Machine Learning Clinical Data: From Records to Results

Why Machine Learning Clinical Data is Changing Healthcare Outcomes
Machine learning clinical data is revolutionizing how healthcare organizations predict patient outcomes, accelerate drug findy, and improve diagnostic accuracy. Here’s what you need to know:
Key Applications:
- Diagnosis – Deep learning achieves 87% sensitivity and 92% specificity in distinguishing COVID-19 from other lung diseases
- Drug Findy – Only 12% of drug programs succeed from phase 1 to launch; ML helps identify promising candidates faster
- Clinical Trials – NLP systems improve patient recruitment by 80% by matching thousands of eligibility criteria in under 16 seconds
- Cost Reduction – Automated systems achieve diagnostic accuracy with AUCs of 0.98 in lab tests, reducing operational waste
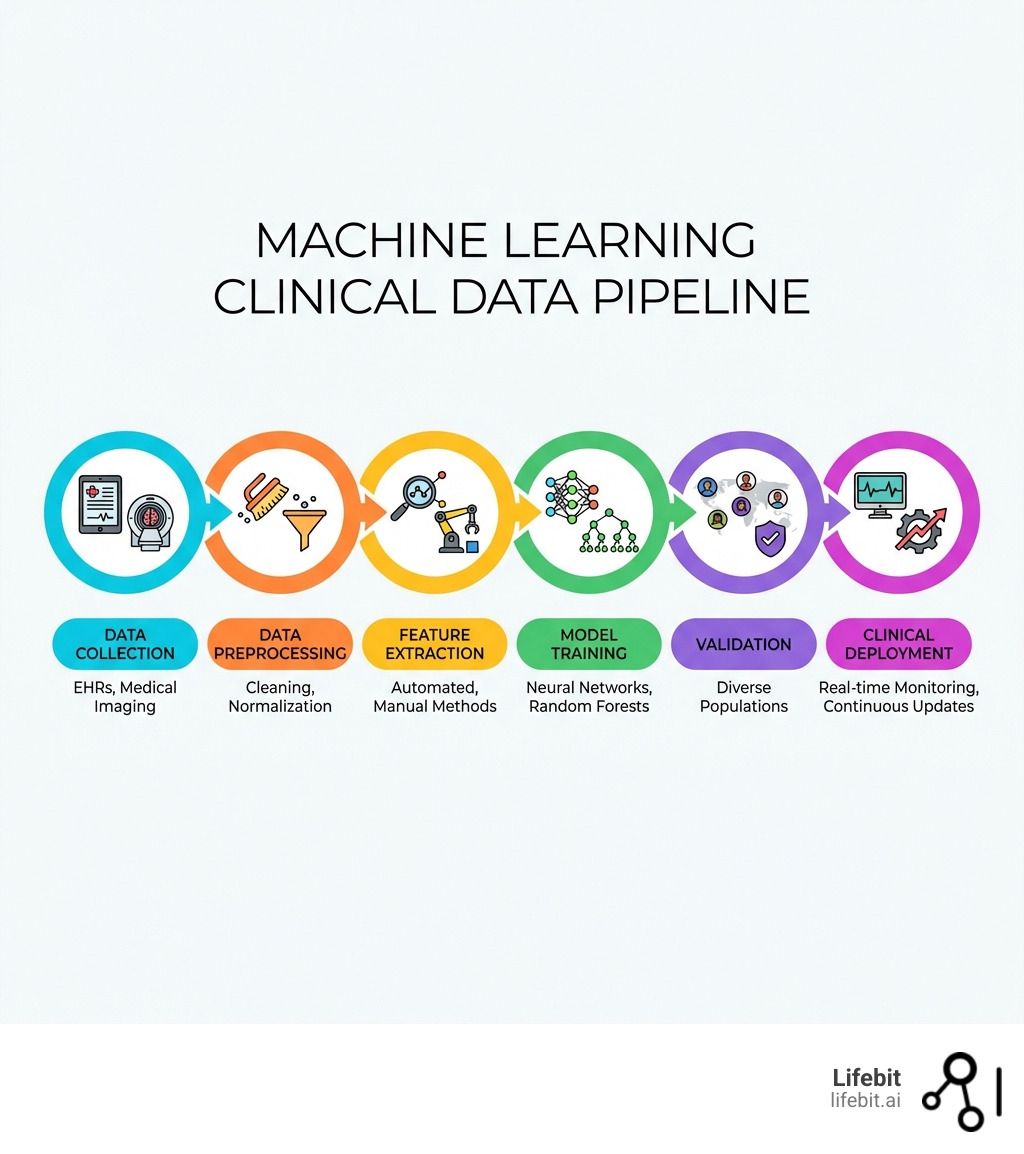
The challenge? The pipeline from AI concept to clinical deployment is long and complicated. Most healthcare organizations struggle with three core problems:
- Data silos – Patient records are scattered across incompatible systems
- Integration barriers – Models fail when they can’t fit into real clinical workflows
- Quality issues – Insufficient or poorly labeled data leads to unreliable predictions
Deep learning models can automatically learn patterns from raw data without manual feature extraction. This makes them ideal for complex tasks like analyzing medical imaging, genomics, and unstructured electronic health records (EHRs). But AI does not free you from good statistical practice – it actually makes study design more important because it’s easy to mislead yourself.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit, where I’ve spent over 15 years building federated genomics platforms that enable secure, compliant analysis of machine learning clinical data across global biobanks and pharmaceutical organizations. Our work powers evidence generation from over 275 million patient records without moving sensitive data.
Key Machine learning clinical data vocabulary:
Machine Learning vs. Deep Learning: What Matters for Clinical Data
When we talk about machine learning clinical data, it is vital to distinguish between traditional machine learning (ML) and its more advanced cousin, deep learning (DL). In the clinical world, this distinction isn’t just academic—it determines how much manual labor your team has to perform.
Traditional machine learning involves a statistical approach to reasoning where human experts usually have to specify “features” (like a patient’s age, blood pressure, or a specific tumor diameter) before the algorithm can make a prediction. Deep learning, however, uses multi-layered artificial neural networks to model complex patterns. It mimics the brain’s synaptic connections by reinforcing or pruning artificial neurons based on data patterns.
According to Scientific research on deep learning foundations, the primary advantage of DL is its ability to handle high-dimensional data where the relevant features are difficult for humans to specify.
| Feature | Traditional Machine Learning | Deep Learning |
|---|---|---|
| Feature Extraction | Manual (requires domain experts) | Automated (learned from raw data) |
| Data Types | Structured (spreadsheets, tables) | Unstructured (images, audio, EHR notes) |
| Hardware | Standard CPUs | High-performance GPUs |
| Interpretability | High (e.g., Logistic Regression) | Low (“Black Box” nature) |
Automated Feature Learning
Deep learning has fundamentally changed medical imaging. Convolutional Neural Networks (CNNs) can automatically learn feature representations from raw pixel data. This means the model identifies the edges, textures, and shapes of a lesion without a radiologist having to define them first.
Recent Scientific research on medical imaging advances highlights that Vision Transformers (ViTs) have further improved on CNNs. While CNNs are great at looking at local patterns, ViTs can handle long-range dependencies in images, leading to more efficient, end-to-end laboratory management systems.
Pattern Recognition in Diagnostics
Pattern recognition is the “bread and butter” of machine learning clinical data. Whether it is an X-ray, an MRI scan, or a pathology slide, ML algorithms look for specific indicators of disease that might be too subtle for the human eye to catch consistently. For example, DL models are now used to predict cardiovascular risks simply by analyzing retinal images—a task that was previously considered impossible for human clinicians.
How to Use Machine Learning Clinical Data for Accurate Medical Diagnoses
Improving diagnostic precision is perhaps the most immediate benefit of AI in the clinic. By training models on massive, diverse datasets, we can create tools that support clinicians in making faster, more accurate decisions.
A prime example of this is seen in infectious disease management. A DL model recently achieved 87% sensitivity and 92% specificity in distinguishing COVID-19 from other lung diseases, boasting an impressive area under the curve (AUC) of 0.95. This level of precision allows for rapid triage in high-pressure hospital environments.
Improving Diagnostic Precision with Machine Learning Clinical Data
Beyond respiratory illnesses, AI is making massive strides in:
- Mammograms: Automatic detection of cancerous lesions with accuracy matching or exceeding human experts.
- Dermatology: AI-driven screening tools have shown a 95% early detection rate for skin cancer, significantly improving survival rates through early intervention.
- Ophthalmology: Validated algorithms can now detect diabetic retinopathy from fundus photographs in primary care settings, preventing vision loss before symptoms appear.
Laboratory Automation and Efficiency
Laboratory systems are often the bottleneck in patient care. AI-driven laboratory systems have achieved diagnostic accuracy with mean AUCs of 0.98 and 0.94 in various tests. By using high-throughput screening (HTS) and robotics, labs can analyze thousands of samples simultaneously. This doesn’t just improve speed; it improves the reliability of diagnoses by reducing human error in repetitive tasks.
Optimizing Clinical Trials and Drug Findy with Machine Learning Clinical Data
The pharmaceutical industry faces a daunting reality: it is estimated that only 12% of drug development programs achieve clinical trial success from phase 1 to launch. The cost of failure is measured in billions of dollars and years of lost time.
Machine learning clinical data helps tip the scales in favor of success. By integrating patient-level data and existing literature, we can use Clinical Trial Simulation for Alzheimer’s and other complex diseases. These simulations allow us to model disease progression and drug effects before we even recruit the first patient, optimizing trial parameters like sample size and dosage.
Accelerating Recruitment Using Machine Learning Clinical Data
Identifying study participants is currently one of the greatest causes of timeline delays. Trials often fail simply because they can’t find enough eligible patients.
Automated approaches are changing this. Advanced recruitment systems use a combination of patient records and eligibility criteria to increase monthly enrollment in breast cancer trials by 80%. By matching over 7,000 separate patient attributes with 11,000 eligibility criteria, these systems achieve a runtime of just 15.5 seconds per patient. This speed hints at a future where the recruitment bottleneck is completely eliminated.
Natural Language Processing for EHR Insights
A significant portion of clinical data is “hidden” in unstructured text—doctor’s notes, histologic reports, and discharge summaries. Natural Language Processing (NLP) is the key to open uping this data.
NLP allows us to:
- Extract Phenotypes: Combine disparate data points (codes, notes, lab results) to create a clear picture of a patient’s condition.
- Audit Accuracy: Inconsistencies in ICD coding for diseases like epilepsy can be corrected by NLP analysis of clinical narratives.
- Real-time Flagging: In acute cases like stroke, NLP can scan radiology reports in real-time to flag patients who meet specific trial criteria, ensuring they don’t miss narrow treatment windows.
Overcoming Technical and Ethical Challenges in Deployment
Despite the excitement, the path to implementation is fraught with pitfalls. One major hurdle is the “black box” nature of complex models. In medicine, a prediction is rarely enough; clinicians need to know why a model reached a certain conclusion.
To address this, we use “Shapley Additive Explanations” (SHAP values). These provide a means to assess the importance of individual features to a model’s ultimate output, making the results justifiable to medical professionals and regulatory bodies.
Managing Data Security and Patient Privacy
When dealing with machine learning clinical data, security is non-negotiable. Real-time breach detection is one of ML’s most practical applications in digital health. Algorithms can identify unusual patterns in data access that may indicate a cybersecurity threat, ensuring that patient privacy remains protected.
At Lifebit, we solve the “data moving” problem through federation. Our Trusted Research Environment (TRE) allows researchers to bring their models to the data, rather than moving sensitive patient records across borders. This approach satisfies strict privacy laws in the UK, Europe, and beyond.
Addressing Algorithmic Bias
We must be honest about the data we use. It has been estimated that nearly 90% of participants in clinical studies are White. If a model is trained on non-representative data, its predictions may be inaccurate for minority populations, potentially increasing health disparities.
Responsible machine learning clinical data implementation requires:
- Diverse Datasets: Ensuring training data reflects the global population.
- Prospective Validation: Moving beyond retrospective “proof of principle” studies to test models in real-world, diverse clinical settings.
- Regular Audits: Checking for “calibration drift” where a model’s accuracy declines as clinical practices or patient demographics change over time.
Frequently Asked Questions about Machine Learning Clinical Data
Can machine learning create digital twins for research?
Yes. By using neural networks and generative models (like GANs), we can create “digital twins”—virtual patient avatars that simulate how a real patient might respond to a treatment. This accelerates research and reduces costs by allowing for simulated clinical trials or “in silico” control arms, which are particularly valuable in rare disease research where patients are scarce.
How are digital biomarkers changing patient care?
Digital biomarkers are objective, quantifiable physiological and behavioral data collected via biosensors and wearables. Combined with machine learning clinical data, these allow for:
- Remote Monitoring: Detecting convulsive seizures with >90% sensitivity outside the hospital.
- Early Detection: Identifying voice biomarkers that signal the early stages of Alzheimer’s or Parkinson’s.
- Digital Therapeutics (DTx): Software-based treatments that adapt in real-time to a patient’s progress, common in neurology and mental health.
What are the regulatory problems for AI in healthcare?
Regulatory bodies like the FDA and EMA are rapidly adapting. Key developments include the CONSORT-AI and SPIRIT-AI extensions, which provide standardized guidelines for reporting AI interventions in clinical trials. The focus is shifting from static software to “Software as a Medical Device” (SaMD) that can learn and change, requiring new frameworks for continuous monitoring and validation.
Conclusion
The journey of machine learning clinical data from raw records to life-saving results is one of the most exciting frontiers in modern science. By bridging the gap between data silos and clinical insights, we are entering an era of high-performance medicine where AI augments human expertise to provide better, faster, and more equitable care.
At Lifebit, we are proud to power this transition. Our federated AI platform provides secure, real-time access to global biomedical and multi-omic data. Through our Trusted Data Lakehouse and R.E.A.L. (Real-time Evidence & Analytics Layer), we enable biopharma and government agencies to conduct large-scale research and pharmacovigilance with total confidence in data security and compliance.
Ready to turn your clinical data into results? Explore Lifebit’s Federated AI Platform.
Punchy, SEO-Driven News Article Titles
- How Lifebit Slashes Clinical Research Costs by 40% — Fast
- Stop Waiting Months: Predict Patient Outcomes in Days with Lifebit
- Why Siloed Clinical Data Is Costing You — And How Lifebit Fixes It
- 2026 Guide: Cut Clinical Trial Costs with Machine Learning Clinical Data
- Turn 275M Patient Records into Real-World Results Instantly with Lifebit
- 5 Data Mistakes Killing Your Clinical Research Budget
- Trusted by Global Biobanks: Secure Machine Learning Clinical Data Results

