Recruitment Revolution: Optimizing Patient Enrollment for Clinical Trials

Cut Enrollment Delays That Cost $8M/Day: 5 Proven Ways to Find Patients 2x Faster
Introduction: The $8M/Day Problem of Lagging Clinical Trial Recruitment
How to improve patient recruitment in clinical trials is a critical question, as recruitment challenges are the top cause of study delays and budget overruns. When enrollment goals aren’t met, patients miss opportunities for investigational therapies and drug development stalls.
Quick Answer: Core Strategies to Improve Patient Recruitment
- Design patient-centric trials to minimize burden.
- Expand awareness through trusted channels like physicians and patient groups.
- Empower clinical sites by reducing administrative tasks and improving communication.
- Leverage data and technology to identify eligible patients faster.
- Build reusable infrastructure for cross-trial recruitment.
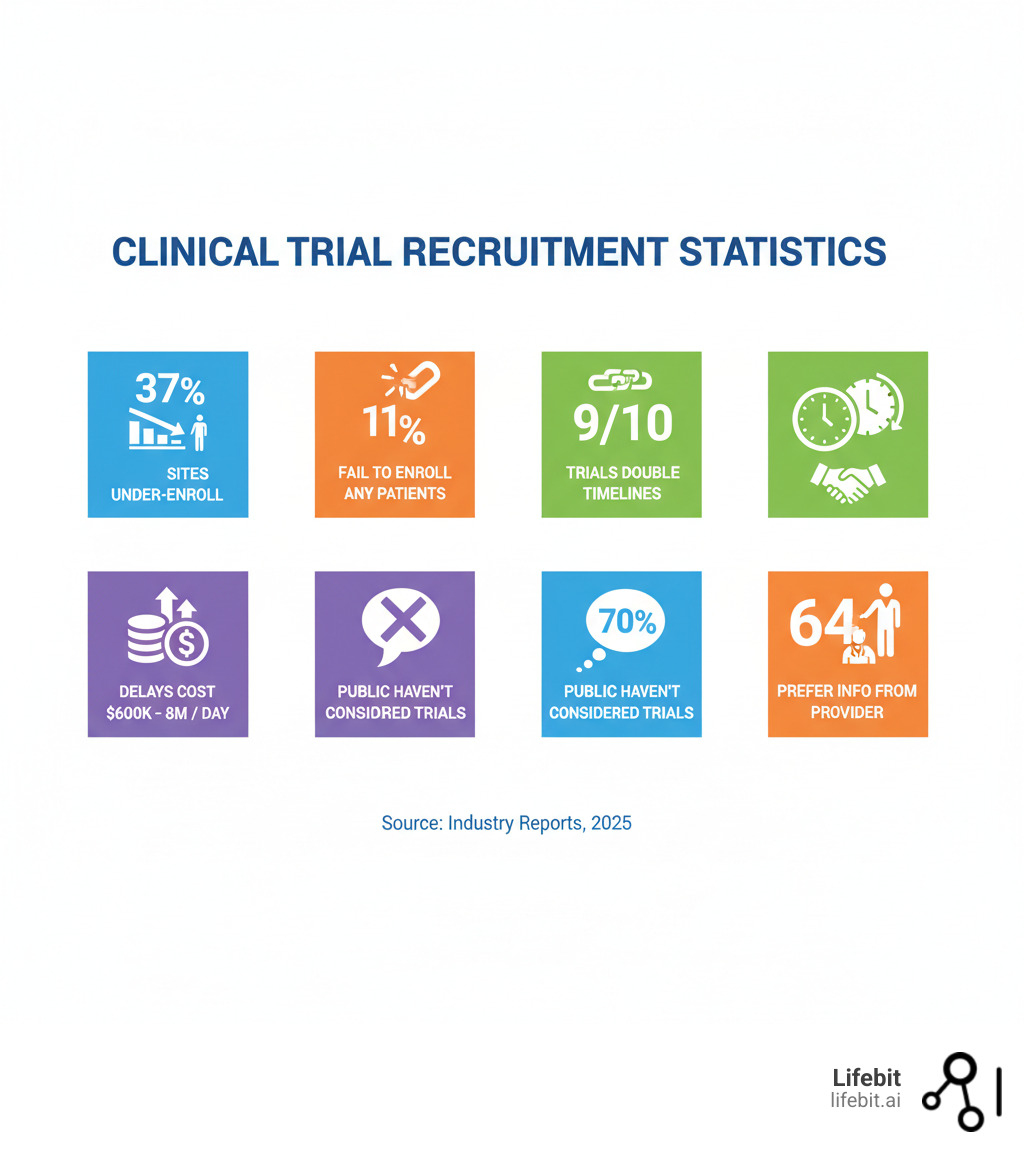
The financial impact is staggering, with delays costing sponsors up to $8 million per day in opportunity costs. The operational reality is sobering: 37% of research sites under-enroll, 11% fail to enroll a single patient, and 9 out of 10 successful trials only meet goals by doubling their original timelines.
These challenges persist, worsened by the COVID-19 pandemic. A staggering 70% of the public haven’t considered trials as a treatment option, and 40% doubt they could find a suitable study. The pandemic amplified these issues, forcing widespread site closures, creating patient reluctance to visit healthcare facilities, and shifting clinical research staff to frontline care. This disruption not only halted many ongoing trials but also created a significant backlog, intensifying the pressure on recruitment for new and restarted studies. The crisis did, however, accelerate the adoption of decentralized and digital methods, highlighting the urgent need for more resilient recruitment models.
Root causes include low patient awareness, strict criteria, overburdened sites, and fragmented data systems. However, modern tools like federated data platforms and digital recruitment strategies offer solutions. As Maria Chatzou Dunford, CEO of Lifebit, I’ve spent over 15 years using genomics, AI, and health-tech to solve these problems. This guide explores practical strategies for sponsors, CROs, and sites to turn recruitment from a bottleneck into a competitive advantage using secure, federated access to real-world data.
Key terms for how to improve patient recruitment in clinical trials:
- AI clinical trial recruitment
- clinical trial patient recruitment companies
- clinical trial patient support
Patient-Centricity: Design Trials People Actually Want to Join
Many trials struggle to enroll because they are designed for scientific rigor, not for the people participating in them. Patient centricity means redesigning trials around the patient’s needs, preferences, and real-world experiences. Understanding what motivates and deters patients is the first step in how to improve patient recruitment in clinical trials.
Understanding What Motivates and Deters Patients
Patient motivations are often altruistic: 36% join to improve the lives of others, and 26% want to advance medicine. Others seek to improve their own condition (15%) or access the best treatment option (8%). Monetary compensation is a primary driver for only 5%.
However, patients weigh factors carefully. 83% consider potential risks and benefits very important, while 75% prioritize understanding the study’s purpose. The top deterrents are concerns about side effects (40%) and risks to overall health (33%).
The trial burden is a major silent deterrent, including time off work, travel, and the sheer volume of appointments. Many potential participants cannot make the schedule work with their lives.

A staggering 70% of the public haven’t considered clinical trials with their doctor, revealing a massive awareness gap. Encouragingly, 94% of volunteers would participate in a clinical trial again. A positive experience turns patients into advocates, linking retention directly to recruitment. Providing clear information, answering questions thoroughly, and offering ethical compensation all boost enrollment and retention. Comprehensive reviews summarize these motivators and barriers across diseases; see Improving Participant Recruitment in Clinical Trials for evidence and practical recommendations.
A sponsor’s guide on how to improve patient recruitment in clinical trials through better design
The best recruitment strategy is designing the trial with patients in mind from the start.
Simplify protocols. Complex protocols deter participation. Limit procedures, reduce visit frequency, and simplify eligibility criteria wherever possible by engaging with patients and advocacy groups early.
Use decentralized trial elements. Incorporating decentralized clinical trial (DCT) components can dramatically lower the participation barrier. This goes beyond simple telemedicine. Consider using electronic patient-reported outcomes (ePRO) collected via smartphone apps, shipping study drugs directly to patients’ homes, deploying wearable sensors to gather continuous physiological data, and utilizing local labs for blood draws. These elements reduce the need for frequent site visits, minimize time off work, and make trials accessible to patients in remote or underserved areas.
Improve the informed consent process. The consent process is often a major hurdle, filled with dense, technical language. Redesign consent forms for health literacy, using plain language, infographics, and clear summaries. Implement electronic consent (eConsent), which can incorporate videos and interactive quizzes to ensure comprehension. The process should be a conversation, not a transaction. Allowing patients ample time to review materials with their families and ask questions is critical. Having trained study coordinators, rather than the treating physician, lead the consent discussion can also help mitigate any perceived pressure to participate.
Create patient feedback loops. Use advisory boards or surveys to integrate patient input throughout the trial. This helps you identify and fix problems before they impact enrollment.
Offer ethical compensation. It’s crucial to distinguish between reimbursement and undue inducement. Patients should be fully reimbursed for all trial-related expenses, such as travel, parking, meals, and childcare. Furthermore, providing a stipend for their time and effort is an ethical way to acknowledge their contribution. This is not payment for risk, but compensation for their commitment. A clear, transparent compensation schedule, approved by an ethics committee, removes financial barriers that can exclude lower-income individuals and helps ensure a more diverse and representative study population.
Expanding Your Reach: Modern Strategies for Trial Awareness
A patient-friendly trial is useless if no one knows it exists. The awareness gap is a major hurdle, with 70% of people never considering trials when discussing treatment with their doctor. To succeed, you must reach patients where they are.
Leveraging the Most Trusted Recruitment Channels
Not all recruitment channels are equal. Understanding which ones deliver quality participants is key to how to improve patient recruitment in clinical trials.
- Primary care physicians (PCPs): 58% of the public learn about trials here; 64% prefer to hear about trials from their doctor.
- Nurses at primary care: 19% of the public learn about trials from nurses.
- Online clinical trial registries: 40% of people use these to learn about trials. Examples include ClinicalTrials.gov and the EU Clinical Trials Register.
- Search engines: 30% use search to find trials.
- Online peer communities: 74% express interest in discussing trials in these forums.
- Pharmaceutical company channels: 19% learn from pharma; 25% prefer receiving info via a company website.
The data is clear: Healthcare providers are the most trusted source. A full 64% of patients prefer hearing about trials from their doctor. However, engaging physicians effectively is a major challenge, as they are often overwhelmed with clinical duties and may lack awareness of available trials. To overcome this, sponsors must equip them with tools that fit seamlessly into their workflow. This includes providing ‘lunch and learn’ educational sessions, one-page trial summaries with clear eligibility criteria, and simple digital referral portals. Building relationships with key opinion leaders and practice managers can also champion trial awareness within a healthcare system.
Digital channels are also crucial: 40% of people use online registries and 30% use search engines to learn about trials. Your trial must be visible in these searches. Personal referrals are also highly effective, with one trial seeing a 100% completion rate from referred participants. A multi-channel approach combining personal outreach with targeted digital efforts delivers the best ROI.
Tapping into Digital and Community-Based Recruitment
The digital landscape has transformed patient recruitment, allowing us to reach potential participants globally, especially in connected regions like Europe, the UK, USA, Canada, and Singapore.

Social media advertising allows for precision targeting to reach specific patient populations. Platforms like Facebook and Instagram are effective for reaching broad consumer demographics based on interests and behaviors, while LinkedIn can be used for professional groups or specific disease indications. Effective campaigns often use a mix of ad formats, including video testimonials from past participants, informative infographics, and clear calls-to-action leading to a pre-screener. A/B testing ad copy, imagery, and targeting parameters is essential to optimize spend and maximize the quality of leads.
Optimize for Search Engine Visibility (SEO). Since 30% of people use search engines to find trials, a strong online presence is non-negotiable. Your dedicated recruitment website must be optimized for search engines. This involves researching and using keywords that patients are likely to search for (e.g., ‘lung cancer clinical trial in New York’, ‘new treatments for Crohn’s disease’). Creating high-quality blog content that answers common patient questions can also attract organic traffic and establish your trial as a credible resource.
Online peer communities are powerful, with 74% of people interested in discussing trials in these spaces. Sharing information here can build trust.
Patient advocacy groups are trusted bridges to patient communities. Partnering with them early provides invaluable insights and facilitates outreach to diverse populations.
A dedicated recruitment website should be a central hub with clear trial information, plain-language eligibility criteria, searchable site locations, and a digital pre-screening form.
Digital pre-screening forms help patients self-assess eligibility and generate de-identified data that can refine future recruitment strategies. Platforms like Lifebit’s federated AI platform enable secure, privacy-conscious data analysis, making it possible to learn from recruitment data across trials.
The bottom line is to be present in the right places, with the right message, delivered by trusted voices.
How to Improve Patient Recruitment in Clinical Trials by Empowering Your Sites
Clinical trial sites are the frontline of recruitment but are often hampered by pressure and administrative burdens that hurt enrollment. When sites are overwhelmed, patient care and how to improve patient recruitment in clinical trials both suffer.
The reality is stark: 37% of research sites under-enroll, and many struggle with staff shortages, making administrative tasks overwhelming. This burden doesn’t just slow enrollment—it can prevent sites from identifying eligible patients altogether. Empowering sites with clear protocols, smart technology, and streamlined communication is essential for success.
Streamlining Site Operations and Communication
Removing friction from daily workflows is the most effective way to improve recruitment.
Clear protocols are foundational. Ambiguous or complex protocols waste site staff’s time. Write concise, easy-to-understand protocols with straightforward eligibility criteria to enable coordinators to move quickly.
Technology can reduce administrative burden. Site coordinators spend countless hours on manual tasks like data entry, scheduling, and reporting. Technology can automate many of these workflows. For example, systems that automatically import patient referrals from various sources (digital ads, physician portals) into a central site database eliminate manual data entry and reduce errors. Digital pre-screeners allow patients to self-assess basic eligibility, providing sites with a pre-qualified list of candidates and saving valuable staff time on initial phone screens.
Centralized communication platforms solve frustrating challenges like patient slot allocation. A single platform connecting sponsors and sites eliminates confusion and delays enrollment, ensuring eligible patients don’t lose interest.

Provide Performance-Based Support and Incentives. Recognize and reward high-performing sites. This can include financial bonuses for meeting or exceeding enrollment targets. However, non-financial support is equally important. Provide dedicated recruitment specialists to struggling sites, offer additional marketing budgets for local outreach, or create a forum for site coordinators to share best practices. This collaborative approach fosters a partnership rather than a purely transactional relationship, motivating sites to stay engaged.
Invest in team training. Formal training in recruitment improves team confidence and effectiveness. One study showed a trained team met its enrollment target within twelve months. Weekly check-ins provide continuous improvement opportunities.
Offer flexible scheduling. To accommodate participants’ work or school schedules, sites should offer extended hours, send clear appointment reminders, and adapt to patient needs.
Enhancing Patient Identification and Pre-Screening
Robust pre-screening processes make the entire recruitment funnel more efficient.
Implement a formal pre-screening process. A systematic approach to reviewing patient data ensures consistency. Tracking I/E criteria failures provides strategic insights into recruitment obstacles.
Leverage existing site databases. Since research shows 72% of participants are already patients at the trial site, mining Electronic Health Records (EHRs) is a high-yield strategy. This requires more than a simple keyword search. Modern approaches use Natural Language Processing (NLP) to scan unstructured data like physician’s notes, pathology reports, and discharge summaries to find eligible patients who might be missed by queries on structured data alone. Implementing these tools allows sites to proactively identify and contact potential candidates within their own patient population, a far more efficient method than waiting for referrals.
Streamline slot request management. Delays in approving slot requests risk losing interested candidates. A unified patient enrollment management platform allows sponsors to quickly review and approve requests, preventing administrative bottlenecks that cause patients to fall through the cracks.
The Data-Driven Advantage: Using Technology to Accelerate Enrollment
Intuition isn’t enough for modern clinical trial recruitment. Understanding how to improve patient recruitment in clinical trials requires moving beyond guesses and embracing data-driven decisions. Technology can transform recruitment from a challenge into a strategic advantage.
Using data to understand how to improve patient recruitment in clinical trials
Systematically collecting and analyzing recruitment data leads to smarter decisions.
Track recruitment channel performance to understand which strategies deliver the best ROI and allocate resources effectively. This reveals which channels produce not just leads, but participants who complete the trial.
Examine the entire enrollment funnel to identify drop-off points. A typical funnel includes stages like Awareness (ad impressions, site visits), Consideration (pre-screener completion), Pre-Screening (passed/failed), Consent (signed/declined), and Enrollment. By tracking conversion rates between each stage, you can pinpoint bottlenecks. For example, a high drop-off after pre-screener completion might indicate the full eligibility criteria are too restrictive or the site follow-up is too slow. Collecting de-identified data on screen failure reasons (e.g., ‘failed lab value X’, ‘comorbidity Y’) provides actionable insights to amend protocols or refine targeting in future trials.
Use predictive analytics for site selection. Site selection is often based on past relationships and stated interest, but data offers a more objective approach. By analyzing aggregated, de-identified real-world data (RWD)—such as insurance claims, EMR data, and demographic information—sponsors can model patient populations around potential sites. These models can predict the number of eligible patients within a certain radius of a hospital, forecast enrollment rates based on historical performance in similar trials, and identify promising sites in new regions, avoiding the costly mistake of activating sites with no realistic path to enrollment.
Harmonize data from past trials to create a compounding knowledge base. Capturing these lessons makes each new trial more efficient than the last.

Building a Sustainable Recruitment Engine with Technology
Technology enables us to act on data insights at scale, making recruitment faster and more sustainable.
Use patient enrollment management platforms as a single source of truth for sponsors and sites. These systems streamline cohort management and slot requests, eliminating the confusion of scattered spreadsheets and emails.
Enable cross-trial recruitment. Instead of starting from scratch with every trial, build a reusable patient registry or ‘talent pool.’ This involves creating a database of individuals who have previously expressed interest in research or participated in a trial and have consented to be contacted about future opportunities. For sponsors with a portfolio of studies in one therapeutic area (e.g., oncology, immunology), this is a goldmine. It allows for rapid identification and outreach to a warm, engaged audience, dramatically improving recruitment ROI and shortening timelines, a strategy that is especially critical for rare disease trials where every potential participant is precious.
Leverage federated data access. Lifebit’s federated AI platform provides secure, real-time access to diverse data (clinical, genomic, RWD) without moving sensitive patient information. This ensures compliance with GDPR, HIPAA, and other privacy regulations across regions like Europe, the UK, USA, and Canada.
The platform’s built-in harmonization capabilities allow for analysis of disparate data sources without lengthy ETL processes, while advanced AI and machine learning analytics accelerate the patient identification process.
Automate manual workflows like appointment reminders and referral management. This frees up site staff to focus on high-value patient engagement, improving both efficiency and the patient experience.
By integrating these solutions, you build a sustainable recruitment infrastructure that becomes more effective with each study.
Frequently Asked Questions about Patient Recruitment
What are the biggest challenges in clinical trial patient recruitment?
The biggest challenges are interconnected. A major one is the awareness gap, with 70% of the public never having considered trials as a treatment option. Even for those who are aware, 40% lack confidence in finding a suitable study.
Strict inclusion/exclusion criteria limit the eligible patient pool. At the same time, sites are overburdened, with 37% under-enrolling and 11% failing to enroll anyone. This administrative strain directly hinders recruitment.
Patient concerns about side effects (40%) and health risks (33%), plus practical burdens like travel and time off work, are also significant barriers that prevent participation.
What is the most effective way to find patients for a clinical trial?
There is no single magic bullet; the most effective method is a thoughtful, multi-channel strategy. The foundation is engaging trusted healthcare providers, as 64% of patients prefer to hear about trials from their doctor.
This should be combined with targeted digital campaigns to reach patients online where they are actively searching for health information. Social media and search engines are powerful tools for this.
Partnerships with patient advocacy groups are also crucial, as they provide a trusted connection to engaged patient communities, especially for rare diseases.
Patient-centric design is key. An appealing trial with minimal burden transforms recruitment from a hard sell into a genuine opportunity that patients want to pursue.
How can technology solve patient recruitment challenges?
Technology is essential for modernizing recruitment. It solves challenges by centralizing data and workflows through patient enrollment management platforms, creating a single source of truth for sponsors and sites and eliminating administrative chaos.
Automation handles repetitive tasks like appointment reminders and digital pre-screening, freeing site staff to focus on patient engagement and care.
Technology also provides real-time insights and analytics, showing enrollment funnel drop-offs and channel ROI. This visibility allows for dynamic adjustments to strategy.
Our federated AI platform enables secure analysis of real-world patient data across global healthcare systems (Europe, UK, USA, Canada, Singapore, etc.) without moving data. This allows for faster identification of eligible patients while ensuring strict privacy compliance.
Finally, technology helps build reusable infrastructure, like patient databases, making recruitment a sustainable, efficient engine rather than a trial-by-trial scramble.
Conclusion: Unify Your Strategy to Revolutionize Recruitment
Improving how to improve patient recruitment in clinical trials requires a unified approach that combines patient-first design, strategic awareness, empowered sites, and data-driven insights. By designing patient-centric protocols, expanding reach through trusted channels, and empowering sites with streamlined workflows, we address the core challenges of enrollment.
The true revolution, however, comes from data and technology. The ability to analyze channels, identify bottlenecks, and use federated platforms to match patients with trials is a game-changer for clinical research.
Lifebit’s federated AI platform is designed to overcome data fragmentation, enabling compliant, real-time patient identification across global networks like Europe, the UK, the USA, Canada, and Singapore. Our platform delivers the insights and secure collaboration needed to accelerate the entire research lifecycle, from identifying eligible patients faster to reducing site burden.
The future of recruitment is not about choosing one strategy, but about integrating them all to build a sustainable, scalable engine that serves patients. Let’s commit to innovation and collaboration to transform recruitment from a persistent bottleneck into a powerful engine for medical progress.

