How to Integrate Electronic Health Records Without Losing Your Mind

Why Electronic Health Records Integration Is the Make-or-Break Decision for Modern Healthcare
Electronic health records integration connects disparate health data systems—EHRs, practice management software, lab systems, and registries—so that patient information flows seamlessly across providers, researchers, and care teams. In the current landscape, where healthcare data is generated at an exponential rate, the ability to synthesize this information into a coherent, actionable patient profile is the primary differentiator between high-performing health systems and those struggling with administrative bloat.
Here’s what you need to know about the current state of integration:
- EHR integration enables real-time access to complete patient histories across multiple providers and locations, effectively ending the era of the “fragmented patient.”
- Key benefits: Faster diagnosis through comprehensive data visibility, reduced medical errors (particularly in prescribing), significantly better patient outcomes, and streamlined clinical workflows that reduce physician burnout.
- Main challenges: Implementation costs remain high ($15,000–$70,000 per provider), alongside staff resistance, data migration risks, and the complex landscape of privacy compliance.
- Critical standards: HL7 FHIR, USCDI, and HIPAA-compliant architectures ensure interoperability and security, moving the industry away from proprietary, closed-loop systems.
- Integration types: EHR-integrated registries (real-time, single-system), EHR-linked registries (periodic extracts, multi-system), and federated access models that allow for analysis without data movement.
Healthcare organizations face a stark reality: EHR transitions are “remarkably expensive, laborious, personnel-devouring, and time-consuming.” The historical context is important here; the HITECH Act of 2009 incentivized the adoption of digital records, but it didn’t necessarily mandate that those records talk to each other. This led to a decade of “digital silos.” In 2023 alone, more than 540 organizations and 112 million individuals experienced healthcare data breaches, often occurring at the vulnerable points where data is transferred between unoptimized systems. Meanwhile, the interoperability issues that have plagued the industry for decades continue to hinder patient safety, block access to complete clinical data, and slow research that could save lives.
Yet integration is no longer optional. Three companies now control 87% of the U.S. hospital EHR market, and regulatory mandates like the 21st Century Cures Act are pushing the industry toward open APIs and standardized data exchange. For global pharma, public sector agencies, and research institutions managing siloed datasets across borders, the stakes are even higher: slow data onboarding, poor data quality, and compliance bottlenecks can derail drug discovery, pharmacovigilance, and population health initiatives worth billions. The shift from “Meaningful Use” to “Promoting Interoperability” reflects a fundamental change in how the government and private sector view health data—not as a static record, but as a dynamic asset.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit, where we’ve spent over a decade solving electronic health records integration challenges for pharmaceutical companies and public health organizations through federated AI platforms that enable secure, real-time analytics across diverse biomedical datasets. This guide distills what we’ve learned—and what the evidence shows—about doing EHR integration right.
EHR vs. EMR: Why Electronic Health Records Integration Changes Everything
To master integration, we first have to clear up the “alphabet soup” of healthcare tech. While many people use the terms interchangeably, there is a massive functional difference between an Electronic Medical Record (EMR) and an Electronic Health Record (EHR). Understanding this distinction is critical for any organization planning a digital transformation strategy.
An EMR is essentially a digital version of a paper chart in a clinician’s office. It contains the medical and treatment history of the patients in one practice. While EMRs were a significant step up from paper, they are provider-specific and rarely travel outside that single practice. If a patient needs to see a specialist or goes to the emergency room, the EMR data usually stays behind, requiring the patient to manually relay their history or the new provider to request faxes.
In contrast, an EHR is designed to be shareable across multiple healthcare stakeholders. It is built to go beyond standard clinical data collected in a provider’s office and is inclusive of a broader view of a patient’s care. It follows the patient to the specialist, the hospital, the nursing home, and even across state lines.
When we talk about electronic health records integration, we are moving beyond just “digitizing records.” We are building a nervous system for healthcare data. True integration allows your Electronic Medical Record Systems to talk to billing software, pharmacy management systems, and external research registries. Without this connectivity, your data remains in a silo—and in modern medicine, a data silo is a patient safety risk.
The Four Levels of Interoperability
To understand the depth of integration, we must look at the four levels of interoperability defined by HIMSS:
- Foundational Interoperability: This is the basic ability of one system to send data and another to receive it. It does not require the receiving system to interpret the data.
- Structural Interoperability: This defines the format, syntax, and organization of data exchange. It ensures that data movement can be interpreted at the field level.
- Semantic Interoperability: This is the “holy grail.” It ensures that two or more systems can exchange information and use the information that has been exchanged. It relies on common coding systems like SNOMED CT and LOINC.
- Organizational Interoperability: This includes the legal, social, and policy frameworks that allow data to flow seamlessly between different organizations.
The Core Benefits of Electronic Health Records Integration
Why go through the headache of connecting these systems? Because the “old way”—manual browser logins, faxing records, and re-entering patient info—is killing efficiency and morale.
- Eased Clinical Workflow: Integration automates patient queries. Instead of a doctor manually searching a state prescription monitoring program (like MassPAT), the data is pulled directly into the EHR dashboard in real-time. This reduces “click fatigue,” a leading cause of physician burnout.
- Improved Patient Outcomes: With a 360-degree view of patient history, including medications prescribed by other providers, the risk of adverse drug events drops significantly. It also enables better chronic disease management by tracking lab trends across different facilities.
- Employee Efficiency: When systems “talk,” staff don’t have to spend hours on data entry or tracking down lab results. Advanced systems can even auto-sync every 30 seconds, ensuring that the most recent data is always available for decision-making.
- Return on Investment (ROI): While the upfront cost is high, integrated systems reduce administrative overhead, improve billing accuracy by capturing all billable events automatically, and enable participation in value-based care programs that reward quality outcomes.
- Precision Medicine and Research: Integrated EHRs provide the high-quality, longitudinal data necessary for genomic research and personalized treatment plans. By linking clinical data with genomic data, researchers can identify which patients will respond best to specific therapies.
| Feature | EMR (Standard) | EHR (Integrated) |
|---|---|---|
| Data Portability | Limited to one practice | Shareable across all authorized providers |
| Patient Access | Often requires manual request | Real-time via patient portals/APIs |
| Interoperability | Low/Proprietary | High (via FHIR/HL7) |
| Research Utility | Low (Siloed) | High (Supports registries & trials) |
| Clinical Decision Support | Basic/Internal | Advanced/Cross-institutional |
Solving the $70,000 Problem: Overcoming Implementation Challenges
Let’s address the elephant in the room: cost. Research shows that EHR implementation can cost practices between $15,000 – $70,000 per provider. For a large health system with hundreds of providers, this represents a multi-million dollar investment. That is a staggering figure for any organization, especially when you factor in the “J-curve” of satisfaction—a phenomenon where productivity and morale often dip for 6 to 18 months after a new system goes live before the benefits are fully realized.
Beyond the price tag, we frequently see these roadblocks:
- Staff Adoption Resistance: Not everyone is a tech wizard. Variations in tech familiarity can lead to “workarounds” that compromise data integrity. Clinicians often feel that the EHR becomes a “data entry tool” rather than a clinical aid. Overcoming this requires a culture shift where the EHR is seen as a tool for patient safety.
- Data Migration Nightmares: Moving data from a Legacy EHR Warehouse to FHIR or between different vendors is fraught with risk. Inconsistent formats, coding, or terminology can lead to “messy data” that hinders clinical decision-making. For example, if one system records a lab result in mg/dL and another in mmol/L without proper mapping, the results could be misinterpreted.
- System Outages and Downtime: Outages are common during transitions. Organizations must develop clear downtime procedures to ensure care doesn’t stop when the screen goes dark. This includes maintaining paper backups and ensuring that critical patient data is cached locally.
- Vendor Lock-in: Some legacy vendors make it intentionally difficult to export data, charging high fees for API access or using proprietary formats that don’t play well with others. This is why the 21st Century Cures Act’s “Information Blocking” rules are so critical.
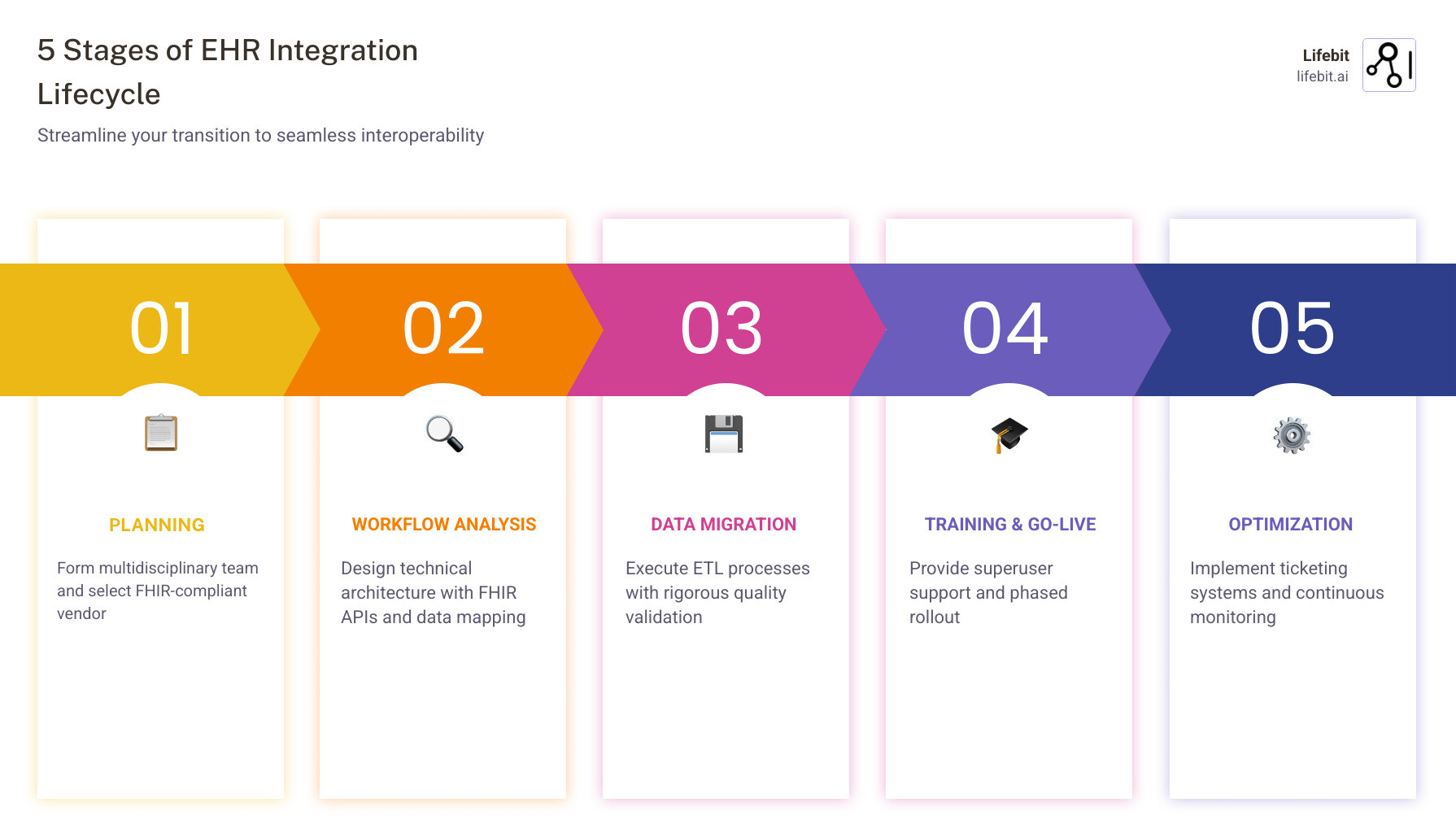
To minimize these risks, we recommend a phased approach rather than a “Big Bang” rollout for large organizations. This allows for troubleshooting in a smaller environment before scaling. The use of “superusers”—internal staff who are trained early and can provide at-the-elbow support to their peers—is the single most effective strategy for ensuring high adoption rates. For more on managing these complex datasets, see our guide on Harmonizing Disparate Electronic Health Records.
Protecting Patient Data During Electronic Health Records Integration
Data privacy isn’t just a legal requirement; it’s a matter of trust. In 2023, more than 540 organizations and 112 million individuals experienced healthcare data breaches. When you integrate systems, you create more “doors” for potential attackers. Each API endpoint and data exchange node is a potential vulnerability if not properly secured.
To stay compliant and secure:
- HIPAA Compliance: Ensure every vendor in your integration chain is fully HIPAA-compliant and has signed a Business Associate Agreement (BAA).
- Encryption: Data must be encrypted both at rest (on the server) and in transit (as it moves between systems). Using TLS 1.3 for data in motion is the current gold standard.
- Two-Factor Authentication (2FA): This is increasingly required, especially for e-prescribing controlled substances (EPCS). It prevents unauthorized access even if a clinician’s credentials are stolen.
- Audit Logs: Maintain detailed logs of who accessed what data and when. This is not only a HIPAA requirement but also a critical tool for forensic analysis in the event of a breach.
- Federated Models: At Lifebit, we advocate for federated governance. Instead of moving sensitive patient data into one giant, vulnerable “honey pot” database, a federated approach allows researchers to analyze data where it resides. The data never leaves the secure environment of the hospital or clinic; only the analytical insights are shared. This significantly reduces the risk of a massive breach and simplifies compliance with international laws like GDPR.
Learn more about building a HIPAA-Compliant EMR to protect your practice.
Technical Architectures: From Legacy Warehouses to FHIR
The “secret sauce” of modern electronic health records integration is the HL7 FHIR (Fast Healthcare Interoperability Resources) standard. For decades, the industry relied on HL7 v2, which was like sending a massive, unformatted telegram. If you wanted to update a patient’s phone number, you had to send the entire medical record. FHIR changed the game by using modern web technologies (RESTful APIs) to allow systems to exchange specific “resources”—like a single immunization record, a medication list, or a diagnostic report.
The 21st Century Cures Act has accelerated this by mandating that patients have access to their electronic health information via “certified” APIs. This is why you can now see your health records on your smartphone’s health app. We are moving away from proprietary “walled gardens” toward a United Medical Language System (UMLS) where data can be understood by any system it enters.
The Role of SMART on FHIR
SMART (Substitutable Medical Applications, Reusable Technologies) on FHIR is a platform that allows third-party developers to create apps that run across different EHR systems. Think of it as the “App Store” for healthcare. If a researcher develops a new tool for predicting sepsis, they can build it as a SMART on FHIR app, and it can be integrated into Epic, Cerner, or any other FHIR-compliant EHR without needing custom code for each one. This modularity is the future of healthcare innovation.
Common Data Types and Quality Considerations
For integration to be useful, the data must be high quality. “Garbage in, garbage out” applies here more than anywhere else. If a clinician enters “Type 2 Diabetes” in a free-text note but doesn’t use the proper ICD-10 code, that data might be invisible to an automated registry. Key data types commonly extracted and shared include:
- Patient Identifiers: Name, DOB, and Master Patient Index (MPI) numbers. MPIs are critical for preventing duplicate records, which can lead to dangerous situations like a patient having two different allergy lists.
- Demographics: Essential for Population Health Management, though often missing social determinants of health (SDOH) like income, education, or housing stability. Modern integration efforts are increasingly focused on capturing this “Z-code” data.
- Clinical Data: Diagnoses (using ICD-10-CM), Medications (RxNorm), and Lab Results (LOINC). These standardized terminologies ensure that “Aspirin” in one system is recognized as “Aspirin” in another.
- Social and Behavioral Data: Increasingly important for identifying at-risk populations and addressing health inequities.
- Unstructured Data: This includes doctor’s notes, discharge summaries, and imaging reports. While harder to integrate, this data contains 80% of the clinical value.
U.S. Core Data for Interoperability (USCDI) provides a standardized set of health data classes that must be interoperable nationwide. Ensuring your integration maps to these standards is critical for long-term scalability and regulatory compliance.
Real-World Impact: Registries, Research, and Population Health
The true power of electronic health records integration shines in research and public health. By connecting EHRs to Patient Registries, we can track outcomes for thousands of patients in real-time, identifying trends that would be invisible in a single practice.
There are two primary ways this happens:
- EHR-Integrated Registries: These live within the clinical workflow. A doctor enters data once, and it populates both the patient chart and the registry. This is ideal for chronic disease management, like the New York City Population Health Registry. It provides real-time decision support, alerting the doctor if a patient is due for a screening based on registry data.
- EHR-Linked Registries: These are often used for large-scale research. Data is periodically extracted (using ETL – Extract, Transform, Load processes) from the EHR and moved to a separate system for analysis. While not real-time, these registries allow for massive datasets to be analyzed for long-term trends, such as the efficacy of a new drug across diverse populations.
Integration also powers EHR Claims Integration, allowing researchers to combine clinical data (what happened in the doctor’s office) with insurance claims (what was paid for). This provides a full picture of the “patient journey” and the true cost of care, which is essential for the transition to value-based reimbursement models.
Case Study: The Power of Federated Analytics
In a traditional model, if a pharmaceutical company wanted to study a rare disease, they would have to request data from 50 different hospitals, wait for legal approvals, and then try to merge 50 different datasets. This process can take years.
With Lifebit’s federated approach, the researcher sends the algorithm to the data. The hospitals keep their data behind their own firewalls. The algorithm runs locally at each site, and only the aggregated results are sent back to the researcher. This has been used to accelerate COVID-19 research and is now being applied to oncology and rare diseases, cutting data access times from years to weeks.
Future Trends in Interoperability and AI
We are entering the era of “Next-Generation Phenotyping.” By using AI and Natural Language Processing (NLP), we can now extract insights from the unstructured data in EHRs—like the free-text notes doctors write during visits. This allows us to identify patients for clinical trials with 80% more accuracy than using structured codes alone. For example, an NLP algorithm can identify “early-stage cognitive decline” mentioned in a note even if the formal diagnosis code for Alzheimer’s hasn’t been applied yet.
At Lifebit, we are taking this a step further with federated access. By enabling secure, real-time access to global biomedical and multi-omic data (genomics + EHR), we allow biopharma and governments to run Scientific research on EHR-driven phenotyping without ever moving the data. This is the future of Electronic Health Records Programs: secure, compliant, and lightning-fast. We are moving toward a world where a patient’s genomic profile is a standard part of their EHR, allowing for truly personalized medicine at scale.
Frequently Asked Questions about EHR Integration
What is the difference between EHR-integrated and EHR-linked registries?
EHR-integrated registries are part of the clinician’s daily software, allowing for real-time data capture and decision support during a visit. They reduce double-entry and provide immediate feedback. EHR-linked registries are separate systems that receive data via periodic extracts (like a monthly “data dump”) and are typically used for long-term research, public health reporting, or post-market surveillance of drugs.
How much does EHR integration typically cost per provider?
Implementation costs generally range from $15,000 to $70,000 per provider. This includes software licensing, hardware upgrades, data migration, and the temporary loss of productivity during the training phase. Ongoing maintenance costs typically run about 20% of the initial investment annually.
How can practices overcome staff resistance to new software?
The best approach is to involve clinicians early in the selection process, provide “at-the-elbow” support from internal superusers, and clearly communicate how the new system will eventually save them time and improve patient safety. Gamification and phased rollouts can also help reduce the initial stress of the transition.
What is the role of APIs in EHR integration?
APIs (Application Programming Interfaces) act as the bridge between different software systems. In healthcare, FHIR-based APIs allow different EHRs to “talk” to each other and to third-party apps. They are the technical foundation that makes modern interoperability possible, moving away from the old method of manual file transfers.
Is EHR integration required by law?
While not strictly “required” for every small practice, the 21st Century Cures Act makes “information blocking” illegal and mandates the use of standardized APIs. Furthermore, participation in many federal reimbursement programs (like MIPS and MACRA) requires the use of certified, integrated EHR technology.
How does integration improve patient safety?
Integration reduces errors by providing a single, accurate source of truth. It prevents duplicate testing, alerts clinicians to dangerous drug-drug interactions based on prescriptions from other providers, and ensures that critical information (like allergies) is available in emergency situations regardless of where the patient usually receives care.
Conclusion
Integrating electronic health records is a massive undertaking, but it is the only way to build a healthcare system that is truly efficient, secure, and data-driven. From reducing medication errors to accelerating life-saving research, the benefits far outweigh the temporary growing pains of implementation. We are moving away from a world of fragmented, siloed data and toward a future of seamless, patient-centered care.
At Lifebit, we specialize in making this complex process seamless. Our federated AI platform provides the “glue” that connects disparate datasets—whether they are in London, New York, or Singapore—ensuring that researchers and clinicians have the insights they need without compromising patient privacy. By solving the technical and regulatory challenges of data sharing, we enable the next generation of medical breakthroughs.
Stop struggling with data silos. Start unlocking the power of your health data.
Learn how Lifebit enables secure, real-time access to global biomedical data

