Clinical Data Security Made Easy (Because HIPAA Isn’t a Suggestion)

Secure clinical data: 6 Critical Steps
Why Healthcare Data Security Can’t Wait Another Day
Secure clinical data is the bedrock of modern healthcare. It involves protecting patient information with encryption, access controls, and compliance frameworks like HIPAA, all while enabling vital research and care. Key components include:
Essential Components of Secure Clinical Data:
- Administrative safeguards: Policies, training, and access management
- Physical safeguards: Facility controls and workstation security
- Technical safeguards: Encryption, authentication, and audit controls
- Compliance frameworks: HIPAA, GDPR, and industry standards
- Incident response: Breach detection, containment, and recovery plans
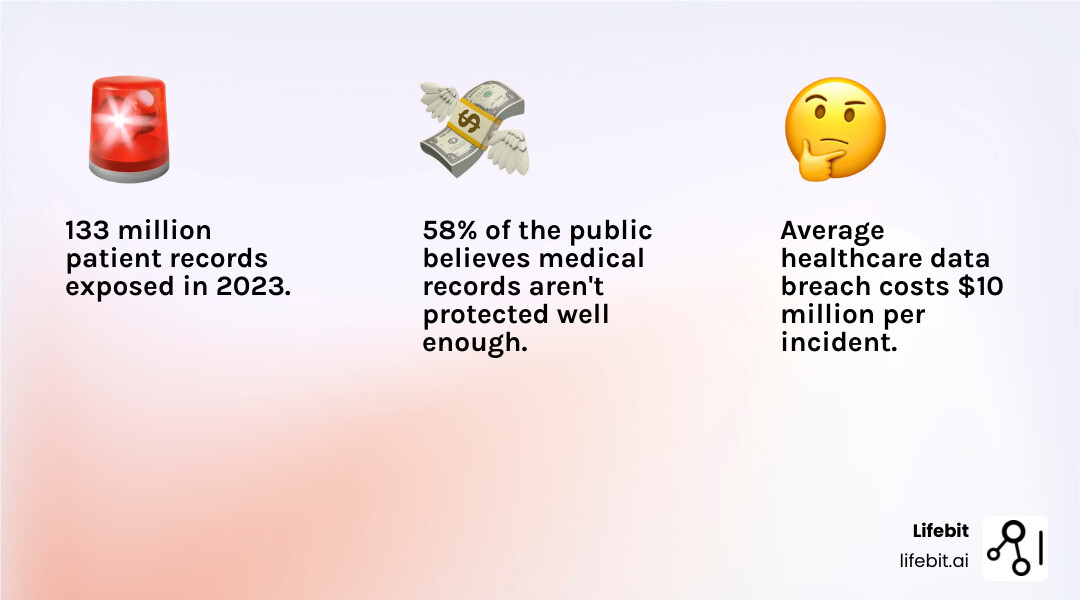
The numbers paint a stark picture. Over 133 million patient records were exposed in 2023 alone across more than 725 cyberattacks. Healthcare organizations face the highest data breach costs of any industry—averaging $10 million per incident.
Despite this, 58% of the public feels their medical records are inadequately protected. Compromised data doesn’t just violate compliance; it disrupts care, erodes trust, and puts lives at risk.
Digital change—through EHRs, telehealth, and cloud research—has created both opportunities and vulnerabilities. Organizations now manage vast, complex datasets across multiple jurisdictions.
As one healthcare security expert noted: “Even if nothing that identifies me were ever published, I still worry about a professional health researcher seeing my medical records.” This sentiment, shared by 50% of patients, highlights the delicate balance between advancing medical research and protecting individual privacy.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. With over 15 years of experience developing secure clinical data platforms, I’ve seen how the right security approach can accelerate research in federated environments without compromising patient trust.
The Regulatory and Threat Landscape of Healthcare Data
Digital change has revolutionized healthcare, but it has also created a perfect storm of regulatory complexity and evolving cyber threats. Securing secure clinical data is no longer just an IT issue; as the American Hospital Association notes, the importance of cybersecurity in protecting patient safety is a core component of patient care.
Key Regulations for Secure Clinical Data
A complex web of regulations governs the use and protection of patient data. Understanding these frameworks is the first step toward compliance and building patient trust.
The Health Insurance Portability and Accountability Act (HIPAA) established the foundational national standards in the U.S. for protecting sensitive patient health information (PHI). The HIPAA Security Rule, detailed by the U.S. Department of Health and Human Services, is particularly crucial, mandating three types of safeguards for electronic PHI (ePHI). HIPAA Security Rule standards.
- Administrative Safeguards: These are the policies and procedures that form the human element of security. They include conducting regular risk analyses, designating a security officer, implementing workforce security policies, managing information access (authorizing, establishing, and modifying access), providing security awareness training, and creating contingency plans for emergencies.
- Physical Safeguards: These controls protect physical access to systems and buildings. They encompass facility access controls (e.g., locks, alarms, and authorized access), workstation use policies (defining how workstations are to be used to access ePHI), workstation security (implementing physical safeguards for all workstations), and device and media controls (governing the movement and disposal of hardware and electronic media containing ePHI).
- Technical Safeguards: These are the technological locks and keys. Key requirements include implementing access controls (e.g., unique user IDs, emergency access procedures), maintaining audit logs to record system activity, ensuring data integrity to prevent improper alteration or destruction, using authentication to verify user identities, and securing data transmissions with encryption.
The HITECH Act of 2009 significantly strengthened HIPAA’s enforcement by increasing penalties for non-compliance, introducing stricter breach notification requirements, and promoting the adoption of Electronic Health Records (EHRs).
For organizations handling data from European citizens, the General Data Protection Regulation (GDPR) imposes even stricter rules. It has global reach and mandates principles like data minimization (collecting only necessary data), purpose limitation (using data only for specified purposes), and granting individuals the “right to be forgotten.” Our approach ensures GDPR compliant data handling, which is critical for international research collaborations. These frameworks impose significant financial penalties—up to 4% of global annual revenue for GDPR—and provide the legal foundation for patient trust.
Top Threats and Vulnerabilities
The HIPAA Journal’s analysis of 2023 data shows that cyberattacks and ransomware exposed over 133 million patient records across 725 incidents, demonstrating that the threat is both real and growing. Healthcare data breach statistics.

Phishing and Spear Phishing: While standard phishing scams use deceptive mass emails to trick employees into revealing credentials, spear phishing is far more dangerous. Attackers research their targets and craft personalized emails that appear to be from a trusted colleague or department, dramatically increasing the likelihood of success.
Ransomware Attacks: These attacks have evolved beyond simple encryption. Modern ransomware employs double-extortion tactics, where attackers not only encrypt an organization’s data but also exfiltrate it, threatening to release the stolen data publicly if the ransom isn’t paid. Some have even moved to triple extortion, adding DDoS attacks or directly contacting patients whose data was stolen.
Insider Threats: These threats come in multiple forms. They can be malicious (a disgruntled employee intentionally selling data), negligent (an employee accidentally emailing PHI to the wrong recipient or falling for a phishing scam), or compromised (an employee whose credentials have been stolen by an external attacker). High staff turnover and insufficient training exacerbate this risk.
Unsecured Networks and Outdated Legacy Systems: Many healthcare organizations still rely on older systems that no longer receive security updates, making them vulnerable to known exploits. Compounding this, unsecured wireless networks, misconfigured cloud services, and a lack of network segmentation can allow an attacker who gains a foothold in one area to move freely across the entire network.
Medical Device (IoMT) Vulnerabilities: The Internet of Medical Things (IoMT) connects devices like infusion pumps, patient monitors, and MRI machines to the network. While this improves care, these devices often lack robust, built-in security, creating backdoors into hospital networks. A single vulnerable device could become the entry point for an attack that exposes millions of patient records.
Supply Chain Attacks: Attackers are increasingly targeting third-party vendors, such as software providers or billing companies, that have access to a healthcare organization’s systems. By compromising a single trusted vendor, attackers can gain access to all of that vendor’s clients, creating a widespread and devastating impact.
Hacktivism: This involves cyberattacks motivated by political or social agendas rather than financial gain. Healthcare and pharmaceutical companies can be targeted by groups seeking to make a statement, adding an unpredictable and disruptive threat vector.
Core Components & Best Practices for Secure Clinical Data
Securing secure clinical data relies on the foundational principles of the CIA Triad: Confidentiality (keeping data private), Integrity (ensuring data is accurate and trustworthy), and Availability (making data accessible to authorized users when needed). A failure in any one of these areas can have dire consequences—a breach of confidentiality erodes trust, a loss of integrity could lead to misdiagnosis, and a lack of availability during a ransomware attack can halt patient care entirely. These principles, outlined in frameworks from authorities like the NIST Computer Security Resource Center, are the foundation of a robust security posture.
Primary Components of Data Security
Building a resilient security framework requires orchestrating multiple, layered components to work in harmony, creating a defense-in-depth strategy.

Data Encryption: This is the process of translating information into a code that only authorized parties can decipher. It is essential to protect data in all three states:
- At Rest: Data stored on servers, laptops, or databases, typically protected with strong algorithms like AES 256-bit.
- In Transit: Data moving across a network, protected by protocols like Transport Layer Security (TLS).
- In Use: Data being actively processed in memory. Emerging technologies like confidential computing keep data encrypted even during analysis, providing the highest level of protection.
Access Control Systems: These act as digital gatekeepers, enforcing the principle of least privilege. Common models include:
- Role-Based Access Control (RBAC): Grants permissions based on job function. For example, a nurse’s role allows access to patient records on their assigned floor, while a billing clerk’s role grants access only to financial information.
- Attribute-Based Access Control (ABAC): Uses more granular context for dynamic decisions. For instance, a doctor can access a patient’s record only if they are the attending physician (attribute), during work hours (attribute), and from a hospital-issued device (attribute). These systems are key to Preserving Patient Data Privacy and Security.
Network Security: This involves creating protective barriers and monitoring traffic. Key tools include firewalls to filter traffic, Intrusion Detection and Prevention Systems (IDS/IPS) to identify and block malicious activity, and network segmentation to isolate critical systems, preventing a breach in one area from spreading to others.
Endpoint Security: Every device connecting to the network—from laptops and servers to medical equipment—is an endpoint that must be secured. Modern Endpoint Detection and Response (EDR) solutions go beyond traditional antivirus, using behavioral analysis to detect and respond to sophisticated threats in real time.
Physical Security: Often overlooked in a digital world, this remains vital. It includes restricted access to data centers using biometric scanners or key cards, surveillance systems, and environmental controls to protect servers from physical theft, damage, or tampering.
Data Classification: This involves categorizing information by its sensitivity level (e.g., Public, Internal, Confidential, Restricted). This ensures that the most critical data, like PHI, receives the highest level of protection and handling controls.
Data Loss Prevention (DLP): These systems act as a final safeguard, monitoring for and blocking unauthorized transfers of sensitive data. Using content inspection and contextual analysis, a DLP tool can automatically stop an employee from emailing a file containing patient records to an external address or uploading it to an unauthorized cloud service.
List of Best Practices for Protecting Sensitive Data
Protecting secure clinical data requires a comprehensive strategy that combines technology, processes, and people.
-
Implement Strong Access Controls: Enforce the principle of least privilege rigorously. Augment this with multi-factor authentication (MFA), which requires users to provide two or more verification factors (e.g., a password and a code from a mobile app) to gain access.
-
Utilise End-to-End Encryption: Encrypt data everywhere—at rest, in transit, and, where possible, in use. Use industry-standard algorithms like AES 256-bit and ensure robust key management practices are in place, as encryption is only as strong as the protection of its keys.
-
Conduct Regular Security Audits and Penetration Testing: Proactively identify and fix weaknesses through a continuous cycle of security assessments. This includes automated vulnerability scanning, regular penetration testing by third-party experts to simulate real-world attacks, and compliance audits against frameworks like HIPAA and ISO 27001.
-
Deploy a Security Information and Event Management (SIEM) System: Centralize logging and security event data from across your network. A SIEM allows for real-time threat detection, forensic investigation, and compliance reporting by correlating events from different sources to identify patterns of malicious activity.
-
Foster a Culture of Security: Your workforce is your first line of defense. Implement continuous employee training that covers phishing recognition, password hygiene, social engineering tactics, and incident reporting procedures. Regular phishing simulations can test and reinforce this training.
-
Maintain a Robust Backup & Disaster Recovery Plan: Ensure business continuity and minimize data loss after an incident. Follow the 3-2-1 rule (three copies of your data, on two different media types, with one copy off-site). Regularly test your backup restoration process to ensure it works and meets your defined Recovery Time Objectives (RTO) and Recovery Point Objectives (RPO).
These practices are essential for enabling HIPAA Compliant Data Analytics without compromising patient trust.
Navigating Digitization and Modern Data Challenges
The digital revolution in healthcare—from Electronic Health Records (EHRs) to telehealth and AI-driven diagnostics—offers incredible benefits but also dramatically expands the security perimeter. Each new connection, device, and third-party system creates a potential vulnerability, making it a significant challenge to share secure clinical data safely for care and research across different institutions.
The Impact of Digitization on Data Security
Digital transformation requires a new approach to security, one that balances the immense benefits with the inherent risks. Acknowledging both sides is key to building a resilient strategy.
| Pros of Healthcare Digitization | Cons of Healthcare Digitization |
|---|---|
| Centralized Data Management: EHRs centralize patient information, providing a holistic view for better, more informed care decisions. | Single Point of Failure: Centralized databases become high-value targets for attackers, where a single breach can expose millions of records. |
| Improved Access for Care: Providers can access patient records from anywhere, enabling effective telehealth, remote consultations, and faster emergency care. | Increased Attack Surface: Every new device (IoMT), mobile app, cloud service, and remote connection is a potential entry point for attackers. |
| Enhanced Research Capabilities: Aggregated, large-scale datasets enable researchers to identify patterns, test hypotheses, and develop new treatments at an unprecedented pace. | Privacy Concerns with Data Aggregation: Patients worry that their de-identified data in large research pools could be re-identified and traced back to them, eroding trust. |
| Operational Efficiency: Digital systems reduce paperwork, streamline administrative workflows, and automate tasks, freeing up staff to focus on patient care. | User Error and Training Gaps: Untrained or negligent staff can accidentally expose data through misconfigurations, weak passwords, or by falling for sophisticated phishing scams. |
| Improved Data Interoperability: Standards like FHIR make it easier for different systems to share data, improving care coordination and enabling seamless data exchange. | Third-Party and Supply Chain Risk: Reliance on external software vendors, cloud providers, and service partners introduces risks if those third parties have weak security postures. |
Modern Solutions for Secure Data Collaboration
Fortunately, technology also provides innovative solutions that allow for secure collaboration, enabling research without compromising patient privacy.

Federated Data Analysis: Instead of centralizing sensitive data into a single repository, this paradigm-shifting approach brings the analysis to the data. The process is simple yet powerful: a researcher sends an analytical query to multiple organizations, each organization executes the query locally on its own data behind its firewall, and only the aggregated, non-identifiable results are returned and combined. The sensitive raw data never moves, dramatically reducing the risk of a breach during transfer or from a centralized database.
Secure Data Environments (SDEs) and Trusted Research Environments (TREs): These are highly controlled digital laboratories designed for analyzing sensitive data. Researchers are given access to the data within a secure, monitored environment that prevents data extraction. Key features include secure remote access, the prohibition of downloading or copy-pasting raw data, a curated set of analysis tools, and a rigorous “safe output” process where all results are vetted for disclosure risk before being released to the researcher. Learn more about What is a Secure Data Environment (SDE)? and Trusted Research Environments on our blog.
Confidential Computing: This breakthrough technology protects data even while it is being processed. It utilizes hardware-based secure enclaves, also known as Trusted Execution Environments (TEEs). Think of a TEE as a locked, opaque box: data is loaded into the enclave in an encrypted state, processed inside, and the results are encrypted before they exit. The contents of the enclave are invisible even to the cloud provider, system administrators, and the host operating system, offering unparalleled protection for data in use.
Data Tokenization and De-identification: These techniques reduce the risk of data exposure by replacing or removing sensitive information. De-identification, following standards like the HIPAA Safe Harbor method, removes 18 specific personal identifiers. Tokenization goes a step further by replacing a sensitive data element (like a patient ID) with a non-sensitive substitute, or “token.” The token can be used for processing and analytics across systems, while the original data remains securely stored in a limited-access vault.
These solutions are not mutually exclusive; in fact, they are most powerful when combined. A federated network of TREs using confidential computing represents the gold standard for secure, collaborative research, making it possible to unlock the power of healthcare data while maintaining the highest standards of privacy and security.
Managing a Data Breach and Maintaining Public Trust
Even with strong, layered defenses, the unfortunate reality is that breaches can still happen. In this event, how an organization responds is just as critical as the defenses it had in place. A well-executed, transparent response can mitigate damage, meet legal obligations, and begin the long process of rebuilding trust. A poor one can amplify the crisis, leading to greater financial penalties, reputational ruin, and a permanent loss of patient confidence when secure clinical data is compromised.
Essential Steps in Healthcare Data Breach Management
A clear, well-rehearsed incident response (IR) plan is essential for rapid and effective action. The process generally follows these key phases:
-
Identification and Activation: The first step is detecting the breach, which may come from an internal security alert, a user report, or an external notification. Once an incident is declared, the pre-defined Incident Response Team—typically comprising IT security, legal, communications, and executive leadership—must be immediately activated.
-
Containment: This is a critical race against time to limit the damage. The primary goal is to stop the unauthorized access and prevent the attacker from moving laterally across the network. Actions may include isolating compromised systems from the network, disabling breached user accounts, and blocking malicious IP addresses at the firewall.
-
Eradication and Evidence Preservation: Once contained, the threat must be removed from the environment. This could involve eliminating malware, patching vulnerabilities, and ensuring all backdoors are closed. Simultaneously, forensic data must be preserved by creating disk images and collecting logs to understand the attack and meet legal requirements.
-
Investigation and Scope Assessment: With the immediate threat neutralized, a thorough investigation begins. Digital forensics experts work to determine the root cause, the attacker’s methods, and, most importantly, the scope of the breach: what specific data was accessed or exfiltrated, which patients were affected, and for how long the attacker had access.
-
Notification: Transparent communication is paramount. Under the HIPAA Breach Notification Rule, organizations must notify affected individuals “without unreasonable delay” and no later than 60 calendar days following the discovery of a breach. If the breach affects more than 500 residents of a state, prominent media outlets must also be notified. This contrasts with GDPR’s much stricter 72-hour notification deadline. Notifications should clearly explain what happened, what data was involved, and what steps patients can take to protect themselves, such as enrolling in offered credit monitoring services.
-
Recovery and Post-Incident Review: This phase involves securely restoring systems from clean backups and validating that they are fully operational and secure. Crucially, the work isn’t over. A post-incident review or “lessons learned” session is essential to analyze the breach, identify weaknesses in security controls or procedures, and implement improvements to prevent a recurrence.
The Role of Public Perception and Trust
Trust is the currency of healthcare. A 2008 survey found that 12% of adults reported improper disclosure of their medical information, a number that has likely grown with the rise of cyberattacks. How the public views privacy and health research.
Recent statistics reveal a persistent trust gap: while 83% of people trust their own providers, a staggering 58% believe current privacy protections are insufficient to protect their data. This anxiety directly impacts medical progress. Half of all patients worry about researchers seeing their records, even if de-identified, which can hinder participation in clinical trials and slow down vital research.
Consent preferences reflect this deep-seated concern: 38% want detailed information for each study, and 13% refuse to share their data for research at all. Among those requiring explicit consent, 80% want to understand the research purpose before agreeing.
Building trust requires more than just robust security; it demands transparency and patient empowerment. This is where new models like “dynamic consent” come into play, allowing patients to manage their sharing preferences through a digital platform, giving them granular control over how their data is used. At Lifebit, we earn patient confidence by combining robust technical safeguards with clear communication about how our federated technology protects their privacy. Unwrapping Lifebit Data Security. When patients feel confident their data is secure and they are in control, they are more likely to become active partners in advancing medical research.
The Future of Clinical Data Security
The future of healthcare data security is a dynamic landscape of powerful emerging technologies and increasingly sophisticated, well-funded threats. Staying ahead in this high-stakes game requires a shift from a reactive, defensive posture to a proactive, adaptive strategy to protect secure clinical data.
Evolving Challenges and Future Trends
The Double-Edged Sword of Artificial Intelligence: AI is a powerful tool for improving threat detection and automating security responses. However, attackers are also leveraging AI to create more sophisticated and evasive phishing attacks, generate polymorphic malware that constantly changes its signature, and conduct automated reconnaissance on target networks.
Securing AI/ML Models: As AI becomes integral to diagnostics and treatment plans, the models themselves become critical assets. A new frontier in security involves protecting these models from adversarial attacks, such as data poisoning (corrupting training data to cause misdiagnoses) or model inversion (extracting sensitive training data from the model itself), as explored in Secure Healthcare AI with Confidential Computing.
The Uniqueness of Genomic and Multi-omic Data: This type of data presents unparalleled security challenges. It is inherently identifiable, contains information about an individual’s relatives, and is immutable—unlike a password, it cannot be changed if compromised. Protecting this data requires specialized, end-to-end security controls throughout its entire lifecycle.
Cross-Border Data Sharing and Data Sovereignty: Global health research is often slowed by a complex maze of international regulations and data localization laws, which require data to be stored within a specific country’s borders. Navigating these legal frameworks while enabling collaboration is a major challenge.
Escalation of Cyberattack Sophistication: The gap is closing between cybercriminals and nation-state actors, with criminal groups now using highly sophisticated, state-sponsored tools. The rise of hacktivism, or politically motivated attacks, adds another layer of unpredictability, as motivations are not purely financial.
The Quantum Threat: In the coming years, large-scale quantum computers are predicted to become capable of breaking the asymmetric encryption algorithms (like RSA) that protect much of the world’s digital communications. Organizations must begin planning for a transition to post-quantum cryptography (PQC) to protect data with a long-term need for confidentiality.
Strategies for Maintaining Secure Clinical Data
Meeting these future challenges requires smarter, more adaptive, and forward-looking defenses.
Adopting a Proactive Threat Hunting Mindset: Instead of passively waiting for security alerts, threat hunting involves actively searching for signs of compromise within your network. Hunters form hypotheses based on threat intelligence (e.g., “An attacker might be using a specific tool for lateral movement”) and then search through system logs and network traffic for evidence of that behavior.
Implementing a Zero Trust Architecture (ZTA): A Zero Trust mindset discards the old castle-and-moat model of security, assuming that no user or device is inherently trustworthy, regardless of its location. It operates on the principle of “never trust, always verify,” requiring strict authentication for every access request. Key techniques include micro-segmentation to create isolated network zones around critical applications and enforcing least-privilege access at a granular level.
Leveraging Federated Technologies for Collaboration: Federated technologies are the key to overcoming cross-border data sharing challenges. By bringing the analysis to the data, they enable global research collaboration without moving or exposing sensitive information, thus respecting data sovereignty and minimizing privacy risks.
Automating Compliance and Security (DevSecOps): Continuous compliance monitoring uses automated tools to ensure that policies and controls consistently meet evolving regulatory standards. By integrating security into the development lifecycle (“DevSecOps”), organizations can build more secure applications from the ground up and maintain a state of “compliance as code,” as reflected in our Lifebit ISO Certification: Genomic Data Security.
Preparing for the Quantum Future: The transition to quantum-resistant encryption will not happen overnight. Organizations should start by creating an inventory of their cryptographic systems and developing “crypto-agility”—the ability to easily swap out cryptographic algorithms. This will make the eventual migration to PQC standards, once finalized by bodies like NIST, far smoother and more manageable.
Our approach through AI-Enabled Data Governance AI-Enabled Data Governance combines these cutting-edge strategies with the fundamental understanding that we are not just protecting data; we are protecting real people and their futures.
Conclusion
Securing secure clinical data is a continuous journey of adaptation. The landscape is complex, with evolving threats like sophisticated phishing, ransomware, and vulnerabilities from connected devices.
My 15 years in this field have taught me that the best defense is a comprehensive approach. Technology like encryption and access controls must be paired with a strong security culture where every team member understands their role in protecting patient information.
Digitization has revolutionized healthcare, but each advancement introduces new security considerations. This is why solutions like federated data analysis and Secure Data Environments are crucial. They enable powerful research on distributed data without compromising patient privacy by keeping sensitive information secure in its original location.
Trust is the foundation. While 83% of people trust their providers, 58% worry that protections are insufficient. Closing this trust gap is our primary mission. At Lifebit, our federated platform is designed to do just that, enabling collaborative research while ensuring data remains secure, as demonstrated by our ISO certifications and use of cutting-edge technologies.
Future challenges like quantum computing and AI-driven threats are on the horizon, but innovations like Zero Trust architecture and Trusted Research Environments prove we can have both security and scientific progress.
The key is a proactive mindset: constant vigilance, continuous improvement, and an unwavering commitment to patient privacy.
This is what drives us at Lifebit. We believe robust security accelerates research, empowering scientists to focus on what matters most: finding treatments, improving outcomes, and saving lives.

