Trial and Error No More with Real World Evidence
Real-World Evidence Clinical Trials: Cut Trial Costs and Get Answers Faster
Real-world evidence clinical trials are fundamentally changing the paradigm of how drugs are developed, approved, and monitored throughout their lifecycle. For decades, the pharmaceutical industry relied almost exclusively on traditional randomized controlled trials (RCTs). While RCTs remain the gold standard for establishing efficacy under tightly controlled conditions, they often fail to represent the complexity of the general population. RWE trials address this by analyzing data from routine healthcare delivery—electronic health records (EHRs), insurance claims, patient registries, and increasingly, wearable devices and mobile health apps.
This approach captures how treatments perform in diverse, real-world populations characterized by multiple health conditions (comorbidities), varied treatment patterns, and different healthcare settings. By moving beyond the “sterile” environment of a research clinic, RWE provides a more accurate picture of a drug’s safety and effectiveness in the hands of everyday patients and physicians.
Key facts about real-world evidence clinical trials:
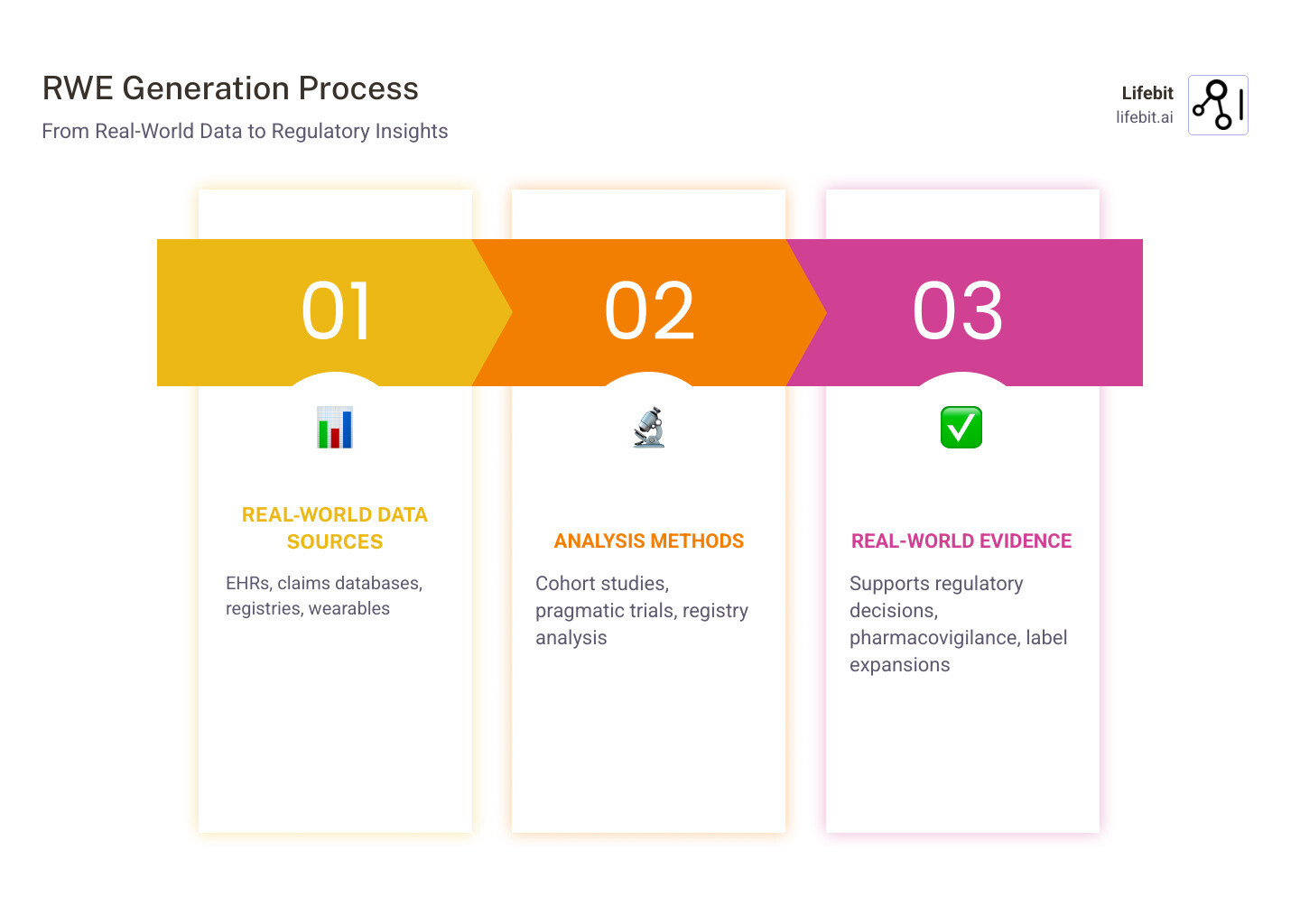
- RWD (Real-World Data): This is the raw material. It includes patient health status and/or the delivery of health care routinely collected from a variety of sources, including EHRs, medical claims and billing data, product and disease registries, and patient-generated data from in-home-use settings.
- RWE (Real-World Evidence): This is the clinical evidence regarding the usage and potential benefits or risks of a medical product derived from the analysis of RWD. It is the result of applying rigorous statistical methods to messy, real-world datasets.
- Regulatory acceptance: The landscape has shifted dramatically. Between January 2019 and June 2021, the FDA approved 85% (116 of 136) of new drug applications (NDAs) and biologics license applications (BLAs) that were backed by some form of real-world evidence.
- Global growth: The volume of RWE studies is exploding. 2021 saw the highest number of RWE trials on record, and 2024 is projected to surpass 336 major trials, reflecting a compound annual growth rate that outpaces traditional research.
- Geographic leaders: China currently accounts for 29.9% of global RWE trials, driven by massive centralized data initiatives. They are followed by Italy (10.1%), Germany (9.8%), and the US (9.2%), though the US remains the leader in regulatory framework development.
The shift toward RWE addresses critical gaps in traditional clinical research. RCTs often exclude patients with comorbidities, pregnant women, children, and elderly populations due to safety concerns or the need for a “clean” signal. However, these groups are the very people who will eventually use the drug. Real-world evidence fills this gap by providing data on how therapies work across the full spectrum of patients who will actually use them.
Furthermore, the sheer volume of data available through RWD allows for the detection of rare adverse events that might not appear in a trial of 3,000 people but become evident when looking at a population of 3,000,000. This makes RWE an indispensable tool for post-market surveillance and long-term safety monitoring.
As Maria Chatzou Dunford, CEO and Co-founder of Lifebit with over 15 years of experience in computational biology and health-tech, I’ve seen how real-world evidence clinical trials are accelerating precision medicine. By enabling secure, federated analysis of genomic and biomedical data across global healthcare systems, we can now identify patient subpopulations that respond best to specific therapies, moving us closer to the goal of truly personalized healthcare. This guide will walk you through how RWE is reshaping drug development, from regulatory frameworks to practical implementation strategies.
Real-World Evidence Clinical Trials: Stop Waiting Years for Drug Results
Strategic Advantages Over Traditional Randomized Controlled Trials
The “gold standard” status of RCTs is being challenged not because they are wrong, but because they are incomplete. In the modern era of drug development, relying solely on RCTs is like trying to understand a forest by looking at a single tree in a greenhouse. We see four major areas where RWE offers a decisive competitive edge:
1. Cost-Effectiveness and Resource Optimization
By using existing real-world data, sponsors can avoid the multi-million dollar costs associated with site activation, manual data entry, and the physical infrastructure of traditional trial sites. Traditional Phase III trials can cost between $11,000 and $40,000 per patient enrolled. When you consider that a large cardiovascular trial might require 10,000 patients, the costs become astronomical. RWE-based approaches can significantly reduce these expenses by tapping into data that has already been collected for clinical or billing purposes. This allows smaller biotech companies to compete with “Big Pharma” by conducting high-quality research on a fraction of the budget.
2. Recruitment Speed and Patient Identification
One of the biggest bottlenecks in drug development is clinical trial patient recruitment. Statistics show that 80% of clinical trials fail to meet their initial enrollment deadlines, and 11% of sites fail to enroll a single patient. RWD allows researchers to identify eligible patients in seconds rather than months. By querying EHR databases, sponsors can find exactly where the patients are located and which physicians are treating them. This data-driven approach to site selection and recruitment can save sponsors months of delays and millions in operational costs, ensuring that life-saving drugs reach the market faster.
3. Pragmatic Trial Designs
Pragmatic clinical trials (PCTs) are a subset of RWE trials designed to show the real-world effectiveness of the intervention in broad patient groups. These trials occur during routine care, meaning the results reflect actual clinical practice. Physicians and patients do not need to alter their behavior significantly, which produces evidence that is immediately applicable to treatment decisions. This is particularly useful for comparative effectiveness research—determining which of two already-approved drugs works better for a specific type of patient.
4. Synthetic Control Arms (SCAs)
For rare diseases or certain cancers where a placebo arm is unethical or practically impossible, we can use RWD to create a “virtual” or “synthetic” control group. This involves using historical data from EHRs or registries to simulate the control group, allowing every patient in the actual trial to receive the experimental treatment. This approach has already been accepted by regulators in several oncology approvals, such as the FDA’s approval of Blincyto (blinatumomab), where a single-arm trial was compared against a historical control group derived from RWD.
Research into adverse event detection shows that RWE is far superior at catching rare side effects that only appear once a drug is used by millions of people. For example, the rare heart-related side effects of certain COX-2 inhibitors were only fully understood through large-scale observational RWE studies after the drugs had been on the market for years.
Using Real-World Evidence Clinical Trials for Rare Diseases
Rare disease research is perhaps the greatest beneficiary of the RWE revolution. When only a few hundred people globally have a condition, traditional randomization is nearly impossible. Recruiting enough patients for a statistically powered RCT can take years, and many rare disease trials fail simply because they cannot enroll sufficient participants.
RWE allows us to use real-world data for clinical evidence generation in oncology and other specialized fields to expand drug labels to new populations. A landmark example is the expansion of the breast cancer drug Ibrance (palbociclib) to include male patients. Because male breast cancer is so rare, a traditional RCT was not feasible. Instead, the manufacturer used EHR data and insurance claims to prove the drug’s effectiveness in men, leading to a successful label expansion. Historical control arms built from registry data and EHRs have enabled single-arm trials to gain regulatory approval, giving patients access to therapies that would otherwise remain unavailable for years.
Navigating the Global Regulatory Landscape
Regulators in our core regions—the US, UK, Canada, and Europe—have moved from skepticism to active support. They recognize that the traditional model of drug development is becoming unsustainable and that RWE is essential for maintaining a robust pipeline of new therapies.
How the FDA’s Framework Cut Approval Times
The FDA’s framework for evaluating RWE, mandated by the 21st Century Cures Act, focuses on three pillars that every sponsor must address:
- Relevance: Does the data contain the necessary information (e.g., specific outcomes, exposures, and patient characteristics) to answer the clinical question? This involves assessing the “fitness-for-purpose” of the data source.
- Reliability: Was the data collected accurately and with integrity? This includes evaluating the data accrual process and the quality assurance measures in place at the source.
- Transparency: Are the study protocols and analysis plans pre-specified? To avoid “data dredging” (searching for a positive result after the data has been collected), the FDA requires that RWE studies follow the same rigorous pre-registration standards as RCTs.
Under the Prescription Drug User Fee Act (PDUFA) VII, the FDA has committed to further integrating RWE into its decision-making process, including a pilot program for RWE submissions to support new labeling claims.
European and UK Frameworks
Across the Atlantic, the EMA “Regulatory Science to 2025” strategy aims to integrate RWE into every stage of the drug lifecycle. The DARWIN EU (Data Analysis and Real World Interrogation Network) is a prime example. It acts as a federated platform to interrogate European healthcare data, providing the EMA with rapid access to RWE for safety and efficacy evaluations.
In the UK, the NICE (National Institute for Health and Care Excellence) real-world evidence framework provides clear guidelines for how RWE can impact price and reimbursement. NICE uses RWE to fill evidence gaps in their health technology assessments (HTAs), particularly when RCT data is limited. This ensures that patients get access to innovative treatments while ensuring the NHS receives value for money. Similarly, Health Canada has been active in developing guidance for using RWE in submissions, particularly for rare diseases and during public health emergencies like the COVID-19 pandemic.
Overcoming Challenges in Data Quality and Privacy
Despite the immense promise, RWE is not a magic wand. We face significant hurdles, primarily around data quality, standardization, and patient privacy. Unlike clinical trial data, which follows strict CDASH (Clinical Data Acquisition Standards Harmonization) standards, RWD is often messy, unstructured, and inconsistent.
Stop Missing Data from Killing Your Research
One of the primary challenges is the “missing data” problem. In a clinical trial, every data point is meticulously recorded. In a real-world EHR, a doctor might forget to record a patient’s weight, or a lab result might be stored as a scanned PDF that is unreadable by standard software. Furthermore, biases—such as selection bias and confounding by indication—are inherent in observational data. For example, doctors might prescribe a new, expensive drug only to the sickest patients, making the drug appear less effective than it actually is.
To combat this, we use advanced biostatistical methods:
- Propensity Score Matching: This technique helps balance the characteristics of patients who received the treatment versus those who didn’t, mimicking the randomization process of an RCT.
- Inverse Probability Weighting: A method used to account for non-random treatment assignment.
- Instrumental Variable Analysis: A technique used to estimate causal relationships when controlled experiments are not possible.
Furthermore, the WHO and HL7 collaboration on data standards is helping to harmonize how EHR data is recorded globally. The adoption of the OMOP (Observational Medical Outcomes Partnership) Common Data Model is a game-changer, allowing researchers to run the same analysis code across different databases in different countries without moving the data.
Privacy and the Federated Revolution
Privacy is the other side of the coin. With GDPR in Europe and HIPAA in the US, moving patient data is legally and ethically complex. Cross-border studies face additional problems, as data sovereignty laws in many countries prohibit the transfer of health records outside national boundaries. This is where Lifebit’s federated platform changes the game.
Instead of moving the data to the analysis (which creates security risks and regulatory headaches), we move the analysis to the data. This federated approach ensures that sensitive patient information never leaves its secure environment (such as a hospital’s server or a national health registry) while still enabling multi-site, multinational research at scale. This is the only viable path forward for global precision medicine research.
Future Innovations in Evidence Generation
The future of real-world evidence clinical trials is being written by Generative AI and the OMOP revolution. AI and machine learning are now capable of scanning millions of unstructured doctor’s notes to find safety signals seven months before they appear in medical literature. Natural language processing (NLP) models can extract structured clinical data from free-text notes, pathology reports, and radiology summaries—unlocking vast amounts of information that was previously inaccessible to researchers.
Wearable devices are also providing a continuous stream of “high-definition” RWD. Traditional trials rely on “snapshots” taken during clinic visits every few weeks. Wearables, from continuous glucose monitors to cardiac rhythm sensors, generate granular, longitudinal data that captures treatment effects in real-time. This allows us to see how a drug affects a patient’s sleep, activity levels, and heart rate in their natural environment, providing a much more holistic view of patient health.
Frequently Asked Questions about RWE
How does RWE complement traditional RCTs?
RWE doesn’t replace RCTs; it bridges the gap between “can it work?” (efficacy) and “does it work in practice?” (effectiveness). RCTs provide the internal validity needed for initial approval, while RWE provides the external validity needed for long-term safety, label expansions, and payer value demonstrations. Think of RCTs as the laboratory test and RWE as the field test.
What are the primary sources of Real-World Data?
The most common sources include:
- Electronic Health Records (EHRs): Detailed clinical data from hospital and clinic visits.
- Claims Data: Billing information from insurance providers, which is excellent for tracking patient journeys and costs.
- Patient Registries: Collections of data for specific diseases, often managed by patient advocacy groups or medical societies.
- Digital Health Technologies: Data from wearables, mobile apps, and sensors that provide continuous monitoring.
- Social Media and Patient Forums: Increasingly used for sentiment analysis and understanding the patient’s perspective on side effects.
Why is China leading in RWE trial volume?
China’s leadership (29.9% of global trials) is driven by a massive, centralized patient population and a rapid digital leap in healthcare infrastructure. Their regulatory body (NMPA) has also been aggressive in issuing guidance to accelerate drug approvals through RWD, particularly in oncology, where the need for new treatments is urgent.
What is the role of “Tokenization” in RWE?
Tokenization is a process that allows researchers to link de-identified patient data across different sources (e.g., linking a patient’s EHR data with their insurance claims) without ever revealing the patient’s identity. This creates a more complete picture of the patient’s health journey while maintaining strict privacy compliance.
Can RWE be used for primary regulatory approval?
Yes, though it is most common in rare diseases and oncology. In these cases, RWE often serves as a synthetic control arm to compare against a single-arm trial. As data quality improves and methodologies become more standardized, we expect to see RWE playing an even larger role in primary approvals across other therapeutic areas.
Conclusion
The era of relying solely on “trial and error” in controlled environments is ending. Real-world evidence clinical trials offer a faster, cheaper, and more representative way to bring life-saving therapies to patients. By using the power of routine healthcare data, we can ensure that treatments are not just effective in a laboratory setting, but truly transformative in the real world.
As we look to the future, the integration of multi-omic data (genomics, proteomics, etc.) with RWD will unlock the next level of precision medicine. We will be able to predict not just if a drug works, but exactly which patient will benefit from it and why. This is the promise of the RWE revolution.
At Lifebit, we are at the forefront of this transformation. Our federated AI platform provides the secure, compliant infrastructure needed to access global biomedical and multi-omic data without compromising patient privacy. From our Trusted Research Environments (TRE) to our Real-time Evidence & Analytics Layer (R.E.A.L.), we empower biopharma and public health agencies to turn global data into actionable clinical insights. The journey from data to discovery has never been shorter.
Accelerate your research with Lifebit’s federated evidence layers today.

