Detailed Guide to Health Data Integration Process

Why Health Data Integration is the Backbone of Modern Healthcare
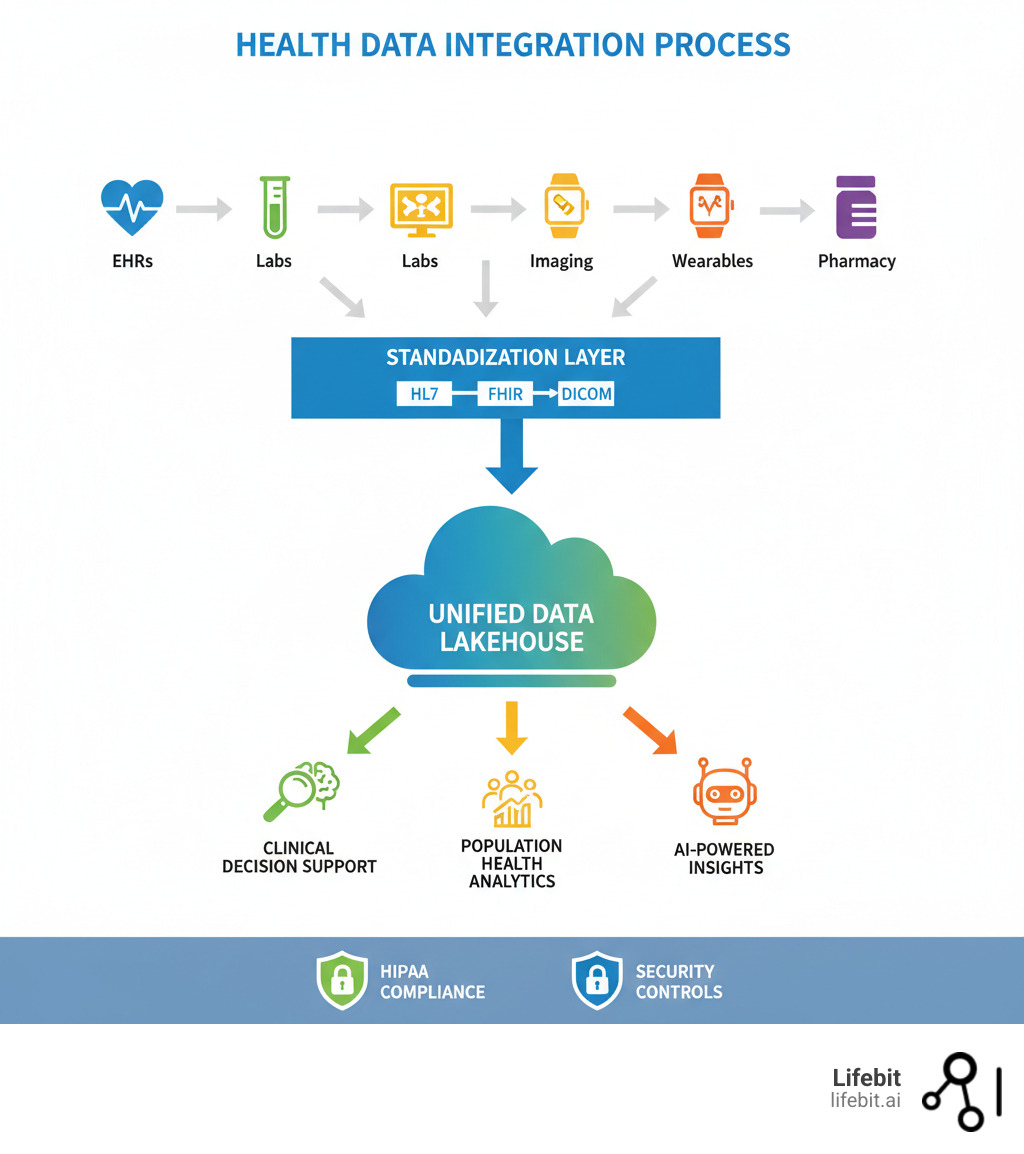
Health data integration is the process of consolidating patient information from multiple, disconnected systems—electronic health records (EHRs), lab results, imaging systems, and pharmacy databases—into a single, unified view. It ensures that when a doctor sees a patient, they have a complete health story, not just scattered fragments.
Healthcare generates 30% of the world’s data, yet most of it remains trapped in silos. A single hospital can use up to 18 different EHR platforms, forcing clinicians to spend nearly an hour a day manually reconciling data. This inefficiency costs the industry billions and increases the risk of medical errors.
Effective integration yields clear results. Hospitals with integrated data have reduced duplicate testing by 34% and cut 30-day readmission rates from 18.7% to 12.3%. This isn’t just a technical problem—it’s a patient safety imperative. In 2023, data breaches affected over 112 million individuals, highlighting the need for secure, seamless data exchange.
As Dr. Maria Chatzou Dunford, CEO of Lifebit with over 15 years in computational biology, I’ve seen how secure health data integration transforms drug findy and precision medicine. This guide will walk you through how modern organizations are building truly connected healthcare systems.
Why Health Data Integration is No Longer Optional
Healthcare data has exploded, growing from 153 exabytes in 2013 to 2,314 exabytes in 2020. But more data doesn’t automatically mean better care. Without effective health data integration, this information remains trapped in disconnected silos, preventing a complete view of a patient’s health.
Integration has shifted from a “nice-to-have” to a necessity, forming the foundation for improved patient outcomes, informed clinical decision-making, and streamlined operational efficiency. It’s also critical for the success of value-based care models, which reward providers for patient outcomes rather than service volume. This data-driven approach requires a complete picture to identify at-risk populations and implement proactive interventions.
When data flows seamlessly, the results are measurable. Patients in value-based care programs experience 9.4% fewer ER visits and 13% lower use of ERs for non-emergent care, leading to significant cost savings. Recognizing this, governments are pushing for a patient-centric, connected health system.
For providers, a unified patient view eliminates hours spent hunting for information, reducing the administrative burden. This leads to faster diagnoses and more personalized treatment plans. For patients, it means fewer repeated tests, better-coordinated care, and a healthcare journey where everyone on their care team is working from the same playbook.
Top 3 Challenges Hindering a Unified Health View
Achieving a unified view of health data is a significant challenge. The reality is that health data integration faces three fundamental roadblocks that every healthcare organization must steer.

First, the lack of data standardization makes it difficult to make sense of information recorded in countless different formats. A single health system might juggle 18 different EHR platforms, each with its own data structure.
Second, strict privacy regulations like HIPAA demand rigorous compliance to protect sensitive patient information. With data breaches affecting over 112 million individuals in 2023 alone, the stakes are incredibly high.
Third, implementation costs can be substantial, requiring significant financial investment in technology, infrastructure, and specialized talent.
Understanding these challenges is the first step toward solving them. In the sections that follow, we’ll explore practical strategies that organizations are using to overcome these obstacles on their health data integration journey.
1. Lack of Standardization and Interoperability
The most significant obstacle to effective health data integration is the lack of standardization. Data silos—isolated repositories of information—are rampant in healthcare, arising from disparate EHR systems, proprietary software from medical device manufacturers, and specialized departmental systems. This fragmentation traps patient information, preventing it from flowing where it’s needed most and creating a dangerously incomplete clinical picture.
A single healthcare system can operate up to 18 different EHR platforms, each storing similar data in different ways. This lack of consistency makes it nearly impossible to piece together a complete patient history. For example, a patient’s allergy to penicillin might be clearly flagged in their primary care physician’s EHR but be recorded as free-text in a hospital’s admission note, making it invisible to automated safety alerts.
This brings us to the core problem: a lack of interoperability, the ability of different systems to access, exchange, and use data cooperatively. Experts often describe interoperability in four levels:
- Foundational interoperability: Establishes the basic connectivity for one system to send and receive data from another. It doesn’t require the receiving system to be able to interpret the data.
- Syntactic interoperability: The ability to exchange data in a structured format that different systems can read. It ensures the message format is consistent, like agreeing on the grammar of a sentence.
- Semantic interoperability: The deeper challenge. It ensures that the exchanged data is interpreted with the same meaning by all systems. For example, one system might record a “heart attack” while another uses the ICD-10 code “I21.9.” Without semantic interoperability, which requires standardized coding systems like SNOMED CT for clinical terms and LOINC for lab tests, systems can’t recognize they are referring to the same condition.
- Organizational interoperability: Includes the governance, policy, and legal frameworks that allow data to be shared across different organizations. Even with perfect technical interoperability, data sharing fails without trust and clear data use agreements.
This inconsistency in formats, terminology, and governance makes creating a holistic patient view incredibly difficult. Until these fundamental standardization issues are addressed, true health data integration remains a major challenge.
2. Navigating Security and Privacy Regulations
Healthcare data contains our most sensitive personal information, and protecting it is paramount. When we talk about health data integration, we’re handling the stories of people’s lives, which demands the highest level of security and an unwavering commitment to privacy.
Regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the US, GDPR in Europe, and PIPEDA in Canada set the legal framework for protecting patient information. In the US, HIPAA is divided into the Privacy Rule, which governs how Protected Health Information (PHI) can be used and disclosed, and the Security Rule, which mandates specific administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of electronic PHI. Compliance isn’t just a legal checkbox—it’s a trust contract with patients.
Managing patient consent for data sharing across multiple systems is a complex but essential requirement. Organizations must navigate “opt-in” versus “opt-out” models and provide patients with granular control over how their data is used—for example, allowing its use for direct clinical care but not for secondary research purposes. This requires sophisticated consent management technology built directly into the integration architecture.
The risk of data breaches is a stark reality. In 2023, over 540 healthcare organizations reported breaches affecting more than 112 million individuals. While data integration creates a more complete health picture, it also consolidates data, making it a more valuable target for attackers.
To mitigate this, techniques like de-identification are essential for research and analytics. HIPAA outlines two primary methods: the Safe Harbor method, which involves removing 18 specific types of identifiers, and the Expert Determination method, where a statistician certifies that the risk of re-identification is very small. These methods, along with pseudonymization (replacing direct identifiers with artificial codes), allow for data analysis while minimizing privacy risks.
The challenge is to architect systems that deliver both data access and privacy. At Lifebit, our federated platform is built to resolve this tension. Our Trusted Research Environment (TRE) allows analysis of sensitive data without moving it from its secure source, dramatically reducing breach risk while enabling the powerful analytics that health data integration promises.
3. Managing Cost and Complexity
Building a robust health data integration infrastructure is both expensive and complex, requiring sustained investment in technology and people. Organizations often spend millions annually on interoperability initiatives, not including hidden costs like staff training and workflow redesign.
A major hurdle is the prevalence of legacy systems, some decades old, that were never designed for modern data exchange. Integrating or replacing these systems is a massive undertaking, often taking years and costing millions per upgrade.
Furthermore, effective health data integration requires a specialized workforce with skills in data engineering, healthcare security, and clinical informatics. This talent is both expensive and in high demand.
The work doesn’t end at launch. Integration solutions require ongoing maintenance to keep pace with evolving standards (like the shift to FHIR), new technologies, and changing regulations. The architecture must also be designed for scalability to handle the exponential growth of healthcare data without performance degradation.
For smaller organizations with limited IT resources, these combined challenges can feel impossible. Yet the cost of not integrating—in terms of medical errors, inefficiencies, and missed opportunities for better outcomes—is often even higher.
The Technology Powering Modern Health Data Integration
Modern health data integration relies on a sophisticated stack of standards, APIs, and cloud platforms to move medical information safely and efficiently. While traditional data integration methods like Extract, Transform, Load (ETL) still have a role, the industry is shifting toward the real-time capabilities offered by APIs and cloud-native architectures.

Key Data Exchange Standards
Data exchange standards provide the common language necessary for different healthcare systems to communicate.
| Standard | Primary Use | Data Format | Flexibility |
|---|---|---|---|
| HL7 (Health Level Seven) | Messaging for clinical and administrative data | Text-based, XML | Lower (older versions) |
| DICOM (Digital Imaging and Communications in Medicine) | Storage and transmission of medical images | Binary | Specific to imaging |
| FHIR (Fast Healthcare Interoperability Resources) | Modern, web-based exchange of clinical data | JSON, XML | High (API-driven) |
HL7 v2 has long been the workhorse for messaging, but its rigid, pipe-delimited format often requires custom, point-to-point interfaces that are brittle and difficult to maintain. DICOM is the universal standard for medical imaging, ensuring diagnostic quality is maintained across devices. The game-changer is the modern FHIR standard, which uses modern web technologies and RESTful APIs. Its modular, resource-based structure (e.g., Patient, Observation, Encounter) makes it far easier for developers to implement and is quickly becoming the global standard for interoperability, driven by regulations like the 21st Century Cures Act in the US.
The Role of Cloud Architecture and APIs
Cloud-native platforms have transformed health data integration. They enable real-time data exchange from wearables and clinical systems, providing immediate insights. The scalability and flexibility of the cloud mean infrastructure can adapt to any data volume, from a small clinic to a national health system. This shift has also popularized ELT (Extract, Load, Transform), where raw data is loaded into a cloud data lake or lakehouse before being transformed, providing greater flexibility for data scientists. Platform-as-a-Service (PaaS) offerings make sophisticated tools accessible, while RESTful APIs and microservices architectures create lightweight, resilient, and maintainable systems that are easier to update and scale than monolithic applications.
Centralizing Data: From Warehouses to Lakehouses
Once data is flowing, it needs a home. Data warehouses are highly structured for business intelligence but struggle with the variety of modern healthcare data, especially unstructured data like physician notes or genomic sequences. Data lakes can store any data type but often lack the governance and performance to prevent them from becoming unusable “data swamps.”
The data lakehouse concept offers the best of both worlds. It combines the low-cost, flexible storage of a data lake with the ACID transactions, data governance, and performance optimization features of a data warehouse. This makes diverse data types—from structured claims data to unstructured clinical notes and multi-omic data (genomic, proteomic, etc.)—analytics-ready in a single platform. This architecture is especially powerful for training AI/ML models, which require access to massive, varied datasets. At Lifebit, our Trusted Data Lakehouse (TDL) leverages this approach to create a unified, secure environment for biomedical research, supporting everything from simple SQL queries to advanced AI.
A 5-Step Roadmap for Effective Health Data Integration
Starting on a health data integration project requires a clear roadmap. With strategic planning, solid governance, and built-in security, you can build an integrated system that is both scalable and sustainable.
Step 1: Define Clear Objectives and Governance
Before you begin, answer the critical question: why are we doing this? Establish specific, measurable goals, such as reducing duplicate testing or improving patient safety. Catalog all data sources (EHRs, labs, imaging) and form a data governance committee with clinical, IT, and legal stakeholders. This group will define data ownership, set quality metrics, and create the rules for how data is acquired, stored, and used.
Step 2: Prioritize Data Standardization and Quality
To manage the messy reality of healthcare data, adopt a common standard like FHIR to act as a universal translator. Perform detailed data mapping to ensure concepts like “heart attack” and “myocardial infarction” are recognized as the same event. Use standardized terminologies like SNOMED CT for clinical concepts and LOINC for lab observations to ensure true semantic interoperability. Finally, implement data cleansing and validation rules to remove duplicates, correct errors, and flag questionable data before it enters the integrated system.
Step 3: Ensure Accurate Patient Identity Management
A critical challenge is ensuring that “John Smith” in the EHR is the same person as “J. Smith” in the lab system. The solution is a robust Master Patient Index (MPI), which serves as a single source of truth for patient identity. The MPI uses sophisticated record linkage algorithms to analyze data points and determine if multiple records belong to the same person. Proven strategies exist for consolidating patient data from legacy systems into unified records. This prevents duplicate records that lead to fragmented care, medical errors, and repeated tests.
Step 4: Implement Robust Security and Compliance
With data breaches on the rise, security must be a foundational requirement. Adopt a security-by-design approach, thinking about threats and protections from the very first planning meeting. Use end-to-end encryption for data both in transit and at rest. Implement strict role-based access controls based on the principle of least privilege, ensuring users can only access the data they need to do their job. Maintain comprehensive audit trails to log all data access and conduct regular HIPAA risk assessments to identify and remediate vulnerabilities.
Step 5: Leverage Analytics and Measure ROI
Health data integration is the foundation; the real value comes from what you do with the unified data. Deploy advanced analytics tools and create intuitive business intelligence dashboards to surface insights for clinicians, administrators, and researchers. Track key performance indicators (KPIs) that tie directly back to the goals you defined in Step 1, such as readmission rates or time-to-diagnosis. Most importantly, demonstrate the clinical and financial impact of your efforts to prove the ROI of your integration project.
The Future is Federated: AI, Analytics, and What’s Next
We are moving beyond simply connecting systems to asking, “what can we find when we do?” The future of health data integration is about intelligent, privacy-preserving collaboration. This next frontier is defined by three interconnected trends: the application of AI and predictive analytics, the rise of federated learning, and the growing importance of Real-World Evidence.
The Impact of AI and Advanced Analytics on health data integration
Artificial intelligence is changing what’s possible with integrated health data. AI-driven insights uncover complex patterns in massive datasets that can reveal early warning signs of disease or explain why patients respond differently to treatments. For example, an AI model could analyze real-time data from an ICU—integrating vital signs, lab results, and medication orders—to predict the onset of sepsis hours before human clinicians can detect it, triggering life-saving alerts. Predictive modeling can also identify individuals at high risk for chronic conditions, enabling proactive interventions. This is making personalized medicine a reality, where treatments are tailored to a person’s unique biology and lifestyle. AI also helps by automating clinical workflows and using Natural Language Processing (NLP) to extract structured information from unstructured data like clinical notes.
The Rise of Federated Learning for Privacy-Preserving Insights
The greatest insights come from analyzing data across many institutions, but privacy regulations and data ownership concerns make this difficult. Federated learning offers a groundbreaking solution: instead of moving sensitive data to a central location, the AI model travels to the data. The process works as follows:
- A central server distributes a base machine learning model to multiple data partners (e.g., hospitals).
- Each partner trains the model on its own local, private data behind its firewall.
- Instead of sharing the raw data, each partner sends back only the updated model parameters (aggregated, anonymized learnings).
- The central server aggregates these updates to create an improved global model.
This enables unprecedented cross-institutional collaboration, allowing organizations worldwide to train powerful AI models on their combined data without ever sharing patient records. It overcomes legal, ethical, and security barriers to data sharing by keeping data where it belongs while still enabling collective intelligence.
Real-World Data and Evidence (RWD/RWE)
Integrated health data is the engine for generating Real-World Evidence (RWE) from Real-World Data (RWD)—data collected outside of traditional clinical trials, such as from EHRs, claims data, and patient registries. RWE provides critical insights into how treatments perform in diverse, everyday clinical settings. Regulators like the FDA are increasingly accepting RWE to support new drug approvals and monitor post-market safety. Effective health data integration is the essential first step to creating the high-quality, large-scale RWD datasets needed to generate reliable RWE.
At Lifebit, our platform is built on this federated approach. Our federated data platform enables secure, real-time insights across distributed health data ecosystems, making large-scale research, RWE generation, and pharmacovigilance possible in a way that traditional centralized methods cannot support.
Frequently Asked Questions about Health Data Integration
Here are answers to some of the most common questions about health data integration.
What is the main goal of health data integration?
The primary goal is to consolidate health information from diverse sources (EHRs, labs, wearables) into a single, comprehensive view. This unified narrative enables better care coordination, sharper clinical decision-making, and improved operational efficiency. It also provides the foundation for advanced analytics that can lead to better patient outcomes.
How does health data integration enable interoperability?
Integration is the foundational work that makes interoperability possible. By standardizing data formats, cleaning inconsistencies, and centralizing information using technologies like FHIR and APIs, integration creates a common ground. This allows different applications and providers to seamlessly and securely exchange and interpret data, moving beyond simple connection to true understanding.
What is the difference between HL7 and FHIR?
HL7 v2 is an older, widely used standard for pushing messages between systems (e.g., lab orders). It uses a rigid, text-based format. FHIR (Fast Healthcare Interoperability Resources) is a modern standard built for the web. It uses flexible, developer-friendly APIs (REST) and a resource-based data model, making it ideal for real-time data access across web and mobile applications. FHIR is rapidly becoming the global backbone for modern interoperability.
Conclusion: Building a Healthier Future, One Connection at a Time
We have reached a pivotal moment where the shift from fragmented data to integrated intelligence is reimagining healthcare. Health data integration transforms isolated information into actionable insights that save lives, reduce costs, and accelerate medical breakthroughs. The journey is complex, but the results are clear: organizations are seeing dramatic improvements in diagnostic accuracy and treatment delays.
This change allows providers to intervene proactively, personalize treatments, and coordinate care seamlessly. Researchers can find new therapies, and public health agencies can respond faster to threats. Success demands a strategic approach that accepts modern standards like FHIR, leverages cloud architectures, and adopts privacy-preserving technologies like federated learning.
At Lifebit, we are building this future. Our next-generation federated AI platform enables secure, real-time access to global biomedical and multi-omic data. With built-in capabilities for harmonization, advanced AI/ML analytics, and federated governance, we empower biopharma and governments to conduct large-scale, compliant research. Our platform’s components—including the Trusted Research Environment (TRE) and Trusted Data Lakehouse (TDL)—deliver real-time insights and secure collaboration across distributed data ecosystems.
The future of healthcare is connected. Every system integrated and every insight shared brings us closer to a world where the right information reaches the right person at the right moment. That is the promise of health data integration.
Explore Lifebit’s federated data platform for secure, real-time insights

