The OMOP Advantage: Harmonizing Biomedical Data at NIAID

Why NIAID Data Harmonization with OMOP Matters for Global Health Research
NIAID data harmonization omop is the critical process of converting diverse, siloed clinical research data into a unified, analysis-ready format. This standardization is essential for accelerating infectious disease research and powering rapid public health responses.
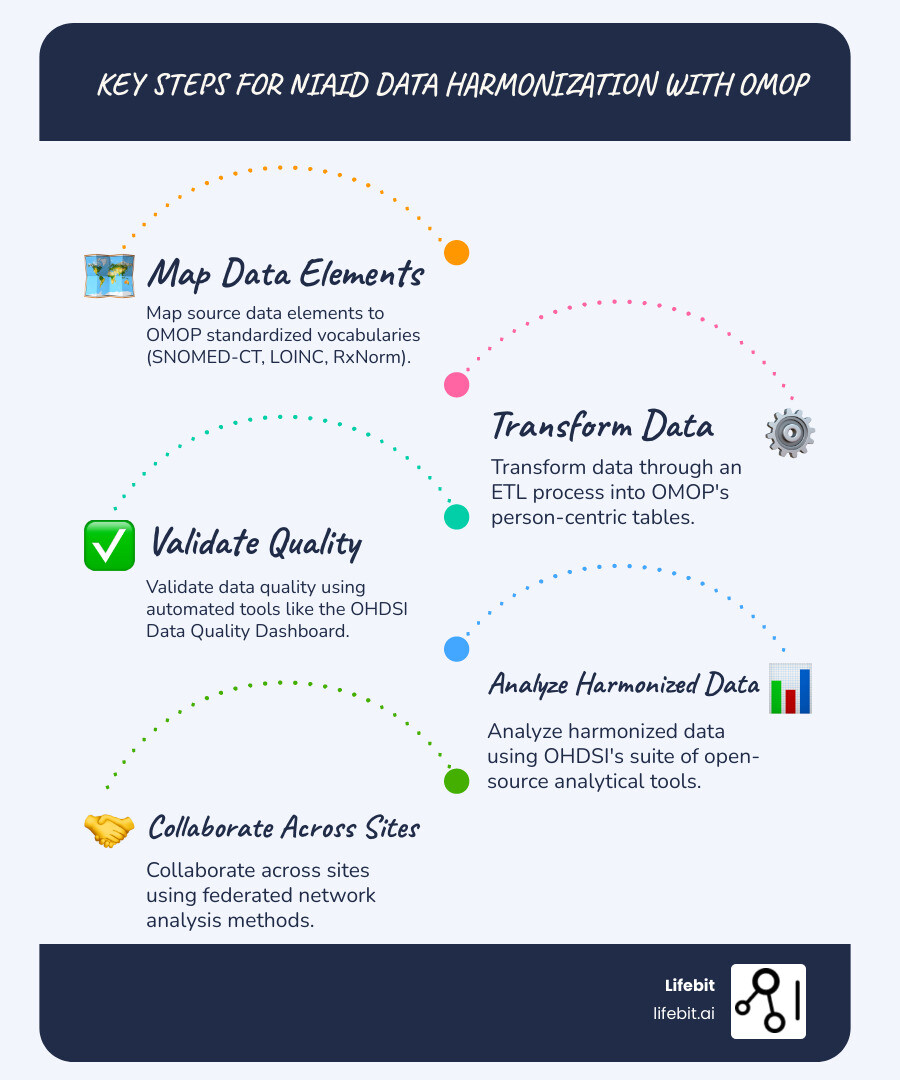
Quick Answer: Key Steps for NIAID Data Harmonization with OMOP
- Map your source data elements to OMOP standardized vocabularies (SNOMED-CT, LOINC, RxNorm)
- Transform data through an ETL (Extract, Transform, Load) process into OMOP’s person-centric tables
- Validate data quality using automated tools like the OHDSI Data Quality Dashboard
- Analyze harmonized data using OHDSI’s suite of open-source analytical tools
- Collaborate across sites using federated network analysis methods
The National Institute of Allergy and Infectious Diseases (NIAID) funds research across hundreds of sites worldwide, but a persistent challenge undermines its speed and power: data doesn’t speak the same language. One site records a drug using WHO ATC codes, another uses RxNorm, and a third uses a proprietary system. Combining these datasets to answer urgent questions requires months of manual data wrangling—or it’s simply impossible.
This is where the Observational Medical Outcomes Partnership (OMOP) Common Data Model provides a solution. OMOP is a standardized blueprint that transforms messy, heterogeneous data into a clean, analysis-ready format, enabling researchers to query massive, multi-site datasets as if they were a single database.
During the COVID-19 pandemic, the National COVID Cohort Collaborative (N3C) used OMOP to harmonize over 23 billion clinical records from 18 million patients across 75 institutions in months. This enabled real-time answers on treatment effectiveness and risk factors. For NIAID networks studying HIV, tuberculosis, and other global threats, adopting OMOP can similarly accelerate evidence generation and enable large-scale international collaboration.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. We build federated data analysis platforms that enable secure NIAID data harmonization omop across global research networks. With over 15 years in computational biology, I’ve seen how standardized data models transform research velocity and quality.
The Harmonization Hurdle: Why Combining NIAID Data is So Complex
Trying to solve a global health puzzle with pieces from different boxes—that’s the reality for researchers combining data from NIAID-funded studies. The goal is to make clinical research data traceable, accessible, interoperable, and reproducible. The reality is far from it.
A staggering 85% of research studies never translate to meaningful clinical findings. A 2016 Nature survey found over 70% of researchers struggle to reproduce others’ experiments. This “reproducibility crisis,” highlighted by John Ioannidis in 2005, represents lives that could have been saved and outbreaks that could have been contained faster.
The root cause is heterogeneous data.
NIAID-funded consortia like the International epidemiology Databases to Evaluate AIDS (IeDEA) gather data from hundreds of sites across dozens of countries. The potential is enormous, but combining the data is like merging 400 different filing systems. Without a common language for niaid data harmonization omop, timely analysis is impossible.
The High Cost of Unharmonized Data
The obstacles are not just technical; they are embedded in how health data is collected globally. The consequences fundamentally undermine the speed and impact of NIAID-funded research.
- Semantic Chaos: What one site calls “patient age” might be “age at diagnosis” at another. A tuberculosis diagnosis could be recorded using ICD-9 (011.9), ICD-10 (A15.0), SNOMED-CT (56717001), or a local, non-standard term like ‘TB positive’. Furthermore, lab results for viral load might be recorded in ‘copies/mL’ at one site and ‘log10 copies/mL’ at another, with no explicit unit information. Without a common vocabulary and unit standardization, these data points cannot be computationally compared.
- Structural and Quality Issues: Database architectures differ dramatically. Missing values, illogical dates (e.g., discharge before admission), and duplicate entries are common. For instance, a ‘null’ value in a lab result field could mean the test was never ordered, the result is pending, or the value was zero. Each possibility has vastly different clinical implications. These data landmines can derail analyses or produce misleading results.
- Longitudinal Data Complexity: NIAID-funded research, particularly for chronic infectious diseases like HIV, relies on longitudinal data collected over many years. Harmonizing this data is uniquely challenging. Patient identifiers may change over time, clinic visits may be recorded inconsistently, and the evolution of treatment regimens and diagnostic criteria must be accounted for. Merging these complex patient journeys from different systems without a common structure is a monumental task.
- Delayed Research and Public Health Responses: Months or years are lost to manual data cleaning instead of being spent on analysis. By 1970, if data on infant sleeping positions had been properly aggregated and analyzed, over 60,000 infant deaths from SIDS could have been prevented. That is the human cost of delayed harmonization.
- Inaccurate and Irreproducible Findings: Errors that slip through manual harmonization undermine research validity and contribute to the reproducibility crisis.
- Wasted Resources and Reduced Power: Scientists spend valuable time on data cleaning instead of findings. Smaller, isolated datasets lack the statistical power to detect subtle but clinically significant effects, leaving important findings hidden.
- Barriers to Collaboration: The inability to combine data effectively across sites reduces the generalizability of findings. During a health crisis, this means insights arrive too late to inform urgent policy decisions.
These challenges highlight an urgent need for a robust, standardized approach—one that empowers researchers and accelerates findings. That’s exactly what niaid data harmonization omop methodologies provide.
The OMOP Blueprint: A Standardized Framework for Research-Ready Data
Imagine a symphony where every musician reads a different language of sheet music. The result is chaos. This is what researchers face with health data—until OMOP enters the stage.
The Observational Medical Outcomes Partnership (OMOP) Common Data Model is an open-source framework that brings order to diverse healthcare data. Maintained by the Observational Health Data Sciences and Informatics (OHDSI) community, OMOP provides a standardized blueprint that transforms heterogeneous clinical data into a uniform, analysis-ready format.
Through an Extract, Transform, Load (ETL) process, messy source data from electronic health records, claims, or registries is converted into a common structure. Once transformed, researchers can query data across hundreds of institutions as if it were a single database. For niaid data harmonization omop projects, a clinic in Kenya and a hospital in Boston can contribute to the same analysis without changing how they collect data locally.
Key Components of the OMOP CDM for NIAID Research
The OMOP CDM organizes a patient’s health journey through two core components:
Standardized Tables create a logical structure for clinical information. The PERSON table holds demographics, while other key tables capture clinical events: VISITOCCURRENCE (encounters), CONDITIONOCCURRENCE (diagnoses), DRUGEXPOSURE (medications), MEASUREMENT (lab results), PROCEDUREOCCURRENCE (interventions), and OBSERVATION (other clinical facts). Beyond these ‘event’ tables, OMOP includes derived tables like DRUGERA and CONDITIONERA. These are computationally generated tables that group individual drug exposures or condition occurrences into continuous episodes of care. For example, multiple prescriptions for the same antiretroviral drug are collapsed into a single ‘drug era,’ simplifying analyses on treatment duration and adherence.
Standardized Vocabularies are the magic that enables true harmonization. The CONCEPT table acts as a universal dictionary, mapping all clinical data to a standard concept. A diagnosis arriving as an ICD-10 code from one site and a local code from another are both mapped to the same standard SNOMED-CT concept, making them identical for analysis. Key vocabularies include SNOMED-CT for conditions, LOINC for labs, and RxNorm for medications. The power of these vocabularies is amplified by their hierarchical structure. For instance, SNOMED-CT organizes concepts from general to specific (e.g., ‘Viral disease’ -> ‘HIV’ -> ‘HIV-1’). This hierarchy, captured in OMOP’s CONCEPT_ANCESTOR table, allows researchers to query data at different levels of granularity—for example, to find all patients with any type of viral pneumonia, not just those coded with a specific subtype.
This system means a researcher can write one query to find all HIV patients across a global network, regardless of how each site originally coded the diagnosis.
How OMOP Directly Addresses Harmonization Challenges
OMOP solves the core problems that make multi-site research so difficult:
- Semantic Interoperability: By mapping all data to standard vocabularies, OMOP ensures “tuberculosis” means the same thing everywhere, eliminating confusion from inconsistent codes and definitions.
- Standardized Analytics: Once data is in OMOP format, you can use the same analytical code across every dataset. The OHDSI community provides a rich ecosystem of open-source tools for analysis, which you can explore here.
- Transparent Data Lineage: A well-documented ETL process creates an audit trail, showing exactly how data was transformed from source to OMOP, which builds trust and supports reproducibility.
- Large-Scale Network Studies: OMOP enables distributed analysis, where code is sent to the data, not the other way around. This respects patient privacy while dramatically boosting statistical power. The National COVID Cohort Collaborative proved this model by integrating data from multiple sources into a unified OMOP format, creating a connected resource for thousands of researchers.
For niaid data harmonization omop initiatives, this common language is transformative, turning months of data wrangling into weeks and making previously impossible analyses routine.
A Practical Guide to niaid data harmonization omop Implementation
How do you take a messy collection of databases and spreadsheets from dozens of sites and turn them into a unified, analysis-ready OMOP dataset? The process revolves around the ETL—Extract, Transform, Load—pipeline, where raw data is systematically converted into the OMOP format.
While it can be complex, modern tools and methodologies make it increasingly accessible. The journey involves understanding your source data, defining mapping rules, building the ETL, rigorously assessing data quality, and planning for ongoing maintenance.
Step 1: The ETL (Extract, Transform, Load) Process
The ETL process is where the real work of niaid data harmonization omop happens.
- Extract: Pull data from its source, whether it’s REDCap, SQL databases, or CSV files. The goal is to get the data into a workable format without losing information.
- Transform: This is the heavy lifting. You apply mapping rules to standardize the data. A diagnosis code from a local system is translated into a standard OMOP Concept ID. Date formats are standardized. Illogical values are flagged. Vocabulary mapping is crucial here, ensuring a local code for “HIV-1 infection” and an ICD-10 code (B24) both map to the same standard SNOMED-CT concept (e.g., Concept ID 86406008 for ‘Human immunodeficiency virus 1 infection’). This mapping process is meticulous. For each source data element (e.g., a column named ‘DIAGNOSIS_CODE’ in a source table), a rule must be created to map its values to a target OMOP Concept ID. For example:
IF source_table.DIAGNOSIS_CODE = 'B24' THEN map to target_concept_id = 86406008. - Load: Once cleaned and standardized, the data is loaded into the OMOP CDM tables, creating a unified, analysis-ready database.
Step 2: Leveraging Tools for Quality and Analysis
You don’t have to build everything from scratch. Powerful tools can dramatically reduce the technical burden.
The Harmonist Data Toolkit is a game-changer for consortia with limited programming resources. Developed for the IeDEA consortium, it’s an interactive, web-based application that checks data quality without requiring local coding expertise. It uses REDCap to store data model rules and automatically assesses whether a dataset conforms, catching issues like duplicates, formatting errors, and illogical dates. The IeDEA Harmonist Toolkit is available on GitHub.
The OHDSI community tools are invaluable for OMOP-specific work. The OHDSI Data Quality Dashboard provides comprehensive checks, while tools like ATLAS let you design and execute studies across multiple OMOP databases through a web interface.
AI-assisted harmonization is also emerging as a powerful accelerator. Emerging AI systems use Large Language Models to automate tedious mapping tasks, with a human-in-the-loop approach to validate suggestions. At Lifebit, our federated AI platform is designed to handle these challenges, enabling secure, real-time access to global biomedical data with built-in harmonization capabilities.
Step 3: Mitigating Limitations and Ensuring Success
Successful niaid data harmonization omop implementation requires careful planning.
- Computational Demands: Harmonizing large datasets requires robust, cloud-based infrastructure. Lifebit’s Trusted Research Environment (TRE) is architected to handle this scale securely.
- Non-Standard Data: Specialized data like raw genomics or complex imaging may require extensions to the OMOP model or complementary data structures. For example, while raw genomic data (VCF/BAM files) is not stored directly in OMOP, the model can be extended. A common approach is to store summary-level genomic findings (e.g., presence of a specific mutation like ‘KRAS G12C’) in the MEASUREMENT or OBSERVATION table, while linking to the raw file’s location in a secure repository. For imaging data, DICOM metadata can be stored in OMOP tables with a pointer to the full image file.
- Domain Expertise: Collaboration between clinicians, data managers, and informaticians is non-negotiable. You can’t map clinical data without understanding what it represents.
- Data Governance and Privacy: Clear data use agreements, Privacy-Preserving Record Linkage (PPRL), and robust de-identification are critical for multi-site collaborations. Security standards like NIST SP 800-53 and ISO/IEC 27001 are essential.
- Stakeholder Engagement and Governance: Harmonization is as much a social and political challenge as a technical one. Success requires early and continuous engagement with all stakeholders: principal investigators, clinicians, data managers, IT staff, and patients. Establishing a clear data governance framework—with transparent rules for data access, use, and publication—is essential for building trust and ensuring long-term sustainability, especially in international consortia funded by NIAID.
- Ongoing Maintenance: Harmonization is not a one-time project. It requires continuous data quality monitoring to maintain integrity as data sources and the OMOP model evolve.
The Payoff: Real-World Wins and Collaborative Power
When research networks invest in niaid data harmonization omop, they’re not just organizing data—they’re changing what’s possible in infectious disease research. The impact is faster findings, saved lives, and global collaboration on a scale no single institution could manage alone.

Success Stories in niaid data harmonization omop
The proof is in the results. Landmark initiatives show how powerful harmonized data can be.
- The National COVID Cohort Collaborative (N3C) stands as the most dramatic demonstration. It harmonized over 23 billion clinical records from 18 million patients across 75 institutions into the OMOP CDM within months. This gave over 3,800 researchers real-time access to a massive dataset, informing treatment decisions and identifying risk factors as the pandemic evolved.
- The IeDEA consortium (International epidemiology Databases to Evaluate AIDS) spans almost 400 HIV care sites in 44 countries. Their Data Exchange Standard and the Harmonist Data Toolkit have empowered five international infectious disease consortia—including RePORT International (tuberculosis) and NA-ACCORD (HIV)—to improve data quality with minimal local programming expertise.
- The All of Us Research Program is building a massive, diverse dataset linking genomic and clinical information, all harmonized to OMOP. With 245,388 whole-genome sequences released and 77% of participants from under-represented communities, it enables precision medicine insights for populations historically excluded from research.
Benefits for Multi-Site and International Collaboration
OMOP harmonization delivers concrete benefits that transform how NIAID-funded research operates.
- A Common Language for Data: When a researcher in Mumbai, a clinician in Johannesburg, and an official in Boston all use OMOP-harmonized data, they are speaking the same language. This eliminates months of bespoke data translation for every new collaboration.
- Distributed Network Analysis: Design a study once and run it across dozens of sites without pooling sensitive patient data. Each institution keeps its data firewalled, yet researchers can query the entire network, improving privacy while boosting statistical power.
- Accelerated Findings for Infectious Diseases: Harmonized data means researchers can start analyzing within weeks instead of spending months on data wrangling. During an outbreak, this speed can save lives.
- Increased Statistical Power and Reproducibility: Combining data from multiple sites allows for the detection of rare events and subtle treatment effects. Because the process is standardized, findings are inherently more reproducible.
- Broader Generalizability: Research on diverse, harmonized datasets produces findings that are more clinically relevant to the real-world populations we aim to help.
At Lifebit, our federated AI platform is built to enable this secure, large-scale collaboration. Our Trusted Research Environment (TRE) and Real-time Evidence & Analytics Layer (R.E.A.L.) provide the infrastructure to make these success stories possible at scale.
Frequently Asked Questions about NIAID Data and OMOP
What is the main benefit of using OMOP for NIAID-funded research?
The primary benefit is creating a standardized, analysis-ready dataset from diverse sources. This accelerates research by enabling standardized analytics, improves reproducibility, and powers large-scale, multi-site collaborations. By creating a common data language, NIAID networks can tackle complex infectious diseases more effectively, leading to faster translation of findings into patient care and public health policy.
Can OMOP handle all types of NIAID research data?
OMOP is incredibly robust for observational clinical data like diagnoses, procedures, medications, and lab results. However, highly specialized data types, such as raw genomic sequences or complex imaging data, may require extensions to the model or be linked to external specialized repositories. The N3C’s ongoing work to incorporate data on long COVID and social determinants of health shows how OMOP can be extended to capture more nuanced information.
How long does it take to convert a dataset to the OMOP CDM?
The timeline varies significantly based on the source data’s complexity, size, and quality, as well as available resources. A simple, clean dataset might take a few weeks, while a large, multi-site network can take many months for the initial setup. However, once established, the harmonization process can be automated. Emerging AI-assisted tools are significantly accelerating this timeline, reducing manual effort and speeding up the entire process.
What is the difference between OMOP and other common data models like PCORnet or i2b2?
While all three models aim to standardize health data for research, they have different origins and focuses. i2b2 (Informatics for Integrating Biology and the Bedside) excels at cohort discovery and hypothesis generation through its ‘star schema’ structure, which is intuitive for many clinicians. PCORnet (National Patient-Centered Clinical Research Network) is designed to support comparative effectiveness research and is optimized for pragmatic clinical trials across its network. OMOP, maintained by the global OHDSI community, is distinguished by its deep integration of standardized vocabularies and its vast ecosystem of open-source analytical tools. This makes it exceptionally powerful for large-scale observational research, evidence generation, and prediction modeling across highly diverse, international networks, aligning perfectly with the global scope of NIAID’s mission.
Conclusion: Powering the Future of Federated Health Research
The journey to niaid data harmonization omop is about fundamentally changing how global health research happens—making it faster, more collaborative, and more effective at saving lives.
The challenges of inconsistent codes and variable data quality across hundreds of international sites are daunting. But the OMOP Common Data Model is a battle-tested framework that enables researchers to speak a common data language, run standardized analyses across continents, and generate evidence at a scale previously unimaginable.
The evidence is clear: N3C harmonized data from 75 institutions in months, IeDEA transformed data quality across 44 countries, and the All of Us program is building an unprecedentedly diverse genomic dataset on an OMOP foundation. These are real-world demonstrations that harmonized data accelerates scientific findings.
For NIAID networks tackling global health threats, adopting OMOP means launching multi-site studies in weeks, not years. It means when the next pandemic emerges, the infrastructure will be ready to generate answers in real-time.
The future of biomedical research is federated and AI-powered. The NIH Strategic Plan for Data Science 2025-2030 envisions an infrastructure where algorithms can train on harmonized data without compromising privacy and where researchers collaborate seamlessly across borders.
This future requires platforms built for the challenge. That’s what Lifebit’s platform delivers. Our Trusted Research Environment and R.E.A.L. layer are designed to power the large-scale, compliant, federated research that NIAID networks need.
By embracing niaid data harmonization omop, research networks are building the foundation for decades of accelerated findings. The question isn’t whether to harmonize, but how quickly we can make it happen.
Learn more about our federal health solutions and how we’re transforming biomedical research.

