From Incentives to Innovation: Understanding Electronic Health Records Programs
Slash Errors, Cut Costs 12%: The EHR Programs Hospitals Need Now
Electronic health records programs are initiatives that help healthcare providers adopt and optimize digital patient record systems. These programs range from vendor platforms and government incentives to certification standards that enable organizations to switch from paper to secure, interoperable digital health ecosystems.
Quick Overview: What You Need to Know
- EHR Systems: Store and share comprehensive patient data across providers, unlike EMRs which are siloed to one practice.
- Four Main Types: On-premise, Application Service Provider (ASP), Software as a Service (SaaS), and Cloud-based.
- Average ROI: $86,400 per provider over five years; hospitals see 12% lower operational costs.
- Implementation Costs: Start around $32,606 per full-time physician.
- Certification: Most federal programs require ONC-certified systems and often CEHRS credentials for staff.
- Job Growth: Medical records specialist roles are projected to grow 9%, with median salaries around $48,740/year.
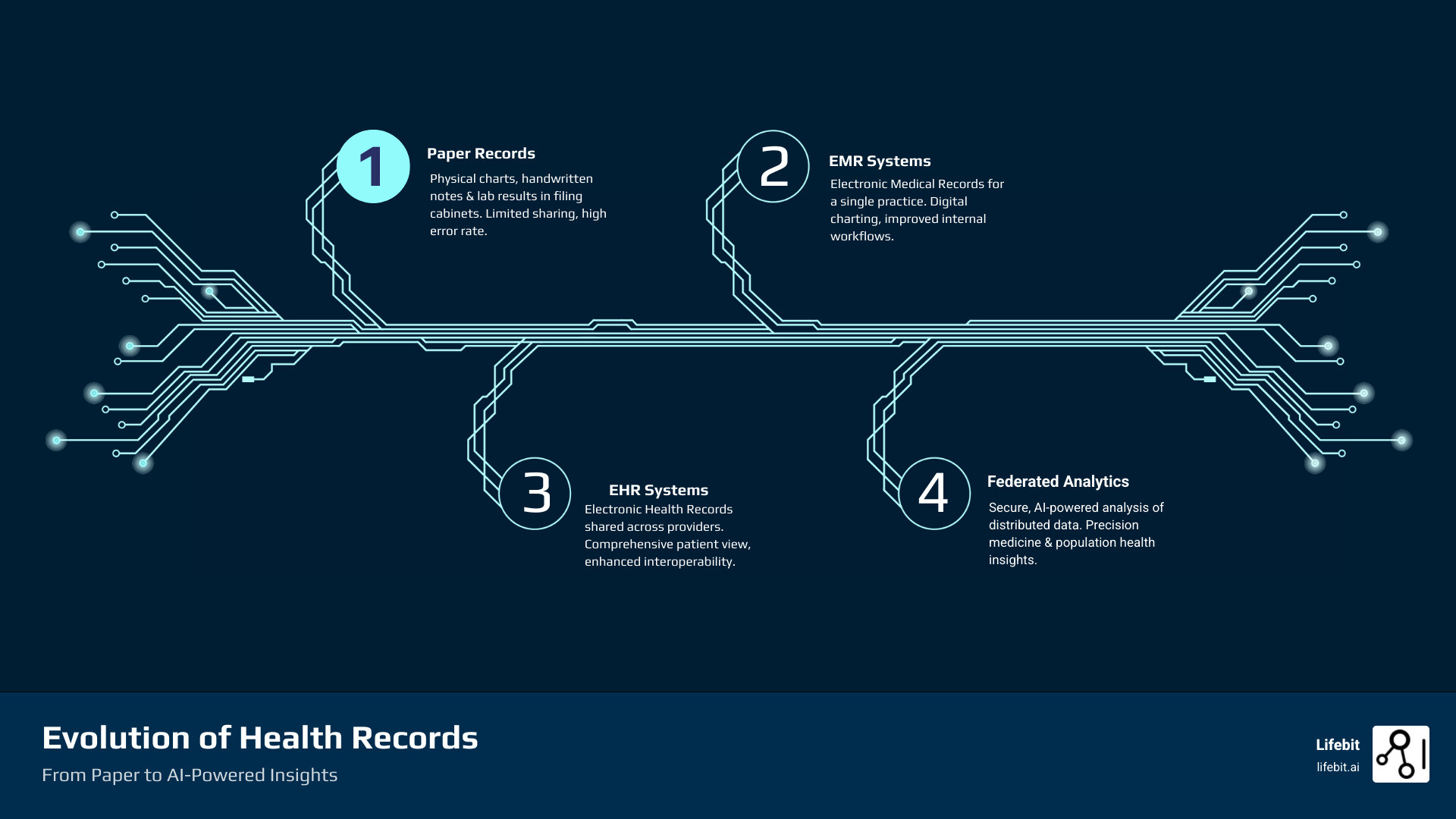
Over the past decade, healthcare has digitized. Paper charts and filing cabinets have been replaced by secure digital platforms. This shift was driven by regulatory incentives and the urgent need to reduce medical errors, which claim an estimated 250,000 lives annually in the U.S. alone.
But adoption is just the start. The modern challenge is turning siloed EHR data into actionable intelligence while maintaining security and compliance. Pharmaceutical companies need real-time pharmacovigilance; public health agencies need federated cohort analysis; regulatory bodies demand AI-powered evidence from disconnected datasets.
As someone who has spent over 15 years building secure, federated platforms for biomedical data analysis, I’ve seen electronic health records programs evolve from simple digitization projects into sophisticated data ecosystems. The real value isn’t just storing datait’s enabling secure, in-situ analytics across fragmented systems without compromising patient privacy.
EMR vs. EHR: End Data Silos and Stop Preventable Errors
At the heart of modern healthcare is the patient record, which has largely transitioned from paper to pixels thanks to electronic health records programs. This shift has fundamentally changed how healthcare is delivered and managed, moving the industry toward a more connected, efficient, and safer future.
An electronic health record (EHR) is a digital version of a patient’s chart. According to HealthIT.gov, it is a comprehensive record of health-related information that can be created, managed, and consulted by authorized clinicians and staff across more than one healthcare organization. This digital file can bring together information from current and past doctors, emergency facilities, pharmacies, labs, and imaging facilities, creating a holistic view of a patient’s health journey.
The Shift from Paper to Pixels
The transition from paper to digital was a critical step toward improving patient safety and efficiency. For decades, healthcare ran on paper charts, a system plagued by inherent flaws. Files were frequently lost or misplaced, handwriting could be illegible, and sharing information between providers was a slow, manual process involving faxes and couriers. These issues are not trivial; roughly 1.5% of U.S. medical prescriptions have dispensing mistakes, and at least one in five Americans have received prescriptions with errors, many of which are attributable to unclear or incomplete paper records.
Electronic health records programs directly address these problems. EHR software can help avoid medical errors by flagging potential drug reactions or allergies based on a patient’s complete medical history. They provide clinical decision support tools that alert providers to potential issues, ensuring that care is based on the most current and comprehensive data available. By centralizing and standardizing patient data, EHRs significantly reduce the risk of such errors, which are a leading cause of death in the United States.
The Catalyst for Change: The HITECH Act
The widespread adoption of EHRs in the U.S. was significantly accelerated by the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009. This legislation established the Meaningful Use program, which provided financial incentives to healthcare providers and hospitals for adopting and demonstrating the “meaningful use” of certified EHR technology. The program was structured in stages, encouraging providers to not only implement EHRs but also to use them to achieve specific objectives, such as improving care coordination, reducing health disparities, and engaging patients and their families. This federal push was instrumental in digitizing the American healthcare landscape.
EHR vs. EMR: It’s All About Interoperability
While the terms “EHR” and “EMR” (Electronic Medical Record) are often used interchangeably, the key difference is interoperability.
An Electronic Medical Record (EMR) is a digital version of a paper chart from a single practice. It contains a patient’s medical history from one clinician’s officeessentially a digital filing cabinet for that specific location. Its data does not easily travel outside that system, creating a digital silo.
An Electronic Health Record (EHR) is designed to be far more comprehensive. EHRs share data across different organizations, allowing a patient’s information to move with them. For example, if a patient on vacation has an emergency, the ER doctor can securely access their EHR to see their medical history, allergies, and current medications prescribed by their primary care physician hundreds of miles away. This connectivity fosters coordinated care, as everyone involved in a patient’s treatment has access to up-to-date information.
This interoperability also empowers patients by giving them secure access to their own health data through patient portals. These portals allow patients to view lab results, request prescription refills, schedule appointments, and communicate with their providers, making them active participants in their own care.
Pick the Right EHR Now: 4 System Types by Cost, Control, and Scale
When implementing electronic health records programs, selecting the right deployment model is a critical decision that shapes your budget, data control, and accessibility.
Think of it like deciding where to build a house: do you own the land and do all the work, rent space, or pay for a fully managed service? Each approach has merits depending on your organization’s size, budget, and technical capabilities. There are four main types of electronic patient records software to consider.
| EHR System Type | Upfront Cost | Maintenance Burden | Scalability | Accessibility | Data Control | IT Staff Requirement |
|---|---|---|---|---|---|---|
| On-Premise | High | High | Moderate | Limited (Local) | Full | Dedicated Internal |
| Application Service Provider (ASP) | Moderate | Moderate (Vendor) | Moderate | Remote (Private Network) | Shared (Vendor Hosts) | Vendor-Managed Hardware |
| Software as a Service (SaaS) | Low | Low (Vendor) | High | Web Browser (Internet) | Shared (Vendor Hosts) | Minimal Internal |
| Cloud-Based | Low | Low (Vendor) | Very High | Web Browser (Internet) | Shared (Vendor Hosts) | Minimal Internal |
On-Premise (Installed) Systems
With an on-premise system, you buy software licenses and install them on your own servers located within your facility. The biggest advantage is full data control, as patient records never leave your physical control. This is particularly appealing for large hospital systems with strict internal data governance policies. This model offers extensive customization, allowing you to build unique workflows and integrations tailored to your specific needs. However, it requires a high upfront cost for server hardware, networking equipment, and infrastructure, plus significant capital expenditure for software licenses. You’ll also need a dedicated internal IT staff to handle all maintenance, security patches, data backups, and complex upgrades. This includes ensuring all physical and technical safeguards required by HIPAA are met. Scaling up means buying more servers, and sharing data externally can be challenging, limiting interoperability.
Application Service Provider (ASP) Systems
The ASP model is a hybrid approach where a vendor hosts the EHR software on their private servers, and you access it remotely, typically through a dedicated, secure connection. This lowers initial costs since you aren’t buying and maintaining your own server hardware. The vendor handles server maintenance, backups, and some security tasks. However, your data is often kept in a siloed instance on the vendor’s hardware, which can limit interoperability compared to modern cloud systems. You also surrender some data control, as you are reliant on the vendor’s infrastructure and security practices. This model was a popular stepping stone from on-premise solutions but is becoming less common as true cloud-based systems offer more flexibility and scalability.
Software as a Service (SaaS) & Cloud-Based Systems
This is the direction most modern electronic health records programs are heading. Both SaaS and cloud-based EHRs are accessed via a web browser, with the vendor managing all technical infrastructure in a multi-tenant environment (where multiple organizations share the same infrastructure, with data securely segregated). The primary appeal is low upfront costs and predictable monthly subscription fees that fall under operational expenses (OpEx) rather than capital expenses (CapEx).
The vendor handles all software updates, security patches, and data backups automatically, ensuring you’re always on the latest, most secure version. Scalability is a key benefit; the system grows with your practice without requiring new hardware purchases. Because it’s web-based, your team can access records from anywhere with an internet connection, facilitating remote work and telehealth services. These systems are designed for interoperability, often using APIs (Application Programming Interfaces) to communicate seamlessly with labs, pharmacies, and other providers. Many platforms also offer marketplaces with third-party apps that add specialized functionality. The main tradeoffs are the need for a reliable internet connection and less deep customization than on-premise systems. It’s also crucial to scrutinize the vendor’s Service Level Agreement (SLA) to ensure guarantees on uptime, performance, and data security.
Prove ROI Now: EHRs Deliver $86,400 per Provider and 12% Lower Costs
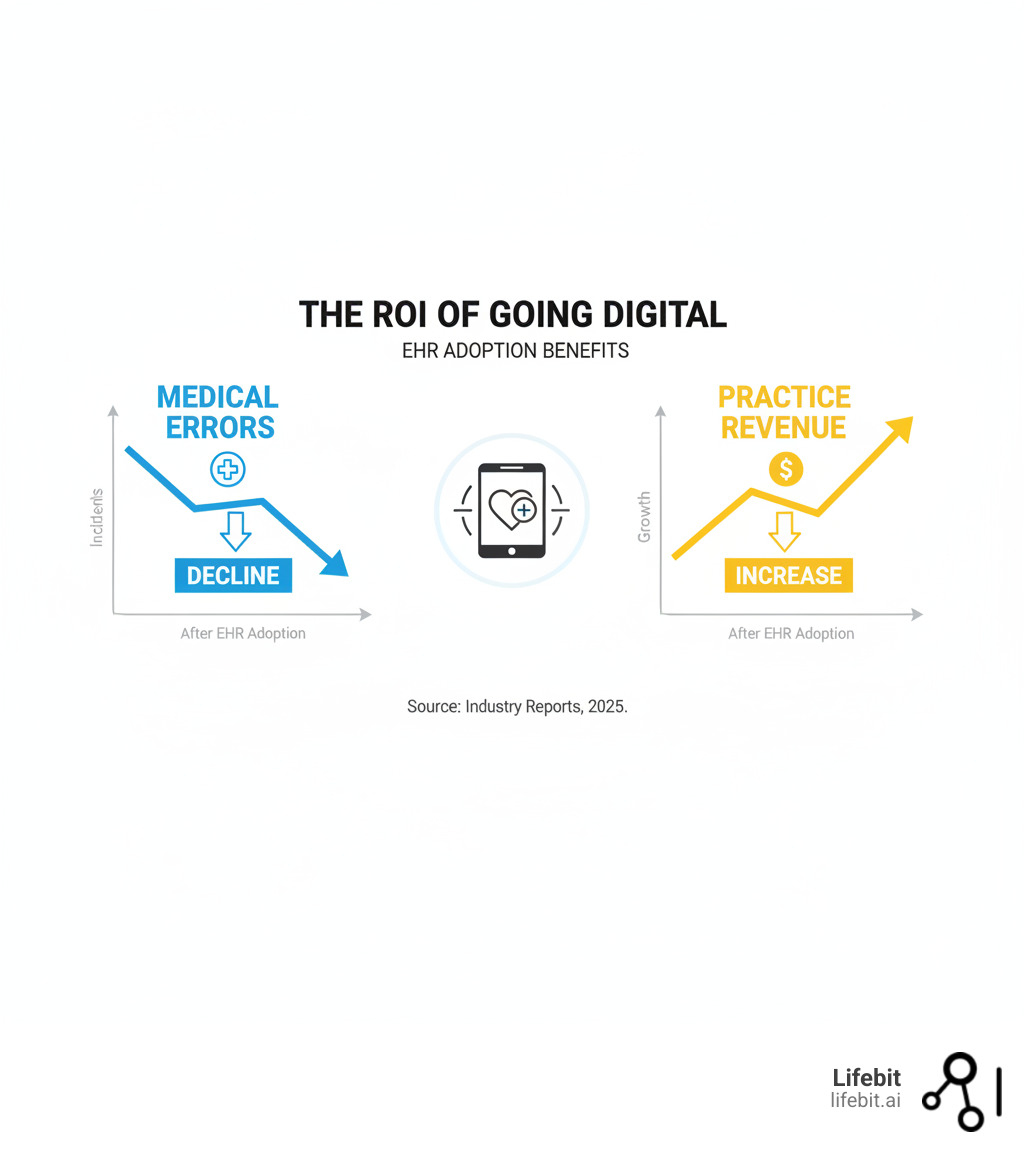
When considering electronic health records programs, organizations are making a substantial investment in better care and lower costs. The return isn’t just financial; it’s about lives saved, errors prevented, and a more efficient healthcare system. The evidence shows that when implemented correctly, EHRs deliver a powerful return on investment (ROI).
Benefits: Better Care, Lower Costs
Patient safety is the top priority. With roughly 1.5% of U.S. medical prescriptions containing dispensing mistakes, the need for a better system is clear. Electronic health records programs address this by flagging potential drug interactions, allergies, and contraindications in real-time. Clinical decision support tools embedded in EHRs provide evidence-based guidelines at the point of care, helping clinicians make more informed choices.
Studies show the impact: 78% of physicians agree that EHR adoption correlates with better patient care, and 81% report that remote chart access improves their ability to deliver it. The financial case is also strong. Hospitals with basic EHRs have 12% lower average costs. Over five years, organizations see an average ROI of $86,400 per provider. This comes from increased efficiency, reduced administrative overhead, and improved billing accuracy.
Beyond individual practices, EHRs enable population health management. By aggregating and analyzing data, organizations can identify at-risk populations, track disease outbreaks, manage chronic conditions more effectively, and shift from reactive to proactive healthcare.
Costs: Understanding the Investment
Of course, these benefits require investment. A 2005 study pegged the initial cost at $32,606 per full-time equivalent (FTE) physician, a figure that provides a baseline for understanding the scale of investment. While technology costs have evolved, this highlights that implementation is a significant financial undertaking.
Actual costs vary by system type and practice size. On-premise systems require significant hardware and software license expenses. SaaS and cloud models shift these to predictable subscription fees. Other major costs include:
- Implementation: Data migration from old systems, system customization, and workflow configuration.
- Security: Infrastructure and services to maintain robust HIPAA compliance and protect against cyber threats.
- Staff Training: A critical and often underestimated cost. Productivity is temporarily impacted during the learning curve, and 75% of physicians report wanting more training than they receive.
- Ongoing Maintenance: Whether managed internally or through a vendor, support is a continuous operational expense.
Hidden Costs and Long-Term Expenses
Beyond the initial price tag, organizations must budget for less obvious expenses. Workflow redesign is essential; simply digitizing inefficient paper processes leads to poor outcomes. This requires time and resources from clinical and administrative staff. Change management is another critical cost factor, involving communication, leadership alignment, and strategies to overcome resistance. Finally, ongoing costs can include fees for third-party integrations (e.g., connecting to a new lab), data storage upgrades, and periodic hardware refreshes for on-premise systems. Viewing these costs as a comprehensive investment in a foundation for improved patient outcomes, reduced errors, and long-term savings makes the value proposition clear.
Avoid Go-Live Chaos: Your Step-by-Step EHR Implementation Plan
Implementing new electronic health records programs is a transformative project that requires meticulous planning, careful data migration, and a strong focus on user adoption. It’s a complex undertaking that touches every part of a healthcare organization, but one that pays dividends in efficiency and patient safety when done right.

Key Factors for Choosing Electronic Health Records Programs
Choosing the right EHR system is not a one-size-fits-all decision. A thorough evaluation process is crucial. Consider these critical factors:
- Practice Size and Specialty: A small primary care clinic’s needs differ vastly from a large multi-specialty hospital’s. Look for systems with templates, workflows, and content designed for your specific field, such as cardiology, oncology, or mental health.
- Compliance and Security: The system must be fully HIPAA compliant with robust security features like end-to-end encryption, granular access controls, and detailed audit trails. A 2014 survey by TransUnion Healthcare found 65% of patients would avoid providers after a data breach, highlighting the importance of trust and security.
- Interoperability: For coordinated care, your system must communicate seamlessly with other EHRs, labs, pharmacies, and health information exchanges (HIEs). Look for support for modern standards like FHIR (Fast Healthcare Interoperability Resources) to ensure data can flow where it’s needed.
- User Experience (UX) and Physician Burnout: A clunky, poorly designed EHR is a primary driver of physician burnout. Evaluate the system’s usability from a clinician’s perspective. Is it intuitive? Does it reduce clicks and administrative burden? Involve physicians in the selection process to ensure the chosen system supports, rather than hinders, their work.
- Vendor Support and Training: Evaluate the quality and availability of the vendor’s training programs and ongoing customer support. Is support available 24/7? What is the average response time? Good support is essential, not a luxury.
- Certification: To participate in federal programs and ensure a baseline of quality, your system must be certified. The ONC Certified Health IT Product List is the official resource for finding certified EHRs that meet government-recognized standards for functionality, interoperability, and security.
Training Staff on New Electronic Health Records Programs
Even the best EHR is only as effective as the people using it. Staff training is the difference between a successful implementation and an expensive failure. One study found that 75% of physicians felt they would benefit from additional training, indicating that many organizations underestimate what’s required.
Developing a solid training plan starts with clear, role-based objectives. A physician needs different skills than a front-desk administrator or a billing specialist. Use these strategies for effective training:
- Hands-on Sessions: Use a simulated training environment or a digital adoption platform to let staff practice common workflows without impacting real patient data.
- Go-Live Support: Provide ample on-site or easily accessible remote support during the transition period. Having experts available to troubleshoot issues in real-time minimizes frustration and prevents bad habits from forming.
- Continuous Improvement: Implementation is not a one-time event. Continuously monitor system usage, gather feedback, and provide ongoing education and refresher courses. Healthcare evolves, software updates, and staff changes, so a commitment to continuous learning is essential for your electronic health records programs to remain effective.
Beyond Training: Mastering Change Management
Successful EHR adoption is as much about managing people as it is about managing technology. A formal change management strategy is crucial. This involves communicating the “why” behind the change, setting clear expectations, and getting buy-in from stakeholders at all levels. Identify and empower “super users”clinicians and staff who are enthusiastic about the new system and can act as peer-to-peer trainers and champions. By addressing the human element of the transition, you can mitigate resistance and foster a culture of adoption.
Get Hired Fast: EHR Careers Growing 9% with $48,740 Median Pay
As electronic health records programs expand and become more complex, so does the demand for skilled professionals to implement, manage, and optimize them. This field offers a diverse range of roles that ensure patient data is accurate, secure, and accessible, presenting strong and stable career opportunities at the intersection of healthcare and technology.

Job Outlook and Salary Potential
The numbers are compelling. The medical records specialist field has a projected job growth of 9% over the next decademuch faster than the average for all occupations. These professionals organize and manage health data, ensuring its quality, accuracy, accessibility, and security. According to the Bureau of Labor Statistics, the median salary for medical records and health information technicians is $48,740 per year. This provides a solid income with significant room for growth through experience and certifications.
Beyond the generalist role, the EHR ecosystem has created numerous specialized careers:
- EHR Implementation Specialist: These professionals work for healthcare organizations or consulting firms to plan, execute, and manage the transition to a new EHR system. They are project managers who handle everything from workflow analysis to staff training.
- Clinical Informatics Analyst: This role bridges the gap between clinical staff and IT. Analysts work to optimize the EHR for clinical workflows, build reports and dashboards, and ensure the system meets the needs of doctors and nurses.
- Health IT Trainer: Specializing in education, these individuals develop and deliver training programs for new and existing staff on how to use the EHR effectively and efficiently.
- EHR Compliance/Privacy Officer: Focused on security and regulation, this role ensures the organization’s use of the EHR complies with HIPAA and other privacy laws, manages security audits, and investigates potential data breaches.
Getting Certified
While formal training is required, professional certification can significantly boost your career prospects and earning potential. The Certified Electronic Health Record Specialist (CEHRS) exam, from the National Healthcareer Association (NHA), is a widely recognized credential in the field. It validates your skills in navigating EHR systems, maintaining patient confidentiality, and understanding HIPAA regulations. While not always required for entry-level jobs, certified specialists often have a better chance at getting hired and advancing their careers. Employers see the CEHRS credential as a signal of competence and commitment.
Other valuable credentials exist, depending on your career path. The Registered Health Information Technician (RHIT) certification from AHIMA is a broader credential covering health data management. For those looking to specialize, certifications from major EHR vendors like Epic or Cerner are highly sought after and can lead to high-paying consulting and analyst roles. The path to certification typically involves completing a training program, gaining hands-on experience, and passing the exam. It’s an achievable goal that can open doors to a stable, growing career in healthcare.
Stop Wasting EHR Data: How Federated AI Turns Silos into Real-Time Insights
Electronic health records programs are now the backbone of modern healthcare. High adoption rates in countries like the UK (97%) and the Netherlands (98%) show that digital records are essential. But collecting this data was just the beginning. The true value of this massive digital transformation is not in the data itself, but in the insights we can derive from it.
The real challenge isn’t storing more informationit’s making that information work. We need to predict disease outbreaks, optimize treatments, and make public health proactive. The data exists in disconnected silos across hospitals, clinics, and research centers. How do we analyze it securely, at scale, without compromising patient privacy?
Traditional methods of data sharing are slow, risky, and often inadequate. They involve complex data use agreements, painstaking and often imperfect data anonymization processes, and the physical transfer of massive datasets, which introduces security risks and high costs. Standards like FHIR have improved how EHRs talk to each other for individual patient care, but they weren’t designed for complex, large-scale analytics across populations.
The next frontier is enabling secure, in-situ analytics across fragmented systems without moving sensitive patient data. This approach, known as federated learning or federated analytics, works by sending the analysis (the algorithm) to the data, rather than the other way around. Imagine sending a chef (the algorithm) to cook in multiple, separate kitchens (hospitals) using only their local ingredients (patient data), and then combining the final recipes (the insights) centrally. The raw ingredients never leave their kitchen.
This is the future that platforms like Lifebit’s are building. By providing federated AI technology, organizations can analyze sensitive health data where it resides, turning isolated data silos into a collaborative intelligence network. This allows pharmaceutical companies to conduct real-time pharmacovigilance across millions of patient records to detect safety signals faster. It enables public health agencies to perform cohort analysis for pandemic modeling without data transfer headaches. Researchers can leverage global biomedical data to identify cohorts for rare diseases, all while upholding the highest privacy and security standards.
The journey from paper to digital was transformative. But the journey from data collection to actionable intelligenceinsights that save lives and accelerate researchis the revolution happening now.
Ready to open up the full potential of your health data? Learn more about Lifebit and find how federated AI can transform your organization’s approach to healthcare analytics.

