressed reflexes. Seizures are common in this group. Outcomes are variable; while some children recover with few or no issues, many will have some degree of long-term disability. Therapeutic hypothermia is most effective for this group and can dramatically improve outcomes.
- Severe HIE (Grade III): Infants are often comatose, flaccid, and unresponsive, with absent reflexes and brainstem function. They often have persistent, hard-to-control seizures or a severely suppressed EEG. The prognosis is guarded, with a high risk of mortality or severe, lifelong disabilities for survivors.
Potential Complications and Long-Term Outcomes
The full impact of HIE often unfolds over months and years as a child grows and develops. Potential long-term complications are directly related to the areas of the brain that were damaged.
- Cerebral Palsy (CP): This is a group of permanent movement disorders and is one of the most common outcomes of moderate to severe HIE. The type of CP depends on the pattern of brain injury. For example, damage to the basal ganglia often leads to dyskinetic CP (involuntary movements), while damage to the motor cortex can cause spastic CP (stiff muscles).
- Epilepsy: A chronic seizure disorder that can develop months or years after the initial neonatal seizures. It often requires lifelong management with antiseizure medications.
- Developmental and Learning Disabilities: These can range from mild to severe. Children may face challenges with cognitive skills (e.g., memory, executive function), processing speed, and attention, which can impact academic performance.
- Sensory Impairments: Vision and hearing problems are common. A specific concern is Cortical Visual Impairment (CVI), where the eyes are structurally normal, but the brain’s visual pathways are damaged, making it difficult to interpret what is seen. Sensorineural hearing loss can also occur.
- Speech and Feeding Issues: Damage to the parts of the brain controlling the muscles of the mouth and throat can lead to ongoing feeding difficulties (dysphagia) and speech disorders like dysarthria (unclear speech).
- Behavioral and Mental Health Challenges: There is an increased risk for conditions like Attention-Deficit/Hyperactivity Disorder (ADHD), anxiety, and autism spectrum disorder (ASD) in children who have had HIE.
Despite these challenges, the brain’s remarkable ability to adapt, known as neuroplasticity, offers genuine reason for optimism. This is the brain’s capacity to reorganize itself by forming new neural connections to compensate for injury. Neuroplasticity is strongest in early childhood. Early, intensive, and consistent rehabilitative therapies (physical, occupational, speech) are not just about managing symptoms; they actively drive this rewiring process, helping the brain build new pathways to maximize a child’s function and potential.
Families can find invaluable support and resources from organizations like Hope for HIE support organization.
What is the Life Expectancy for Individuals with HIE?
Life expectancy with HIE is directly correlated with the severity of the brain injury and any associated complications.
- Mild HIE: Individuals have a normal life expectancy.
- Moderate HIE: With effective treatment and management of complications, most individuals can have a normal or near-normal life expectancy.
- Severe HIE: The prognosis is more challenging. Mortality in the newborn period can be as high as 20-50%. For survivors, life expectancy can be shortened, primarily due to the severity of associated medical issues like respiratory complications from poor muscle control, severe feeding problems requiring tube feeding, and immobility. However, with dedicated medical care and proactive management of these issues, many individuals live well into adulthood.
It’s crucial to remember that these are statistical averages. Medical care is constantly advancing, improving both quality of life and longevity for people with HIE’s long-term effects. For more detailed research on life expectancy in cerebral palsy, a condition often linked to HIE, this Study on life expectancy in cerebral palsy provides comprehensive information.
Frequently Asked Questions about HIE
It’s natural to have questions when a diagnosis of HIE enters your family’s life. Here are clear, compassionate answers to some of the most common inquiries to help you better define HIE and its implications.
How common is HIE?
HIE is a significant global health concern. It affects an estimated 1 to 6 infants out of every 1,000 live births in high-income countries. The incidence is substantially higher in low- and middle-income countries, where access to comprehensive maternal and neonatal care may be limited, with rates estimated at 10-30 per 1,000 live births.
Globally, neonatal encephalopathy, with HIE as its leading cause, is the second leading cause of infant mortality and lifelong disability. These statistics underscore why continued research into neuroprotective strategies and equitable access to treatments like therapeutic hypothermia are so vital.
Can a baby fully recover from HIE?
Yes, a full recovery from HIE is possible, but it is highly dependent on the severity of the initial injury and the promptness of treatment.
Infants with mild HIE (Sarnat Grade I) almost always recover fully with no long-term neurological issues. For babies with moderate (Grade II) and severe (Grade III) HIE, outcomes are more varied. While treatments like therapeutic hypothermia have dramatically improved survival and reduced the severity of brain damage, a significant portion of these infants may still experience long-term conditions. Studies show that among survivors of moderate to severe HIE who receive cooling, approximately 40-50% may develop conditions like cerebral palsy, epilepsy, or cognitive impairments.
Early and consistent rehabilitative therapies (physical, occupational, and speech) are critical for using the brain’s neuroplasticity and helping every child achieve their maximum potential, regardless of the initial prognosis.
Can HIE be prevented?
While not all cases of HIE are preventable, many proactive steps can significantly reduce the risk.
-
During Pregnancy: High-quality, regular prenatal care is crucial for identifying and managing maternal risk factors. This includes controlling conditions like preeclampsia and gestational diabetes, monitoring fetal growth, and avoiding harmful substances like alcohol and drugs.
-
During Labor and Delivery: Vigilant electronic fetal monitoring can detect signs of fetal distress, such as persistent late decelerations or a non-reassuring heart rate pattern. Recognizing these signs and acting promptly, which may involve an assisted delivery or an emergency C-section, can prevent or lessen the duration of oxygen deprivation.
-
In Older Children and Adults: HIE in this population often results from preventable accidents or medical emergencies. Taking safety precautions (e.g., water safety to prevent drowning), learning CPR, and managing health conditions that could lead to cardiac or respiratory arrest can help prevent HIE.
What is the difference between HIE and Cerebral Palsy?
HIE and Cerebral Palsy (CP) are related but distinct terms. HIE is the acute brain injury that happens around the time of birth due to a lack of oxygen and blood flow. It describes the event and the immediate aftermath of brain dysfunction.
Cerebral Palsy is a potential long-term outcome of HIE. CP is a broad term for a group of permanent disorders affecting movement, muscle tone, and posture. HIE is one of the leading causes of CP, but not every child with HIE will develop CP. Conversely, not all cases of CP are caused by HIE; other causes include genetic conditions, strokes, or infections.
In short: HIE is the cause (the injury), while CP is one of the possible effects (the chronic condition).
Can HIE be misdiagnosed?
Yes, in some cases, HIE can be misdiagnosed or its cause can be mistaken. The clinical signs of neonatal encephalopathy (altered consciousness, tone issues, poor feeding) are not exclusive to HIE. Other conditions can present with very similar symptoms, including:
- Metabolic Disorders: Inborn errors of metabolism can cause a buildup of toxic substances in the brain.
- Genetic Syndromes: Certain genetic conditions can cause neurological problems from birth.
- Severe Infections: Neonatal sepsis or meningitis can cause encephalopathy that mimics HIE.
- Neonatal Stroke: A stroke caused by a blood clot can also lead to brain injury and neurological symptoms.
This is why a thorough diagnostic workup—including blood tests, metabolic screening, a lumbar puncture if infection is suspected, and a brain MRI—is essential. This helps to confirm the diagnosis of HIE, rule out other conditions, and provide the most accurate information for treatment and prognosis.
Conclusion
To define HIE is to explore a term with multiple meanings, but its most critical definition is Hypoxic-Ischemic Encephalopathy—a serious brain injury in newborns caused by a lack of oxygen and blood flow.
This condition presents one of the most challenging situations a family can face, yet it is also an area of remarkable medical progress and hope. The development of therapeutic hypothermia has transformed outcomes, offering many babies the chance at a healthy life when treatment is started within the first six hours.
The journey with HIE highlights both human vulnerability and resilience. While some children recover completely, others face lifelong challenges but achieve amazing progress with dedicated therapy and support. The brain’s capacity for healing, or neuroplasticity, continues to give families reason for optimism.
At Lifebit, we are committed to advancing medical breakthroughs through data. Our federated AI platform enables researchers worldwide to collaborate securely, analyzing biomedical data to better understand conditions like HIE and develop new treatments.
The journey doesn’t end with diagnosis. Supportive communities and organizations dedicated to HIE provide invaluable resources, reminding families they are not alone. As our understanding of HIE evolves, so does our ability to prevent, treat, and support those it affects.
If you’re interested in learning how secure data sharing advances medical research, explore Lifebit’s platform for secure biomedical research and find More info about Trusted Research Environments.

