Your Guide to Electronic Health Records and Industry Shifts

Why Electronic Health Records Matter in Today’s Healthcare Landscape
Electronic Health Records (EHRs) are the digital systems replacing paper charts, now used by nearly 90% of office-based physicians. These records contain everything from demographics and medical history to lab results and treatment plans. The benefits are clear: patients report better care, providers reduce medical errors (saving an estimated $20 billion annually), and healthcare systems see cost savings and improved data security.
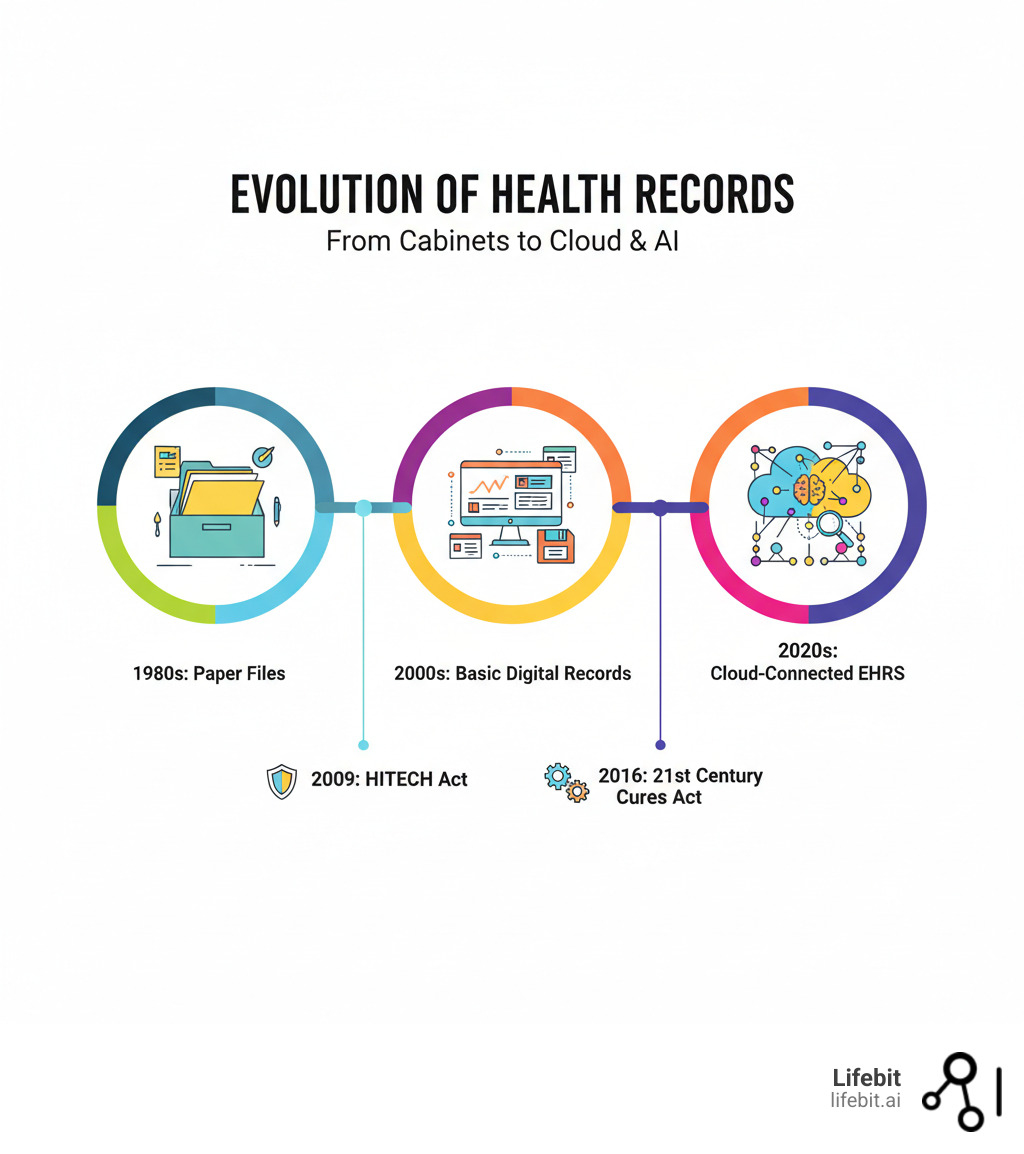
The global EHR market is projected to hit $47 billion by 2027, but this digital revolution, spurred by policies like the HITECH and 21st Century Cures Acts, has created a new challenge. Widespread adoption is done. The real problem now is how to extract value from massive, siloed EHR datasets without compromising privacy or compliance.
For global pharma, public health agencies, and regulatory bodies, the question is no longer if they should use EHRs, but how to unite them across borders and systems to power AI-driven research. This is the problem we solve at Lifebit.
I’m Maria Chatzou Dunford, CEO of Lifebit. We build federated platforms that enable secure analysis of EHRs and other biomedical data without moving it. My background in computational biology and AI has shown me that the right infrastructure can turn fragmented data into actionable evidence for precision medicine and population health.
What are EHRs? The Digital Heartbeat of Modern Healthcare
Electronic Health Records (EHRs) are the digital backbone of modern healthcare, a comprehensive document that follows a patient throughout their entire care journey. Unlike static paper files, EHRs are updated in real-time, capturing everything from diagnoses and medical histories to medications, allergies, and lab results. They are sophisticated systems designed to make healthcare safer, faster, and more coordinated, operating over secure networks to connect providers, labs, and specialists.
EHR vs. EMR: More Than Just a Name Change
Though often used interchangeably, EHR and Electronic Medical Record (EMR) have a key difference. An EMR is a digital version of a paper chart that stays within a single practice. It’s great for internal organization but limited in scope.
An EHR, however, is a comprehensive, longitudinal record that travels with you across different providers and healthcare settings. Imagine you visit your primary care physician for an annual check-up. The notes and vitals from that visit are stored in the practice’s EMR. A month later, you experience chest pains and go to an emergency room across town. Because both your doctor and the hospital use interconnected EHR systems, the ER physician can instantly see your baseline EKG from the check-up, your history of hypertension, and the medications you’re taking. This comprehensive view, impossible with a siloed EMR, allows for a faster, safer diagnosis. An EMR is a record in a practice; an EHR is a record of the patient. This distinction is the foundation of truly connected care. For more details, HealthIT.gov offers a helpful breakdown.
The Core Benefits for Patients and Providers
The widespread adoption of EHRs is driven by measurable benefits.
For patients, the impact is tangible. With instant access to a complete medical history, doctors make better decisions. About 45% of patients report higher quality care since their providers adopted EHRs. This is especially critical for the 60% of American adults with at least one chronic condition. For example, a diabetic patient can use their patient portal to track blood glucose readings over time, share them with their endocrinologist before an appointment, and see how medication adjustments are impacting their A1C levels. This transforms patients from passive recipients of care into active partners in managing their own health. Laws like the HITECH Act and the 21st Century Cures Act also guarantee your right to access your own digital health data, boosting patient engagement and helping to avoid duplicate tests.
For healthcare providers, EHRs streamline administrative tasks like scheduling and billing, freeing up time for patient care. Consider a cancer patient whose care involves an oncologist, a surgeon, a radiologist, and a primary care physician. An EHR provides a single source of truth, allowing the entire team to see the latest pathology reports, review imaging scans, and coordinate treatment plans in real-time, preventing dangerous miscommunications and delays. They also act as a safety net, with automated alerts for potential drug interactions and allergies. Given that medical errors cost the industry around $20 billion annually, this preventative function saves lives and resources. Most importantly, EHRs enable better care coordination by centralizing information so that a patient’s entire care team works from the same complete picture.
Key Components and Functionalities
Modern EHR systems are more than just digital storage. They are sophisticated platforms with several key components.
- Patient Health Information: The core repository for medical histories, demographics, diagnoses, medications, allergies, and test results.
- Order Entry and e-Prescribing: Computerized Physician Order Entry (CPOE) and e-prescribing allow providers to order tests and medications electronically, reducing errors from illegible handwriting and providing instant transmission to labs and pharmacies.
- Clinical Decision Support (CDS): These systems are like a vigilant co-pilot for clinicians. They integrate evidence-based guidelines with patient data to offer real-time recommendations and alerts, such as flagging a new prescription that might interact negatively with a patient’s existing medications, alerting a doctor that a patient is due for a tetanus shot, or presenting treatment protocols for a newly diagnosed condition directly within the workflow.
- Security: Robust encryption, strict role-based access controls, and detailed audit trails ensure only authorized personnel can access sensitive information, tracking every view and modification.
- Patient Portals: These secure interfaces have evolved into comprehensive health management hubs. Patients can not only view their health information but also request prescription refills, schedule appointments online, securely message their provider with non-urgent questions, and complete pre-visit paperwork from home, saving time for both themselves and the clinic staff.
Navigating EHR Adoption: Implementation, Challenges, and Data Quality
Transitioning from paper to a fully digital system is a massive undertaking. The promise of EHRs is real, but achieving it requires careful planning and a clear-eyed view of the challenges.
The Transition to Digital: A Roadmap for Implementation
Successful EHR implementation is a deliberate, multi-stage process. It begins with strategic planning to define an organization’s unique needs and goals. This is followed by careful vendor selection, which involves evaluating vendors based on criteria like ONC (Office of the National Coordinator for Health Information Technology) certification, the availability of specialty-specific modules (e.g., for oncology or pediatrics), user interface (UI) design, and long-term cost models, such as on-premise servers versus cloud-based Software-as-a-Service (SaaS) subscriptions. A critical step is workflow redesign. This means fundamentally rethinking processes. For example, a paper-based workflow might involve a nurse taking vitals on a clipboard and a doctor handwriting notes for later transcription. A redesigned digital workflow has the nurse entering vitals on a tablet at the bedside and the doctor using voice-to-text to document in real-time. Comprehensive staff training is essential to build confidence and drive adoption. The data migration phase, moving historical patient information, must be handled with extreme care to ensure accuracy, security, and proper mapping of data fields from legacy systems. Finally, a phased go-live strategy with robust post-implementation support ensures that the system is continuously optimized based on user feedback. Throughout this journey, transparent change management is key to addressing staff and patient concerns.
Common Problems in EHR Deployment
Even with careful planning, EHR implementations face common problems:
- High Initial Costs: Beyond software licenses, organizations must budget for hardware upgrades (servers, computers, tablets), network infrastructure, extensive staff training programs, IT support personnel, potential productivity losses during the transition period, and fees for customizing the system. The UK’s Guy’s and St Thomas’ NHS Foundation Trust, for example, reported spending £450 million over 15 years on its EHR system.
- Interoperability Issues: Different EHR systems often struggle to communicate, creating data silos that undermine coordinated care and prevent a holistic view of the patient.
- Clinician Burnout: Many physicians spend more time on data entry than with patients, leading to increased cognitive load and dissatisfaction. This has led to a phenomenon known as “pajama time,” where physicians spend hours after work completing their electronic charting at home. The burden of navigating complex interfaces and satisfying documentation requirements can detract from the human element of medicine. Research on EHR-related clinician burden confirms this is a widespread problem.
- Data Security Risks: Centralized digital records are attractive targets for cyberattacks. A single breach can expose the sensitive information of millions of patients, leading to massive regulatory penalties and a loss of public trust.
- Workflow Disruption and User Resistance: If a new system is perceived as less efficient than the old one, it can disrupt care delivery and create significant resistance from staff accustomed to established paper-based workflows.
Data Quality: The Foundation for Research and Reliable EHRs
An EHR is only as valuable as the data within it. For clinical research, quality is paramount—”garbage in, garbage out” is a fundamental truth. Key dimensions of data quality include:
- Accuracy: Information must be correct and free of errors, as a simple mistake in a dosage or diagnosis can have serious consequences for both patient care and research findings.
- Completeness: Missing data is a common problem in EHRs. Understanding why data is missing (e.g., not applicable, not recorded) is critical for valid analysis.
- Timeliness: Real-time data enables real-time insights, which is vital for population health monitoring, early outbreak detection, and AI-driven analytics.
A major challenge in EHR data quality is the distinction between structured and unstructured data. Structured data consists of standardized, discrete fields like drop-down menus and coded entries (e.g., ICD-10 codes). This data is clean and easy to analyze. In contrast, unstructured data is free-form text found in clinical notes and discharge summaries. While it contains rich clinical nuance, it is inherently messy and requires advanced techniques like Natural Language Processing (NLP) to unlock its value. Best practices involve understanding the specific EHR platform, developing clear quality assessment plans, and being transparent about data limitations, as outlined in frameworks for EHR data quality assessment. Federated approaches, which analyze data across multiple systems without moving it, can help address these challenges by enabling research on larger, more diverse datasets, ultimately improving research validity.
The Rules of the Road: Standards, Governance, and Ethics for EHRs
Just as roads need traffic laws, EHRs require standards, governance, and ethics to function safely and effectively. These rules are the foundation for a secure, interconnected healthcare ecosystem.
The Role of Interoperability and Data Standards
An EHR system that can’t communicate with other systems has limited value. Interoperability—the ability of different systems to exchange and make use of data seamlessly—is crucial. For years, “information blocking” by organizations and vendors created data silos. The 21st Century Cures Act (2016) made this practice illegal in the US, mandating data sharing and transparency. Interoperability is often described in three levels: foundational (data can be exchanged), structural (syntax is understood), and semantic (meaning is understood), the ultimate goal for truly connected care.
Technical standards provide the common language for this exchange. Health Level Seven (HL7) develops international standards for transferring health data. More recently, Fast Healthcare Interoperability Resources (FHIR) has emerged as a modern, web-based standard that simplifies data access. FHIR is revolutionary because it uses the same RESTful APIs that power countless smartphone apps, making it far easier for developers to create innovative applications that can securely ‘plug into’ an EHR. This has fostered an ‘app store’ ecosystem for healthcare, enabling tools for everything from patient-facing health trackers to specialized clinical decision support. These standards are central to initiatives like the Promoting Interoperability Programs, which incentivize the meaningful use of EHRs.
Clinical Coding Systems in EHRs: From ICD to SNOMED CT
If standards are the grammar, clinical coding systems are the vocabulary. They translate complex medical language into standardized codes for billing, research, and public health reporting. The most prominent system is the ICD (International Classification of Diseases) from the World Health Organization, used globally for classifying diseases. You can find an overview of the ICD system here. For more detailed clinical documentation, systems like SNOMED CT (Systematized Nomenclature of Medicine—Clinical Terms) offer greater granularity. Beyond these, other critical coding systems create a comprehensive data language. Logical Observation Identifiers Names and Codes (LOINC) is used to standardize laboratory tests, while RxNorm provides normalized names for clinical drugs. Together, these systems allow an EHR to precisely document that a patient with a diagnosis (ICD-10) had a specific lab result (LOINC) and was prescribed a particular medication (RxNorm).
The Bigger Picture: Work Information and Social Determinants of Health
Health is shaped by factors outside the clinic, known as Social Determinants of Health (SDOH). Employment is a key factor. Capturing work-related information—or Occupational Data for Health (ODH)—in EHRs provides critical context. For example, knowing a patient’s occupation can help identify work-related conditions like occupational asthma. Similarly, capturing broader SDOH data like housing status or transportation access can transform care. If an EHR notes a patient lives in a ‘food desert,’ the system could trigger a referral to a nutritionist. If a patient frequently misses appointments and their record indicates ‘unreliable transportation,’ a care manager could be alerted to arrange a ride service. Aggregated ODH and SDOH data can also reveal health patterns in specific industries or communities, guiding public health interventions. Standardizing the collection of this data, as detailed in resources on capturing work information in EHRs, creates a more complete picture of patient health.
Legal and Ethical Guardrails: Protecting Patient Data

Protecting digital patient data is more critical than ever. In the US, HIPAA (Health Insurance Portability and Accountability Act) sets national standards. It is divided into the Privacy Rule, which governs who can access and share protected health information (PHI), and the Security Rule, which dictates the technical safeguards required to protect it. You can find details at HHS.gov. In Europe, GDPR (General Data Protection Regulation) imposes even stricter requirements, enshrining principles like data minimisation (collecting only necessary data) and the ‘right to be forgotten.’
Beyond regulations, ethics demand meaningful patient consent and clear data governance. To enable research while protecting privacy, organizations use techniques like anonymization (removing all identifiers) and pseudonymization (replacing identifiers with artificial ones). However, concerns about data exposure from centralized servers have fueled resistance in regions like the UK and Germany. This is why federated approaches—where data remains in its local, secure environment and only insights travel—are gaining traction as a superior, privacy-preserving alternative for cross-border research.
The Future is Now: AI, Federated Learning, and the Next Generation of EHRs
The EHR systems of the past two decades were built to store data. The next generation is about using that data to predict, prevent, and personalize healthcare.
AI and Machine Learning: Open uping Insights from EHR Data
The vast amount of information in EHRs is a treasure trove for AI and machine learning. These technologies are finally open uping its potential.
- Predictive analytics can scan EHR data to forecast disease outbreaks, identify high-risk patients, and predict treatment responses. For example, a model running in a hospital’s EHR can continuously monitor dozens of variables in a patient’s record. By detecting subtle changes in heart rate, respiratory rate, and lab results, it can identify patients at high risk of developing sepsis hours before a human might notice the pattern, enabling life-saving early intervention.
- Personalized medicine becomes a reality as AI combines EHR data with genomics to help clinicians tailor treatments to a patient’s unique biology.
- Population health management benefits from AI’s ability to spot health trends across millions of records, enabling more effective public health interventions.
- Natural Language Processing (NLP) extracts critical information from unstructured clinical notes. NLP algorithms can scan through millions of discharge summaries and pathology reports to extract details about disease severity, patient-reported symptoms, and lifestyle factors, converting this rich narrative text into analyzable data for research and clinical decision support.
Privacy-Preserving Analysis: How Federated Learning is Changing the Game
Powerful AI needs massive amounts of data, creating a fundamental tension with patient privacy. Moving sensitive EHR data to a central location for analysis is risky and often illegal. Federated learning offers a groundbreaking solution.
Instead of bringing data to the AI, federated learning brings the AI to the data. The process works in steps: First, a central server sends a machine learning model to each participating institution. Second, each hospital trains the model on its own private EHR data, locally and behind its own firewall. Third, the hospital sends only the updated model parameters—the mathematical ‘learnings’—back to the server. Finally, the server aggregates these anonymous updates to create a more intelligent global model. This iterative process builds a powerful model without any patient data ever being moved or exposed.
This approach solves several problems at once:
- Patient data never leaves the institution, dramatically reducing security risks and ensuring compliance with GDPR and HIPAA.
- Researchers gain access to diverse global datasets without the logistical and legal problems of data transfers.
- Data silos are broken down, enabling large-scale collaborative research that was previously impossible.
The seminal paper on federated learning established this transformative approach. At Lifebit, our platform is built on these principles, enabling secure analysis of global biomedical data across distributed environments.
The Outlook for EHRs: Towards a Connected and Intelligent Health Ecosystem
The future of EHRs is connected and intelligent. Imagine a digital twin—a virtual health avatar built from your EHR, genomic, and lifestyle data. A physician could test several potential chemotherapy regimens on this digital twin to predict which one will have the highest efficacy and fewest side effects, before administering a single dose to the actual patient. This would revolutionize personalized medicine. Real-time public health surveillance using EHR data can detect outbreaks in their earliest stages.
EHRs are also integrating data from wearables and mobile health apps, creating a continuous, holistic view of health. The challenge lies in integrating this stream of real-world data (heart rate, sleep patterns, activity levels) with the episodic, clinical data in the EHR. A successful integration would create a dynamic view of a patient’s health, enabling earlier detection of abnormalities. This evolution empowers patients, making them active partners in their care. Initiatives like the European Health Data Space (EHDS) are creating a unified ecosystem for secure data sharing. This is all part of Healthcare 4.0—a predictive, preventative, personalized, and participatory system with EHRs at its core. The global EHR market is expected to reach $47 billion by 2027, reflecting a shift toward a smarter, more connected, and more effective healthcare system.
Frequently Asked Questions about EHRs
Here are straightforward answers to common questions about EHR systems.
How secure is my data in an EHR system?
Modern EHRs offer far better security than paper records. They use multiple layers of protection, including encryption to make data unreadable to unauthorized users, strict access controls to ensure only relevant staff can view your information, and audit trails that log every interaction with your record. In the US, the HIPAA Security Rule mandates these protections, while Europe’s GDPR imposes even stricter requirements. While no system is 100% foolproof, EHRs are designed with robust, layered security to keep your sensitive information safe.
Can I access my own electronic health record?
Yes. Your health information belongs to you. Laws like the HITECH Act in the US and GDPR in Europe strengthen your right to access your digital health data. Most providers offer secure patient portals where you can view lab results, check your medical history, and communicate with your care team. If a portal isn’t available, you have the legal right to formally request your records. This transparency is essential for you to be an engaged and informed participant in your own healthcare.
Why do doctors spend so much time on the computer during appointments?
It can be frustrating when a doctor seems more focused on their screen than on you. They are performing essential clinical documentation, entering your symptoms, diagnoses, and treatment plans into the EHR. This structured data entry is necessary to create an accurate, comprehensive record that supports quality care, meets regulatory requirements, and ensures other providers have a complete picture of your health.
While this process can contribute to clinician burden, the benefits of structured data are significant. It enables safety alerts for allergies or drug interactions, allows for long-term tracking of health metrics, and facilitates better care coordination. The industry is actively developing solutions like voice recognition and improved interfaces to reduce this burden and improve the patient-doctor interaction.
Conclusion: From Digital Records to Predictive Intelligence
The evolution of EHRs from digital filing cabinets to dynamic intelligence platforms is reshaping healthcare. Today, they are the foundation for coordinated care, clinical decision support, and cutting-edge research. The real excitement, however, is what’s happening now.
The integration of AI with privacy-preserving techniques like federated learning is solving the critical challenge of our time: how to harness the collective intelligence in global health data without compromising patient privacy. By analyzing data where it resides, we can open up powerful insights while keeping sensitive information secure.
At Lifebit, our federated AI platform is built to deliver on this promise. We turn fragmented EHRs and other biomedical data scattered across institutions into actionable, real-time intelligence. Through our Trusted Research Environment (TRE), Trusted Data Lakehouse (TDL), and R.E.A.L. (Real-time Evidence & Analytics Layer), we enable biopharma, governments, and public health organizations to conduct large-scale, compliant research without ever moving patient data.
The future of healthcare is one where EHRs help predict what’s next and guide us toward better outcomes. It’s a future where data silos fall, insights flow securely, and every patient benefits from collective knowledge. We are not just watching this future unfold—we are building it.
If you’re ready to open up the full potential of your health data with the highest standards of privacy, we can show you what’s possible. Learn how Lifebit enables secure, real-time research on global biomedical data and join us in building a healthier, more connected future.

