Clinical Meaning: The 3 Critical Facets
Understanding ‘Clinical Meaning’: More Than Just Medicine
The term clinical meaning refers to the practical importance and relevance of observations, data, or findings, especially in a medical or healthcare context. It’s about whether something has a real, noticeable effect or significance for patients and their care, distinct from just a statistical observation.
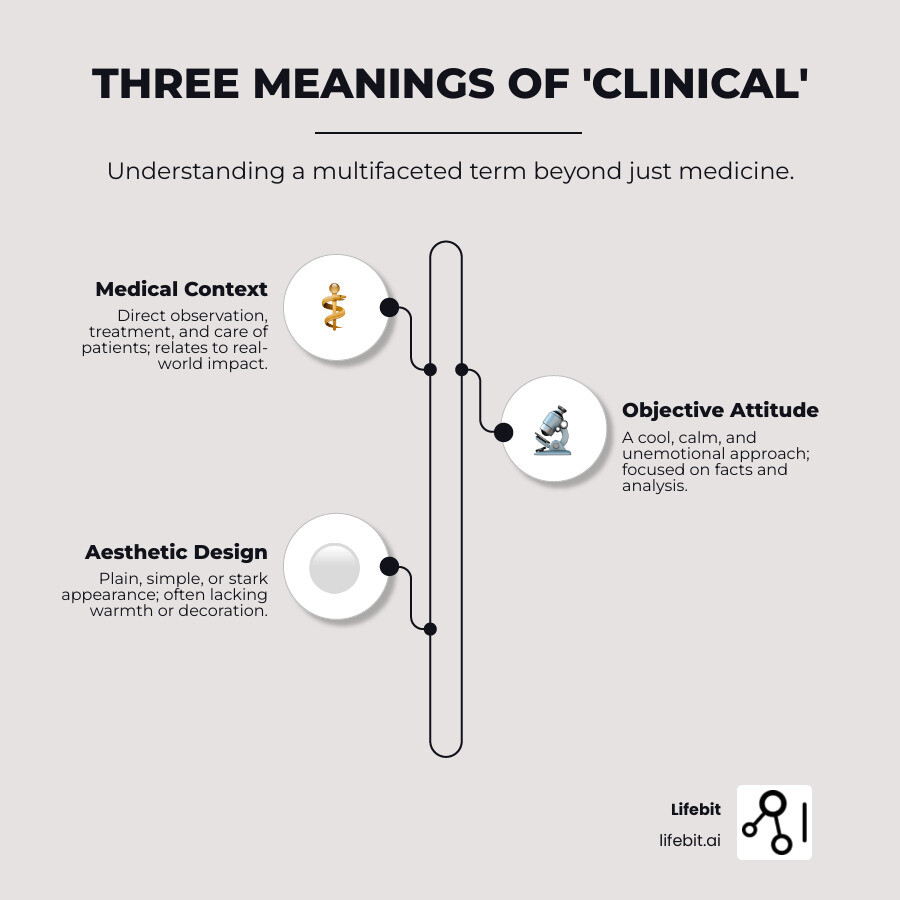
Here’s a quick look at the main ways “clinical” is used:
- Medical/Healthcare Context: This is the most common use. It relates to the direct observation, treatment, or care of patients. Think of “clinical trials” or “clinical symptoms.”
- Objective/Detached Attitude: Sometimes, “clinical” describes a cool, calm, and unemotional approach. It suggests a focus on facts and analysis, without personal feelings.
- Plain/Simple Appearance: Less commonly, it can describe something very plain, simple, or even stark, often lacking warmth or decoration, much like a hospital environment.
You’ve probably heard the word “clinical” many times, especially when talking about healthcare. But this small word carries a lot of weight and can mean different things depending on the situation. From a doctor’s careful observations at a patient’s bedside to the complex data analysis that drives modern medicine, “clinical” has evolved. This guide will help you understand all its layers.
I’m Dr. Maria Chatzou Dunford, CEO and Co-founder of Lifebit. With over 15 years in computational biology and AI, my work has focused on open uping clinical meaning from complex biomedical data, driving precision medicine and drug findy.
The Core Medical Definition: From Bedside to Breakthroughs
When we explore the clinical meaning of something in its most fundamental sense, we’re diving into the heart of what makes medicine truly effective: direct patient care and observation. This is where the word “clinical” finds its strongest roots and most important purpose.
The story begins in ancient Greece, where the word “kline” meant “bed” or “couch.” From this simple beginning, “klinike” emerged to describe the practice of medicine right at the patient’s bedside. It’s a beautiful reminder that real medicine happens where patients are – not just in laboratories or textbooks, but in the actual moments of care and healing.
This bedside medicine approach was revolutionary. Instead of relying purely on theory, physicians began emphasizing what they could observe and learn directly from their patients. This shift toward empirical evidence gathered through direct patient contact became the foundation of modern medical practice.
Common Clinical Phrases and Their Importance
Today’s healthcare language is rich with clinical terms that shape how we understand and deliver medical care. Each phrase carries the weight of that original bedside focus.
Clinical trials represent perhaps the most rigorous application of clinical principles. These carefully designed studies test new treatments on human volunteers to determine safety and effectiveness. The scale is impressive – studies often involve hundreds or thousands of participants. Research shows that around 40% of vaccine candidates in Phase 2 clinical trials prove successful, highlighting both the promise and challenges of medical innovation. The process is deliberately thorough because patient safety comes first. For deeper insights into how these studies work, you can explore our article on emerging trends and technologies in clinical trial design.
Clinical research casts a wider net, encompassing all research conducted with human subjects. While clinical trials test specific interventions, clinical research includes observational studies, surveys, and other methods to understand health and disease patterns.
When doctors make a clinical diagnosis, they’re drawing on that ancient tradition of careful observation. They combine what they see, hear, and feel during examination with laboratory results and patient history. It’s detective work that requires both scientific knowledge and clinical intuition.
Clinical data forms the backbone of modern healthcare decisions. Every patient interaction generates information – from vital signs to treatment responses to long-term outcomes. This data becomes the foundation for understanding what works and what doesn’t in real-world medical practice.
Mental health professionals like clinical psychologists apply these same principles to psychological care, using evidence-based methods to diagnose and treat conditions like clinical depression. The term “clinical” here distinguishes serious, diagnosable conditions from everyday emotional ups and downs.
The Role of Clinical Evidence in Medicine
The National Cancer Institute captures this beautifully in their definition of clinical: it’s about actual observation and treatment of patients, not just theoretical or laboratory study. This distinction matters enormously.
Think about how a new medication travels from laboratory bench to patient bedside. It might show incredible promise in test tubes or animal studies, but its true value only emerges through clinical evidence – real patients, real responses, real outcomes.
The scale of this evidence-gathering is remarkable. In just one week in 2021, clinical laboratories across the country tested over 23,549 specimens for influenza alone. Each test represents a piece of the larger puzzle of understanding disease patterns and treatment effectiveness.
This patient-centered approach to generating evidence drives every major medical breakthrough. Efficacy tests in clinical settings determine whether promising treatments actually help people feel better, live longer, or experience fewer side effects. Vaccine success rates emerge not from computer models but from careful observation of how real people respond to immunization.
The ability to collect, analyze, and interpret vast amounts of clinical data has become crucial for advancing medicine. That’s why we’re passionate about solutions like our de-identified clinical data repository, which enables researchers to access the insights they need while protecting patient privacy.
From those ancient Greek physicians sitting beside their patients’ beds to today’s data-driven treatment decisions, the core principle remains the same: real medicine happens with real patients, generating real evidence that can help the next person who needs care.
Beyond the Hospital: The Other Faces of ‘Clinical’
While its medical meaning is central, the word “clinical” has expanded its reach into other domains, describing attitudes and even aesthetics. These uses often carry a slightly different flavor, moving away from direct patient care to encompass objectivity, detachment, and even a stark simplicity.

‘Clinical’ as an Attitude
When we describe someone’s attitude as “clinical,” we’re highlighting something quite specific. It’s that cool, calm, and collected approach you see when someone needs to handle a tough situation without letting emotions cloud their judgment.
Think about what this really means. A clinical approach involves taking an objective viewpoint – looking at facts and evidence while setting aside personal feelings or biases. It’s about seeing things exactly as they are, not as we might want them to be.
This goes hand-in-hand with dispassionate analysis. When someone analyzes a problem with clinical detachment, they’re focusing purely on logic and reason. Our research shows how a psychiatrist explains in clinical terms, highlighting this analytical approach that prioritizes understanding over emotion.
The most striking example? Picture a surgeon performing a complex operation. Their focus is clinical – precise and unwavering, completely separate from any emotional turmoil an observer might feel. This doesn’t mean they don’t care about their patient. Instead, their professional approach prioritizes the task with complete concentration and skill, maintaining that calm demeanor even under intense pressure.
In professional settings, having a “clinical” attitude is often seen as a strength. It implies competence, professionalism, and the ability to make rational decisions when the stakes are high.
‘Clinical’ in Design and Aesthetics
Here’s where things get interesting. “Clinical” can also describe how something looks and feels, though this meaning is less common. When applied to design, it usually refers to spaces that prioritize function over comfort or visual warmth.
A plain style dominates clinical aesthetics. Think of those simple and unadorned spaces you might find in a hospital – clean lines, minimal clutter, everything designed for utility rather than coziness. The focus is on creating a sterile environment that’s easy to clean and maintain, often featuring lots of white surfaces and bright lighting.
This white and clean look serves an important purpose in medical settings, where hygiene is paramount. But when this aesthetic appears elsewhere, it can sometimes carry an unattractive connotation. You might hear someone say they decided against painting their kitchen white because it would look “too clinical” – meaning it would feel cold or unwelcoming.
The clinical meaning behind this aesthetic choice often reflects a desire for precision and cleanliness, but it can also suggest a lack of personality or warmth when applied outside healthcare settings.
Understanding the Deeper Clinical Meaning in Modern Research
So far, we’ve explored “clinical” in its traditional medical sense and its use to describe a certain attitude or aesthetic. But now, let’s dive into where the term truly gets exciting in today’s world: how we open up clinical meaning from the vast ocean of data. This isn’t just about dictionary definitions anymore. It’s about turning raw information into real understanding that changes lives.
Think of it like this: we have tons of data points, but what do they mean for a patient? What do they mean for finding new treatments? That’s the heart of clinical meaning in modern research. It’s how we transform numbers and observations into actionable insights that genuinely impact patient care and speed up scientific findies.

At Lifebit, we live and breathe this mission. We’re dedicated to helping researchers and healthcare organizations uncover this deeper clinical meaning. Our goal is to connect the dots between data and findy. This helps us deliver precision medicine on a much larger scale. Curious to learn more? Check out our approach to Delivering Precision Medicine at Scale.
How is clinical meaning established from data?
One of the biggest “aha!” moments in data analysis is understanding the difference between statistical significance and clinical meaning. They might sound similar, but they answer very different questions:
- Statistical Significance: This is a technical way of saying: “Is this effect we’re seeing likely real, or just a fluke?” If a drug trial shows a statistically significant improvement, it means the positive change probably wasn’t just random chance. Researchers usually set a threshold (like 5%) for this before they even start the study.
- Clinical Significance: This is the real-world question: “Does this effect actually matter to the patient?” Does it make a noticeable, practical difference in their health, how they feel, or their quality of life? A treatment might look great on paper (statistically significant) but have such a tiny effect that it offers no real clinical meaning to the patient. On the flip side, even a small study showing a huge, practical improvement might be worth investigating further.
Let’s use an example. Imagine a pain relief drug. It might be statistically significant if it reduces pain by a tiny 3%. But honestly, would you notice that? You’d probably prefer a drug that reduces your pain by 80%! Similarly, a drug that cuts stroke risk by 70% for someone at high risk, even with some side effects, has much greater clinical meaning than a super-safe drug that only reduces risk by 20%. It’s all about what truly impacts a person’s life.
So, how do we establish clinical meaning from all that data? We do it by:
- Looking for real-world impact: We focus on outcomes that genuinely matter to patients. Think less pain, better mobility, or a longer, healthier life.
- Measuring patient outcomes: We directly track how treatments affect a patient’s health status.
- Defining meaningful change: We figure out what level of improvement is actually important from a patient’s viewpoint.
A key concept here is the Minimal Clinically Important Difference (MCID). This is the smallest change in an outcome that a patient would identify as important. For example, a statistically significant pain reduction of 0.5 on a 10-point scale may be unnoticeable, while a 2-point reduction might be the MCID—the point where a patient actually feels better. This patient-centric metric ensures that the ‘meaning’ we derive from data is grounded in real-world benefit.
Using Real-World Data in Clinical Research is incredibly helpful here. It gives us the full picture needed to understand true clinical meaning.
Here’s a quick way to see the difference:
| Feature | Statistical Significance | Clinical Significance |
|---|---|---|
| What it answers | Is the observed effect due to chance or the intervention? | Is the observed effect important or meaningful to patients? |
| Focus | Mathematical probability, P-values | Practical importance, patient experience, real-world impact |
| Interpretation | Effect is likely real (not random) | Effect is valuable and makes a noticeable difference |
| Primary Audience | Researchers, statisticians | Clinicians, patients, policymakers |
| Example | Drug reduces blood pressure by 1 mmHg (P<0.05) | Drug reduces stroke risk by 70%, improving life quality |
The importance of clinical meaning for patient outcomes
Understanding clinical meaning is absolutely vital. It shapes patient care and the future of healthcare in many ways:
- Personalized treatment: When we know what truly makes a difference for individual patients, we can tailor treatments just for them. This is the essence of precision medicine. It means giving each person the best possible treatment, based on their unique genes, lifestyle, and health condition.
- Drug findy and development: Drug companies need to know their new medicines don’t just “work” statistically. They need to provide a real, clear benefit to patients. This helps them focus on developing truly impactful therapies.
- Safety surveillance: Once drugs are approved, it’s crucial to keep an eye on their real-world effects. For example, AI-powered safety surveillance can analyze huge amounts of data. This helps us spot any side effects that have clinical meaning for patient safety, quickly.
- Integrating multi-omic data: Today, we have access to so much information. We can look at a person’s genetics (genomics), proteins (proteomics), and even their metabolism (metabolomics). By combining this “multi-omic” data with traditional patient records, we get a much deeper, more complete picture of their health. This is where advanced AI and machine learning really shine. For example, in oncology, a patient’s tumor genomics might show a mutation treatable by a specific drug. However, proteomics (protein analysis) could reveal a resistance pathway, while metabolomics (metabolism analysis) might indicate aggressive growth. Integrating these ‘omic’ layers with clinical data provides a deeper clinical meaning: the patient needs a combination therapy, not just the standard drug. This multi-layered insight is the core of modern precision medicine. Our work in AI for Precision Medicine and our Clinical Genomics Portal for Precision Medicine are perfect examples of how we use these powerful tools.
At Lifebit, our cutting-edge federated AI platform is built for exactly this purpose. It allows secure, real-time access to global biomedical and multi-omic data. We have built-in tools for organizing data, advanced AI/ML analytics, and strong privacy controls. This means large-scale, compliant research and drug safety monitoring are possible for biopharma, governments, and public health groups. Our platform includes components like the Trusted Research Environment (TRE), Trusted Data Lakehouse (TDL), and R.E.A.L. (Real-time Evidence & Analytics Layer). These are designed to deliver insights instantly and provide AI-driven safety surveillance across different data systems. This ensures that the clinical meaning of every single piece of data is fully understood and used.
Frequently Asked Questions about ‘Clinical’
We’ve explored the various facets of “clinical,” from its medical roots to its nuanced uses in describing attitudes and aesthetics. Now, let’s tackle some common questions to solidify our understanding, making sure we’ve got all our bases covered!
What is the difference between clinical research and a clinical trial?
This is a common question, and it’s easier to understand than you might think! Think of it like this: clinical research is the big, wide umbrella that covers all studies involving human participants. Its main goal is to improve human health, whether that’s by understanding diseases better, developing new treatments, or finding smarter ways to detect, diagnose, and prevent illness. This can include simply observing people over time (observational studies) or looking at how diseases spread in populations (epidemiological studies), among many other types of investigations.
Now, a clinical trial is a very specific type of clinical research. It’s an “intervention study,” meaning researchers actively step in and give participants a specific treatment or intervention. This could be a new drug, a vaccine, a medical device, or even a new surgical procedure. Then, they carefully watch and measure the effects. Clinical trials are incredibly structured and follow strict rules to ensure everything is safe and ethical. They are truly the gold standard for testing new medical interventions before they become widely available. So, while every clinical trial is a form of clinical research, not all clinical research is a clinical trial. It’s a bit like saying all squares are rectangles, but not all rectangles are squares! If you’re curious to learn more, our article on The role of clinical trials dives deeper into their crucial importance.
What does it mean to have a ‘clinical’ approach to a problem?
When someone talks about taking a “clinical” approach to a problem, they’re describing a very specific mindset. It means you tackle the issue with a clear head, focusing on facts rather than feelings.
This kind of approach is all about being objective – looking at the situation exactly as it is, without letting personal biases or emotions get in the way. It’s also very data-driven, meaning your decisions and actions are based on solid evidence and information, not just guesses or gut feelings. You’ll seek out all the relevant data and analyze it thoroughly to make the best choice.
Furthermore, a clinical approach means remaining unemotional. You keep a calm, detached demeanor, especially when things get tense or difficult. This allows for clear, rational thinking and effective decision-making. It’s a systematic way of working, where you follow a logical, step-by-step process to understand the problem, find solutions, and put them into action. It’s about making choices based on evidence, not feelings, prioritizing what the data and observations tell you over anecdotes or personal opinions. This kind of precise, analytical thinking is highly valued in fields like medicine, where a doctor must stay focused and sharp to provide the very best care.
What are synonyms and antonyms for ‘clinical’ in its various senses?
The word “clinical” is wonderfully versatile, which means it has different close relatives (synonyms) depending on how you’re using it. And of course, its opposites (antonyms) will shift too!
Here are some ways to think about it:
-
When we talk about ‘clinical’ in its medical sense (meaning related to patients, treatment, or observation), you could use words like:
- Medical
- Patient-focused
- Curative
- Therapeutic
- Diagnostic
- Practical (especially when contrasting it with theoretical lab studies)
-
If ‘clinical’ describes an attitude (objective, detached, unemotional), then good synonyms might be:
- Objective
- Detached
- Impersonal
- Scientific
- Dispassionate
- Analytical
- Unemotional
- Cool
- Calm
- Precise
- Skillful
-
And when ‘clinical’ refers to an aesthetic (plain, simple, stark), you could consider:
- Plain
- Simple
- Stark
- Austere
- Sterile
- Antiseptic
- Unadorned
Now, for the antonyms (the opposites) of “clinical,” these will also change based on the specific meaning you’re trying to contrast:
- Opposite of medical/patient-focused: Theoretical, experimental (if referring to lab-based research that doesn’t involve patients), abstract.
- Opposite of objective/detached: Subjective, emotional, passionate, biased, sympathetic, empathetic, warm, personal.
- Opposite of plain/stark: Ornate, decorative, warm, inviting, cozy, welcoming, personal.
Conclusion: From Definition to Data-Driven Findy
We’ve taken quite a journey with the word “clinical,” haven’t we? From its humble origins at the patient’s bedside in ancient Greece, signifying direct observation and care, to its broader applications describing objective attitudes and minimalist aesthetics, “clinical” has proven to be a surprisingly multifaceted term. Its primary clinical meaning remains firmly rooted in medicine, encompassing everything from clinical trials and diagnoses to the very evidence that underpins our healthcare systems.
But here’s where things get really exciting. In our modern era of big data and advanced biomedical research, the concept of clinical meaning has evolved far beyond simple dictionary definitions. It’s no longer just about understanding the word itself—it’s about the profound implications we can extract from complex, interconnected datasets that span genomics, proteomics, and real-world patient experiences.
The distinction between statistical significance and true clinical meaning has become more critical than ever. We’re living in an age where we can process millions of data points, but the real challenge lies in translating that vast ocean of information into tangible, life-changing benefits for patients. That’s the difference between having data and having wisdom.

This evolution represents both an incredible opportunity and a significant challenge. We have access to unprecedented amounts of biomedical data, but making sense of it all requires sophisticated technology, careful governance, and a deep commitment to patient privacy and security. The goal isn’t just to collect more data—it’s to derive meaningful insights that can genuinely improve human health.
At Lifebit, we understand that open uping the true clinical meaning from complex biomedical and multi-omic data requires more than just powerful computers. It demands a platform that can securely connect researchers across the globe, harmonize data from different sources, and apply advanced AI analytics while maintaining the highest standards of compliance and governance.
Our federated AI platform is designed with this exact purpose in mind. We provide real-time access to global health data, enabling researchers from biopharma companies, government agencies, and public health organizations to collaborate seamlessly. Through our Trusted Research Environment, Trusted Data Lakehouse, and Real-time Evidence & Analytics Layer, we’re helping transform raw data into actionable insights that drive precision medicine, accelerate drug findy, and improve pharmacovigilance.
The future of healthcare lies in this ability to derive profound clinical meaning from complex data ecosystems. Every genomic sequence, every patient outcome, every clinical observation contributes to a deeper understanding of human health. Our mission is to ensure that this wealth of information translates into better treatments, safer drugs, and ultimately, improved patient outcomes worldwide.
Ready to see how we’re changing data into findy? Explore our federated data platform and find how the future of biomedical research is unfolding today.