Advana and Beyond: A Deep Dive into DHA’s Big Data Ecosystem

The Blueprint: Unifying Military Health Data to Save Lives and Dollars
The defense health agency data platform is changing how the U.S. military delivers healthcare to 9.6 million beneficiaries worldwide. Here’s what you need to know:
Key Components:
- MHS Information Platform (MIP) – The largest secondary repository of health data in the DoD, consolidating over 1 petabyte of data from 35+ sources
- MHS GENESIS – The modernized electronic health record system replacing fragmented legacy systems
- Common Data Model – Standardizes health data vocabulary across all systems for seamless interoperability
- Operation Helios – The largest data migration in DHA history, moving 30 years of health records into a unified platform
Primary Goals:
- Enable real-time, data-driven clinical decisions
- Support military readiness through predictive analytics
- Eliminate data silos across 164,000 daily patient encounters
- Prepare infrastructure for AI/ML adoption
- Ensure secure, compliant data governance (HIPAA, FISMA)
For decades, military healthcare relied on disconnected systems—53 inpatient platforms, 140 outpatient systems, and hundreds of business intelligence tools scattered across the globe. This fragmentation meant providers couldn’t access complete patient histories. Service members carried paper records. Critical health data sat trapped in silos while decisions waited.
That era is ending. Through strategic modernization initiatives like the Military Health System Information Platform (MIP) and the deployment of MHS GENESIS, the Defense Health Agency is building a unified, secure, and intelligent data ecosystem. The goal isn’t just better technology—it’s better outcomes. Faster care. Lives saved.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit, where we’ve spent over a decade building federated data platforms that enable secure, real-time analytics across complex healthcare ecosystems. Our work with public sector institutions mirrors many of the challenges the defense health agency data platform addresses—breaking down data silos, enabling AI-ready infrastructure, and ensuring compliance without sacrificing speed or collaboration.

The primary goal driving the Defense Health Agency’s (DHA) data platform change is nothing less than enhancing military readiness, boosting operational effectiveness, and ensuring patient safety. Imagine a world where every service member, veteran, and their family receives seamless, personalized care, no matter where they are or when they need it. This vision is being realized by changing raw data into a strategic, trusted asset.
From Chaos to Clarity: Breaking Down Data Barriers
For too long, the military health system wrestled with data silos – a hidden threat to both care and readiness. Before the current change, the DHA grappled with “a hodgepodge of older, distributed systems” from the 1990s, including 53 instances of inpatient systems and 140 outpatient systems. This fragmentation meant that health authorities and contractors would often stay up late trying to gather and coordinate information from 451 military treatment facilities. This disconnected approach led to inefficiencies, duplicate efforts, and a lack of a comprehensive patient view.
Our experience building federated data platforms for governments and public health agencies in the UK, Canada, Singapore, and across Europe has shown us that this fragmentation isn’t unique to any single system. It’s a common pain point that demands a strategic response.
The modernization mandate for DHA is clear and urgent. The COVID-19 pandemic, for instance, significantly accelerated the need for modernized data platforms in military medicine, highlighting the critical importance of rapid data access for decision-makers. The DHA’s 2023 Strategic Plan outlines a clear path towards an “agile, data-driven, virtual-first, human-centered model of care.” This ambitious plan aims to support wartime skills, clinical currency, medical readiness requirements at a global scale, and deliver value- and outcome-based care.
This strategic plan is also building a crucial foundation for AI and advanced analytics. The DHA is actively preparing its data infrastructure to effectively support and leverage cutting-edge technologies like Artificial Intelligence (AI), Machine Learning (ML), Natural Language Processing (NLP), and Optical Character Recognition (OCR). A modernized data platform, as described by experts, allows decision-makers to work faster and enables AI to augment their work, turning complex data into actionable insights.
The Key Players and Their Roles
A change of this magnitude requires dedicated leadership and specialized teams. At the helm of the DHA is Lt. Gen. Telita Crosland, who serves as the director, overseeing nine medical centers, 36 hospitals, 525 clinics, and 138 dental facilities worldwide, serving 9.6 million beneficiaries. Under her guidance, the DHA’s data strategy is firmly aligned with the broader Department of Defense (DoD) Data Strategy and AI readiness roadmap.
The Enterprise Intelligence and Data Solutions (EIDS) Program Management Office (PMO) plays a pivotal role in this change. EIDS manages the Military Health System Information Platform (MIP), which is the largest secondary repository of health-related data in the DoD. EIDS offers five core capabilities: Legacy Data Consolidation, Workflow Application, Information Portal, Analytics Workbench, and a Data Science Laboratory.
Other key Program Management Offices (PEOs) driving this integration include the Program Executive Office (PEO) for Medical Systems, which is an acquisition organization attached to the DHA. This office is responsible for acquiring and delivering healthcare technology. The DHMSM PMO oversees the deployment and sustainment of MHS GENESIS, while the Joint Operational Medicine Information Systems (JOMIS) PMO develops and sustains IT systems for deployed forces. These PEOs are instrumental in delivering digitally centered health care to warfighters around the world, ensuring that the necessary technologies are in place and functioning effectively.
Inside the Defense Health Agency Data Platform
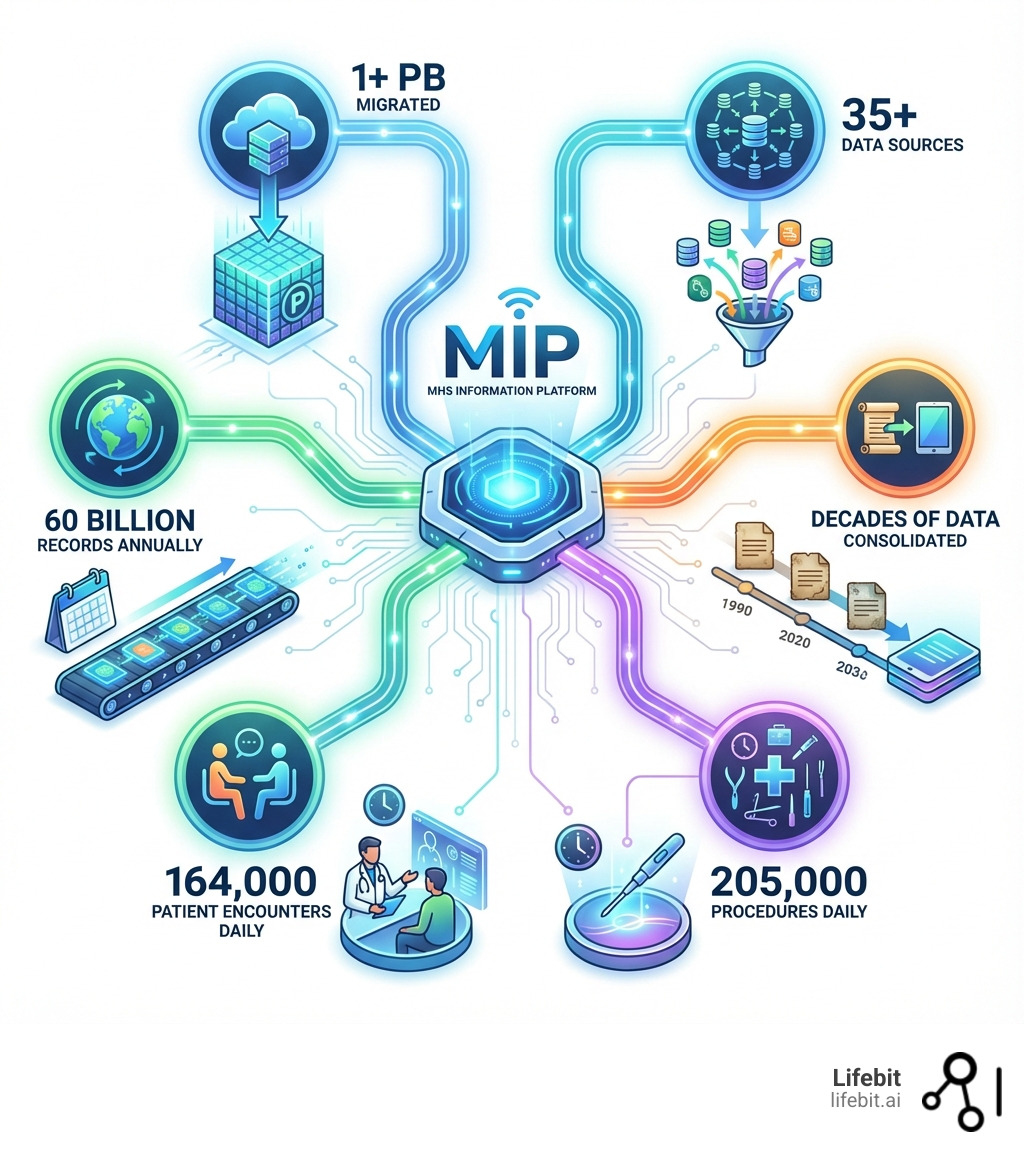
At the heart of the DHA’s data strategy is the Military Health System Information Platform (MIP). This platform represents a monumental leap forward in consolidating and managing vast amounts of healthcare data. The MIP is not just a storage facility; it’s a dynamic system designed to make data accessible and actionable.
The MHS Information Platform (MIP): DHA’s Data Powerhouse
The scale of the MIP is truly staggering. Through a strategic modernization initiative known as Operation Helios, the DHA has completed what’s been called the largest data standardization and migration operation in its history. This involved moving over 1 petabyte of data, which is a mind-boggling one quadrillion bytes, or one million gigabytes. This massive undertaking, executed in carefully planned phases, consolidated data from over 35 disparate sources, including the Armed Forces Health Longitudinal Technology Application (AHLTA), the Composite Health Care System (CHCS), and Essentris®, as well as various ancillary pharmacy, lab, and radiology systems. The process involved complex Extract, Transform, and Load (ETL) pipelines built to handle the unique formats and structures of each legacy system. Hosted on a secure government cloud environment, these pipelines performed intensive data validation and cleansing before loading the information into the MIP, processing an astounding 60 billion records annually.
This isn’t just about moving data; it’s about changing it into a powerful tool for analytics. Previously, analysts would spend up to 80% of their time simply trying to find, access, and merge data from separate repositories like the MHS Data Repository (MDR) and MHS Mart (M2), often with conflicting or incomplete results. Now, the MIP lays the essential groundwork for advanced data analytics capabilities, including big data analysis, Natural Language Processing (NLP), visualizations, and semantic analysis. This means we can move from simply storing information to actively leveraging it for real-world impact, providing seamless data services and decision support for clinicians, patients, beneficiaries, analysts, researchers, and DoD leadership.
By creating a single source of truth, the MIP is designed to eliminate redundant data, reduce operational costs, and significantly improve the provider experience. This consolidation is a critical step towards a more efficient and effective military health system.
Standardizing the Language of Health: The Common Data Model
Imagine trying to understand medical records from different hospitals, each using their own unique terms for the same condition. It would be a nightmare! This is why data standardization is the backbone of interoperability, and why the DHA’s adoption of a Common Data Model (CDM) is so crucial.
The DHA’s Strategic Plan for fiscal years 2023-2028 emphasizes the adoption of a CDM to standardize data definitions. For example, a diagnosis of “obstructive sleep apnea” might have been recorded in one legacy system using an ICD-9 code (327.23), in another as free text in a clinical note, and in MHS GENESIS with an ICD-10 code (G47.33). The OMOP CDM, through standardized vocabularies like SNOMED CT, maps all these variations to a single, unambiguous concept ID. This allows researchers to query for “all patients with obstructive sleep apnea” and receive a complete, accurate cohort without needing to understand the idiosyncrasies of dozens of legacy systems. This vocabulary standardization is vital for enabling seamless care and research. Our experience shows that a standardized vocabulary is foundational for any effective federated data platform, allowing disparate datasets to speak the same language.
The DHA is leveraging the Observational Medical Outcomes Partnership (OMOP) common data model, a widely adopted standard developed through a public-private collaboration. The choice of OMOP was strategic, driven by its robust open-source toolset, strong international community support via the Observational Health Data Sciences and Informatics (OHDSI) community, and its design for enabling large-scale observational research—a key goal for the DHA. This community, boasting over 2,000 collaborators across 74 countries and health records for about 810 million unique patients, provides invaluable guidance and tools.
This standardization effort directly benefits patient care and military readiness by leading to more reliable diagnoses and treatment. It also streamlines research by enabling faster integration of data, even across international partners. Interoperability with other federal agencies, such as the Department of Veterans Affairs (VA) and the Centers for Disease Control and Prevention (CDC), becomes a reality. The VA, in fact, is undergoing a similar initiative, and the close collaboration on CDM mapping is not just about technical alignment; it aims to enable joint research on health issues affecting both populations, such as traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD), and to create a foundation for a truly seamless lifetime health record for service members as they transition to veteran status.
Governance and Security: Building Trust in Every Byte
In the complex world of military healthcare, data isn’t just information; it’s a matter of national security and individual well-being. Therefore, robust governance and uncompromising security are paramount. Our work with governments and public health agencies across the UK, Europe, Canada, and Singapore underscores the critical importance of these pillars in any successful data platform.
Federated Governance: Secure Collaboration Without Centralization
The DHA aims to create a unified, secure, intelligent, and compliant data ecosystem without centralizing data into a single platform. This is a nuanced but powerful approach, embracing a decentralized data model. This strategy is about empowering domain experts and maintaining data sovereignty, allowing data to reside where it is generated while still being accessible for analysis.
The DHA is utilizing a prototype data mesh architecture to modernize its enterprise data infrastructure, supporting domain-driven data ownership and federated governance. This approach aligns perfectly with our philosophy at Lifebit, where our federated AI platform enables secure collaboration across hybrid data ecosystems without ever moving sensitive data. It means data can be exchanged and analyzed securely, preserving privacy and ensuring that control remains with the data owners. This is particularly vital for national defense, where data sovereignty is a non-negotiable requirement.
Protecting Patient Data: Compliance and Security in Action
Protecting patient data is not just a best practice; it’s a legal and ethical imperative. The DHA’s data framework is built to meet the highest standards of regulatory compliance, including the Health Insurance Portability and Accountability Act (HIPAA), and protecting Personally Identifiable Information (PII) and Protected Health Information (PHI). Given the military context, compliance also extends to the Federal Information Security Modernization Act (FISMA) and other stringent DoD cybersecurity requirements.
These protections are implemented through multiple layers:
- Access Controls: Rigorous role-based access control (RBAC) ensures that only authorized personnel can access specific data elements. As seen in the VA’s Health Data and Analytics Platform (HDAP), access is carefully managed and monitored.
- Encryption: Data is encrypted both at rest and in transit, safeguarding it from unauthorized access during storage and transmission.
- Auditing: Comprehensive auditing and logging mechanisms track all data access and activity, providing an immutable record for accountability and compliance checks.
- Continuous Monitoring and Risk Management: The DHA implements robust risk management measures and continuous monitoring to identify and mitigate potential vulnerabilities proactively. The VA’s HDAP, for instance, undergoes regular risk reviews and maintains a FIPS 199 classification of MODERATE, indicating a strong security posture.
Formalizing data stewardship and lifecycle management is also a critical component, with clear roles, responsibilities, and accountability for data ownership established across the enterprise. This holistic approach ensures that every byte of data is handled with the utmost care and integrity.

The Future Is Now: AI, Analytics, and Real-World Impact
The change of the defense health agency data platform isn’t just about organizing existing data; it’s about releaseing its full potential through advanced technologies. The future of military healthcare is being shaped by AI, ML, and sophisticated analytics, turning data into actionable insights that save lives and improve care.
AI in Action: Changing Military Readiness and Patient Care
The DHA is actively preparing its data infrastructure to support and leverage advanced technologies like AI, ML, and NLP. This preparation lays the foundation for future data analytics capabilities, including big data analysis, advanced visualizations, and semantic analysis. Our experience building AI-driven platforms for large-scale biomedical research demonstrates that clean, harmonized data is the fuel for these powerful engines.
- Augmented Decision-Making for Clinicians and Commanders: A modernized data platform allows decision-makers to work faster and enables AI to augment their work. This means clinicians can make more informed diagnoses and treatment plans, while commanders have a clearer common operating picture to make critical operational decisions. This “augmented leadership decision-making” is a direct benefit of the data change.
- Predictive Health: Stopping Problems Before They Start: The ability to leverage predictive analytics means anticipating needs and preventing crises. By analyzing vast datasets, the system can identify patterns and risks, helping clinicians “head off costly medical situations” before they escalate. This proactive approach shifts healthcare from reactive to preventive.
- Operational Triage: Prioritizing Care When Seconds Count: In high-stress environments, seconds count. Integrated medical systems can deliver critical information needed for health and injury concerns, providing predictive analytics and machine teaming to “save lives and improve operational triage.” This ensures that the right care is delivered to the right person at the right time.
- Personalized Medicine: Tailoring Care to Every Service Member: The DHA is shifting from a “one-size-fits-all approach to a personalized healthcare experience” for service members and veterans. Integrating clinical and genomic data, as we do in our platforms, is crucial for personalized medicine and accelerated research translation. This allows for tailoring care to every individual, optimizing outcomes based on their unique health profile.
Real Benefits for Service Members and Veterans
This data change translates into tangible benefits for service members, veterans, and their families:
- Longitudinal Patient Records: Seamless Care Across Deployments: With a unified system, service members no longer have to carry paper medical records. Instead, a “longitudinal patient record” ensures that all relevant data is available to providers, regardless of where the care is delivered—whether in the US, Germany, or Korea. This drastically improves continuity of care across deployments and transitions.
- Proactive Healthcare: From Reactive to Preventive: The ability to use predictive analysis means healthcare can be more proactive, identifying potential issues before they become major problems. This leads to better long-term health outcomes.
- Reduced Paperwork, Improved Safety, Family Health Support: Digitization promises to boost efficiency by reducing the burden of paperwork. With comprehensive data, patient safety is improved through more informed decisions. Furthermore, the goal is to provide a “digital front door” for patients, allowing self-service tasks like prescription refills, appointment scheduling, and secure communication, extending support to families as well.
Challenges and the Road Ahead
Changing an organization as vast and complex as the DHA is no small feat. We’ve seen similar challenges in our work with large-scale government and public health initiatives globally. The road ahead for the defense health agency data platform involves navigating several significant problems.
Overcoming Problems: How DHA Is Building a Resilient Data Platform
- Data Quality: Cleaning Up Decades of Legacy Data: One of the most significant challenges is ensuring data quality. Migrating over 1 petabyte of data, including 30 years of MHS data from legacy systems like the MHS Data Repository (MDR) and MHS Mart (M2), inevitably involves tackling inconsistencies and ensuring accuracy. This process involves more than just mapping fields; it requires sophisticated algorithms for patient de-duplication to create a single “golden record” for each beneficiary who may have been registered multiple times across different facilities over 30 years. Automated data quality rules are run continuously to flag anomalies, such as illogical dates or out-of-range lab values, while teams of data stewards manually curate and correct critical data elements. The accuracy of this historical data is paramount for longitudinal studies and predictive modeling.
- Cultural Shift: Training and Change Management: Technology adoption is as much about people as it is about platforms. There’s a need for a “cultural shift at the speed of relevance for patients,” acknowledging that users vary widely in their readiness for digital tools. To manage this, the DHA has implemented a multi-faceted change management strategy. This includes role-based training modules for clinicians, nurses, administrators, and researchers, ensuring each user group understands how the new tools impact their specific workflows. Furthermore, a network of “clinical champions” and super-users has been established at military treatment facilities worldwide. These individuals receive advanced training and act as on-the-ground peer leaders, advocating for the new system, providing immediate support, and channeling user feedback directly to the program offices to drive iterative improvements.
- Legacy System Integration: Bridging Old and New: The DHA has had to replace a “hodgepodge” of older systems, consolidating disparate networks into a unified system and implementing MHS GENESIS. The challenge lies in seamlessly integrating these new platforms with remaining legacy systems during the transition, ensuring that historical data is accessible and future data flows smoothly without interruption to clinical care. This requires building and maintaining a complex web of interfaces and application programming interfaces (APIs) that can bridge the gap between modern, cloud-native applications and decades-old mainframe systems until the latter can be fully and safely decommissioned.
- User Adoption: Making the Platform Work for Everyone: With over 20,000 users impacted by these changes, minimizing disruption and ensuring that the new platform is intuitive and beneficial is crucial for successful user adoption. The feedback loops created through the clinical champion network are vital for this, allowing for rapid adjustments to user interfaces and workflows based on real-world use.
- Scalability: Preparing for Tomorrow’s Demands: The data infrastructure must be resilient and scalable to handle ever-increasing volumes of data and new technological demands, especially as AI and ML capabilities expand. Our federated cloud-native architectures are designed specifically for this kind of future-proofing, ensuring platforms can grow with demand.
Tackling technical debt and legacy complexity has required a monumental effort. The DHA’s “Desktop to Datacenter” program, for example, consolidated separate Army, Navy, and DHA Medical networks into one unified network with a single help desk. Aligning stakeholders and securing funding has also been critical, involving extensive collaboration across multiple program offices, military hospitals, clinics, and global leaders.
Finally, inter-agency collaboration is breaking down bureaucratic barriers. The close partnership with the VA on data standardization, for instance, ensures interoperability and common approaches. This collaboration is formalized through joint working groups and leverages the Federal Health Information Exchange (HIE) to enable bidirectional data sharing. The ultimate goal is a more integrated federal health ecosystem where a service member’s complete health record is securely and seamlessly available to VA providers the day they transition to veteran status, eliminating dangerous gaps in care and the administrative burden on the individual.
Conclusion: The High Stakes of Military Health Data—And Why DHA’s Platform Matters Now
DHA’s data platform change isn’t just an IT upgrade—it’s a mission-critical shift to smarter, faster, and safer military healthcare. By breaking down silos and building a secure, federated data ecosystem, DHA is saving lives, cutting costs, and powering the next generation of AI-driven care. With advanced technology partners like Lifebit, the right data reaches the right person at the right time—protecting service members, veterans, and their families when it matters most. See how federated data platforms are reshaping federal health.

