The Future of Health: How AI Platforms are Transforming Government Public Health

Why Government Agencies Are Racing to Adopt AI for Population Health
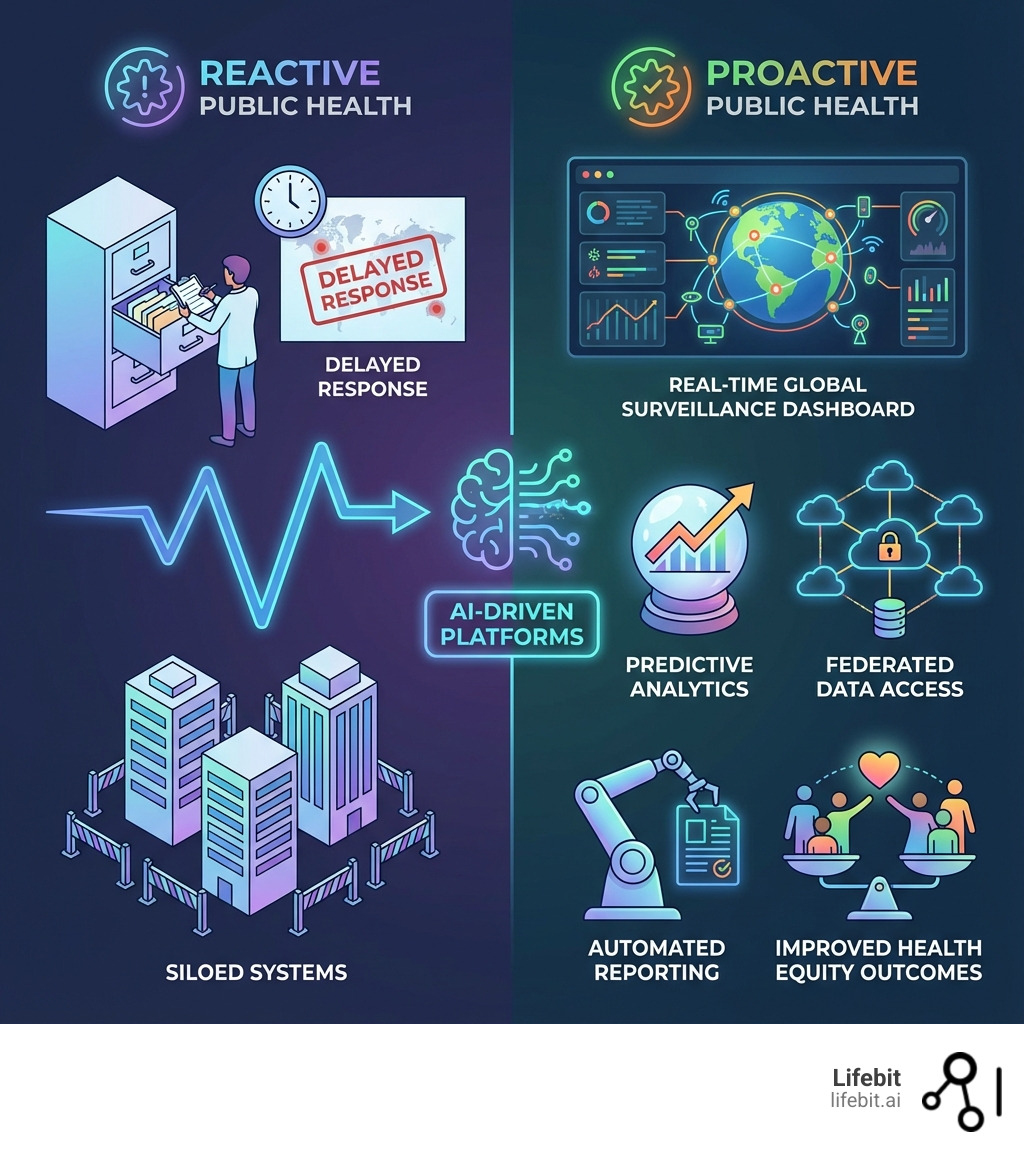
Technology platforms for government ai for population health are now essential infrastructure for public health agencies. They enable a shift from reactive crisis management to proactive, data-driven interventions by analyzing vast, siloed health data in real-time under strict security and privacy standards.
Key Technology Platforms Changing Government Population Health:
- Federated Data Platforms – Enable analysis across siloed datasets without moving sensitive health information.
- Cloud-Based AI Infrastructure – Provide scalable computing power for complex predictive models.
- Trusted Research Environments (TREs) – Create secure, compliant spaces for multi-institutional collaboration.
- AI-Powered Analytics Tools – Include Natural Language Processing (NLP), predictive modeling, and generative AI.
- Data Harmonization Systems – Standardize diverse data sources for AI consumption.
The evidence is compelling: The CDC saved over $3.7 million in labor costs with a generative AI chatbot and cut 5,500 labor hours using AI-powered grant analysis. These are not pilot projects; they are operational systems delivering measurable value today.
This shift is driven by aging populations, chronic diseases, workforce shortages, and the move to value-based care. With over 40% of health payments tied to outcomes, agencies must now measure and predict population health at a scale that manual processes cannot handle.
At Lifebit, we build these platforms, helping federal agencies and public health institutions transform siloed data into actionable insights. Our federated analytics platform powers real-world evidence generation for organizations facing data fragmentation, compliance bottlenecks, and AI inaccessibility.
The New Mandate: Why Government Agencies are Adopting AI for Population Health
The public health landscape is shifting from a reactive field to a proactive, predictive discipline. This evolution is fueled by the move towards value-based care, the rising burden of chronic diseases, and the critical need for health equity. Governments worldwide, from the USA and UK to Canada and Singapore, now see artificial intelligence as a strategic imperative, not just for efficiency gains but for fundamentally transforming how they protect and improve the health of their populations.
The transition to value-based care, where reimbursement is tied to health outcomes rather than services rendered, creates immense pressure on agencies to innovate. With the Centers for Medicare & Medicaid Services (CMS) aiming for 100% of traditional Medicare beneficiaries to be in an accountable care relationship by 2030, the ability to accurately measure risk, predict patient needs, and demonstrate improved outcomes is critical. AI is the engine for this transformation. It improves patient identification for preventative programs, enables sophisticated chronic disease management by detecting early warning signs, and predicts clinical deterioration, allowing for pre-emptive health management that reduces costly hospitalizations and improves quality of life. For Accountable Care Organizations (ACOs), AI models can analyze population data to identify which interventions will have the greatest impact, ensuring resources are allocated effectively to meet stringent quality metrics.
AI also addresses the dual challenges of rising chronic disease rates and persistent operational inefficiencies. In the U.S., six in ten adults have at least one chronic disease, which are the leading drivers of the nation’s $4.1 trillion in annual health care costs. AI can analyze vast datasets—including EHRs, genomics, and even data from wearables—to identify at-risk individuals long before symptoms become severe. Furthermore, with clinicians spending roughly one-third of a clinician’s time is spent on activities outside of patient care, AI-powered tools can streamline administrative workflows, automate documentation, and summarize patient histories, freeing up valuable time for direct patient care. For a deeper dive, explore our guide on AI for Population Health.
Defining AI and Machine Learning in the Public Health Context
To understand the power of technology platforms for government ai for population health, it’s crucial to define key terms. Artificial intelligence (AI) is a machine-based system that can, for a given set of human-defined objectives, make predictions, recommendations, or decisions. It’s a broad field enabling machines to simulate human intelligence. Machine learning (ML) is an application of artificial intelligence that is characterized by providing systems the ability to automatically learn and improve on the basis of data or experience. ML algorithms are the workhorses of modern AI, learning from vast amounts of data to identify patterns and make predictions on new, unseen data.
Key AI technologies transforming public health include:
- Predictive analytics: This technology forecasts future outcomes based on historical data. In public health, this goes beyond just predicting flu seasons. It involves building complex models to forecast demand for hospital beds during a pandemic, identify populations at high risk for developing diabetes in the next five years, or predict which patients are most likely to be readmitted to a hospital after discharge, allowing for targeted post-discharge support.
- Generative AI: This branch of AI creates new content, such as text, images, or data. Its applications in government health are rapidly expanding. Beyond the CDC’s successful GenAI chatbot for staff, generative AI can create high-fidelity synthetic patient data. This synthetic data mirrors the statistical properties of real patient data but contains no actual patient information, allowing researchers to build and test models without compromising privacy.
- Natural Language Processing (NLP): This technology enables computers to understand, interpret, and generate human language. In public health, NLP is invaluable for extracting critical insights from unstructured data sources like clinician notes, pathology reports, public health literature, and even social media feeds. For example, NLP can analyze emergency call transcripts or online forums to detect early signals of a potential disease outbreak based on reported symptoms.
Core Objectives: From Disease Surveillance to Cost Reduction
Government agencies like the Department of Health and Human Services (HHS), the Centers for Disease Control and Prevention (CDC), and CMS are strategically adopting AI to solve complex health challenges. Their shared goals are to improve operational efficiency, foster biomedical innovation, improve patient outcomes, and advance national health goals. The HHS AI Strategy outlines a comprehensive vision for integrating AI across all its divisions, while the CDC aims to empower its entire staff to apply AI for critical functions like outbreak prediction and response. For instance, the CDC’s use of AI to analyze satellite imagery for Legionnaires’ disease outbreaks saved over 280 investigative hours annually, accelerating intervention.
CMS, which manages health coverage for over 160 million Americans, uses AI to improve service delivery, detect fraud, and optimize efficiency, as detailed in its AI Playbook. A common thread across all agencies is reducing the immense administrative burden on the healthcare system. By automating tasks like data entry, claims processing, and report generation, AI frees healthcare professionals to focus on high-value patient interaction. The CDC’s generative AI chatbot, which saved over $3.7 million in labor costs, is a powerful testament that technology platforms for government ai for population health are no longer theoretical but are delivering substantial, real-world value today.
The Engine Room: Key Technology Platforms for Government AI for Population Health
Behind every successful AI initiative is a robust technological foundation. For government agencies managing sensitive population health data, this “engine room” requires more than just raw computing power; it demands specialized capabilities for data management, security, and collaboration. Effective technology platforms for government ai for population health must be secure, scalable, and interoperable by design to handle the complexity and sensitivity of health data.

At Lifebit, our federated AI platform provides this critical infrastructure, enabling secure, real-time analysis of global biomedical data without moving it. Our Trusted Research Environment (TRE) and federated technologies create compliant, auditable spaces for multi-institutional collaboration, which is crucial for managing the fragmented public health data ecosystems that agencies operate within. Learn more about our work with Public Sector Initiatives.
Foundational Infrastructure: Building the Digital Backbone for AI
The effectiveness of AI in public health hinges entirely on its underlying infrastructure. This digital backbone must be purpose-built to handle the unique challenges of health data, prioritizing several key elements:
- Data Harmonization: Public health data comes from countless sources—EHRs, insurance claims, genomic sequencers, public surveys, and environmental sensors—each with its own format and vocabulary. Data harmonization is the process of transforming this disparate data into a unified format. Using a Common Data Model (CDM) like the OMOP CDM standardizes the data structure and terminology, making it possible for AI models to analyze datasets from different institutions as if they were one.
- Interoperability: This is the ability of different IT systems and software applications to communicate, exchange data, and use the information that has been exchanged. Modern platforms achieve this using APIs and standards like HL7 FHIR (Fast Healthcare Interoperability Resources), which allow legacy systems to connect seamlessly with modern AI tools, breaking down data silos between agencies, hospitals, and research institutions.
- Secure Data Access: Protecting patient privacy is non-negotiable. Platforms must provide granular, role-based access controls (RBAC), end-to-end encryption for data in transit and at rest, and comprehensive audit logs of all activity. Technologies like Trusted Research Environments (TREs) provide a ‘five safes’ framework (safe people, safe projects, safe settings, safe data, safe outputs) to ensure that sensitive data can be analyzed without ever being exposed or moved.
- Hybrid Data Ecosystems: Government agencies often have data stored in a mix of on-premise data centers and various private and public clouds. A modern AI platform must operate seamlessly across this hybrid environment, allowing analysis to run wherever the data resides, thus avoiding costly and risky data migrations.
- Scalable Computing: Population-level analysis requires immense computational power. Cloud computing provides on-demand, scalable resources, allowing agencies to spin up powerful computing clusters to train complex models on petabytes of data and then scale them down to save costs, paying only for what they use.
- FAIR Data Principles: To maximize the value of data assets, infrastructure must align with the FAIR principles—making data Findable, Accessible, Interoperable, and Reusable. This involves using rich metadata, persistent identifiers, and clear data-use licenses to ensure that data is well-managed and ready for AI applications.
Essential AI Tools and Technologies in Action
Once the infrastructure is in place, specialized AI tools transform raw data into actionable intelligence:
- Natural Language Processing (NLP): NLP extracts structured information from unstructured text. For example, CMS uses NLP to analyze millions of public comments on proposed regulations, automatically classifying them by theme and sentiment to inform policy decisions. In a clinical setting, NLP can scan doctors’ notes to identify patient symptoms, social determinants of health, and adverse drug events that are not captured in structured EHR fields.
- Predictive Modeling: These models forecast health events by learning from historical data. The CDC’s FluSight program is a prime example; it aggregates multiple predictive models from different research groups into an ensemble forecast that is more accurate than any single model. These models ingest data ranging from past flu seasons and vaccination rates to real-time data like Google search trends for flu symptoms.
- Computer Vision: This AI technology interprets and analyzes visual information. The CDC’s use of computer vision to scan satellite images for cooling towers—potential sources of Legionnaires’ disease—saves hundreds of investigative hours and allows public health officials to act faster to prevent outbreaks.
- Generative AI Chatbots: These tools automate communication and information retrieval. The CDC’s internal staff chatbot, which answers employee questions about agency policies and procedures, has saved millions in labor costs by providing instant answers and freeing up human support staff for more complex issues.
- Anomaly Detection: This technique identifies unusual patterns in large datasets that deviate from the norm. In public health, it is used to detect fraudulent Medicare claims, spot early signs of a disease outbreak in emergency room data, or identify unexpected side effects from a new medication.
From Theory to Impact: Real-World AI Use Cases in Public Health
The true value of AI is measured not by its technical sophistication but by its real-world impact on health outcomes and operational efficiency. Government agencies are already demonstrating significant successes, with the HHS AI Use Case Inventory reporting 271 active or planned AI implementations in FY2024. These are not isolated experiments; they are operational systems delivering tangible ROI and transforming core public health functions. We are proud to provide the secure, federated platforms that enable this vital work. See more on our Federal Health page.
Enhancing Disease Surveillance and Outbreak Response
AI is making a profound difference in the speed, accuracy, and proactivity of disease surveillance and outbreak response.
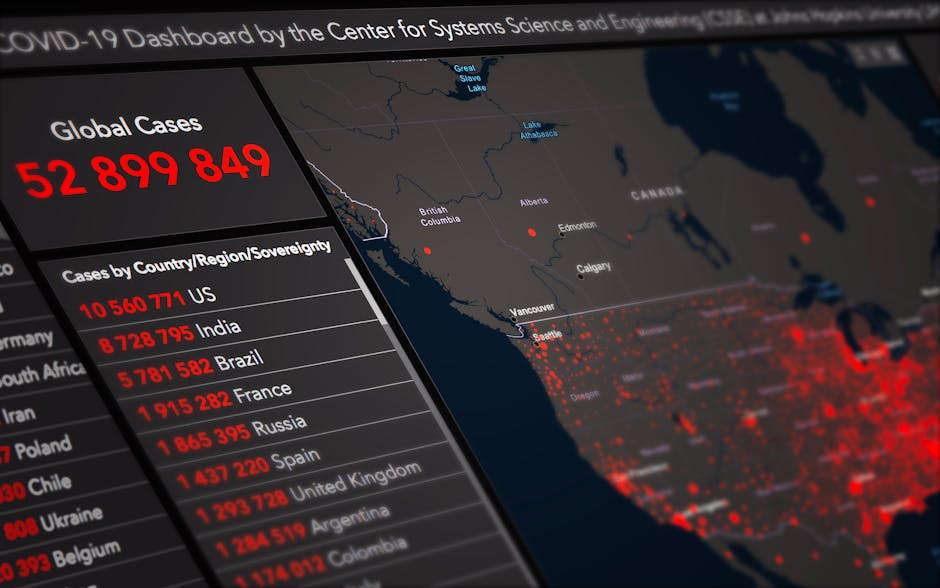
- Legionnaires’ disease: The CDC uses AI-powered computer vision to analyze satellite images to automatically detect cooling towers, a common source of Legionella bacteria. This automated process saves over 280 investigative hours annually and enables public health teams to intervene faster, preventing potential outbreaks.
- FluSight program: The CDC’s FluSight initiative uses predictive analytics to forecast the timing, peak, and intensity of the annual influenza season. It functions as a collaborative forecast, combining dozens of different models from academic and private-sector teams into a single, more accurate ensemble prediction. This allows healthcare systems to better prepare for surges by managing staff, beds, and supplies.
- Syndromic surveillance: AI significantly enhances systems like the National Syndromic Surveillance Program (NSSP), which analyzes de-identified data from over 70% of U.S. emergency department visits in near real-time. AI algorithms continuously scan this data for unusual patterns or clusters of symptoms (e.g., a spike in “cough and fever” complaints), flagging potential outbreaks days or even weeks before they would be confirmed through traditional lab reporting.
- Satellite image analysis: Beyond specific diseases, AI-powered analysis of satellite imagery helps monitor environmental factors linked to public health risks. This includes tracking mosquito breeding grounds to predict vector-borne diseases like Zika or West Nile virus, monitoring air quality changes from wildfire smoke, or identifying communities vulnerable to extreme heat events.
Optimizing Resource Allocation and Public Health Logistics
AI is becoming an indispensable tool for ensuring that limited public health resources are deployed for maximum impact.
- Predicting Healthcare Demand: During public health emergencies, AI models can forecast demand for critical resources like hospital beds, ICU capacity, ventilators, and PPE. By analyzing infection rates, population density, and demographic vulnerabilities, these models help officials anticipate shortages and proactively manage the supply chain.
- Optimizing Vaccination Campaigns: AI was used during the COVID-19 pandemic to help plan vaccine distribution. Models identified optimal locations for vaccination sites to ensure equitable access, calculated the most efficient delivery routes, and predicted vaccine uptake rates in different communities to tailor outreach efforts.
- Targeting Interventions: AI can analyze diverse datasets to identify geographic “hotspots” or specific populations that would benefit most from a public health intervention, such as mobile health clinics, lead screening programs, or nutritional assistance.
Streamlining Operations and Accelerating Research
AI’s impact extends deep into the operational core of health agencies, driving unprecedented efficiency and accelerating the pace of research.
- Grant report analysis: The CDC deployed AI tools using NLP to analyze thousands of grant recipient reports. The system automatically extracted key performance indicators, identified common themes and challenges, and summarized outcomes, reducing manual effort by 5,500 labor hours and saving an estimated $500,000.
- GenAI chatbots: The CDC’s generative AI chatbot for all staff has become a significant productivity tool, saving over $3.7 million in estimated labor costs by providing instant answers to internal queries. This has achieved a remarkable 527% ROI.
- Administrative task automation: Across the healthcare system, AI is automating routine tasks like patient scheduling, medical coding, and prior authorization requests, freeing clinicians and administrative staff to focus on more complex, patient-facing work.
- Accelerating research: AI supports the goals of the Public Health Data Strategy by enabling rapid, large-scale analysis of complex datasets. As highlighted in the annual HHS AI Use Case Inventory, AI platforms are optimizing data exchange and analysis, shortening the timeline from data collection to actionable insight.
Building Trust: Governance, Ethics, and Security in Government AI
While the potential of technology platforms for government ai for population health is immense, their responsible deployment hinges on a foundation of robust governance, ethics, and security. Trust is the bedrock of public health, and any erosion of that trust could undermine the very goals these technologies aim to achieve. This is why our federated platform integrates strong governance and security by design, ensuring that innovation does not come at the expense of public confidence. For more detailed guidance, refer to our Federal Health Guide.
The Policy Landscape: Federal Mandates Shaping AI Adoption
Government agencies are not innovating in a vacuum. They are guided by a comprehensive and evolving policy landscape for responsible AI adoption. Key federal mandates, including the HHS AI Strategy, the Office of Management and Budget’s memo M-25-21 on “Advancing Governance, Innovation, and Risk Management for Agency Use of Artificial Intelligence,” various Executive Orders on AI, and the CMS AI Playbook, provide a unified framework. These directives create a coordinated, government-wide approach, emphasizing ethical development, rigorous risk management, transparency in AI use, and the paramount importance of building and maintaining public trust.
Mitigating Risks: Addressing Bias, Privacy, and Security
AI’s power comes with significant risks that must be proactively identified and managed to build public trust and ensure equitable outcomes.
- Algorithmic bias: AI models trained on biased historical data can perpetuate and even amplify existing health disparities. For example, an algorithm that uses past healthcare spending to predict future health needs may systematically under-serve minority populations who have historically faced barriers to care and thus have lower spending records for the same level of illness. Mitigating this requires curating diverse and representative training data, using fairness-aware machine learning techniques, and conducting regular audits for biased outcomes across different demographic groups.
- Human-in-the-loop: To counteract AI errors and inherent biases, a “human-in-the-loop” approach is critical for high-stakes decisions. This ensures that human experts review, validate, and ultimately oversee AI-generated recommendations before they impact patient care. This can range from a clinician confirming an AI-flagged diagnosis (human-in-the-loop) to an epidemiologist investigating an AI-generated outbreak alert (human-on-the-loop).
- Privacy and HIPAA Compliance: All platforms must strictly adhere to privacy regulations like the Health Insurance Portability and Accountability Act (HIPAA). However, modern platforms go further by incorporating Privacy-Enhancing Technologies (PETs). These include federated learning, where models are trained on decentralized data without the data ever leaving its source location, and differential privacy, which adds mathematical noise to query results to make it impossible to re-identify individuals from the data.
- NIST Risk Management Framework: To standardize risk management, agencies are adopting frameworks like the NIST AI Risk Management Framework. This provides a structured process to Govern (establish a culture of risk management), Map (identify risks in the specific AI context), Measure (assess and analyze risks), and Manage (treat risks with appropriate mitigations), ensuring AI systems are trustworthy, reliable, and secure.
- Responsible AI (RAI): Implementing RAI principles is the overarching goal. This means ensuring that AI systems are designed and operated to be fair, transparent, accountable, safe, privacy-preserving, and reliable. It requires a holistic approach that combines technical solutions, strong governance, and a commitment to ethical practice.
A Practical Guide: Implementing AI in Your Agency
Implementing technology platforms for government ai for population health requires a strategic approach that combines technology with workforce development, public-private partnerships, and a culture of innovation. For comprehensive guidance, explore our resource on AI for Population Health Management.
Building an AI-Ready Workforce and Promoting AI Literacy
An AI platform is only as effective as the people using it. Agencies are building an AI-ready workforce by developing upskilling programs and promoting AI literacy. The CDC, for example, has established an AI Community of Practice (CoP) with over 2,200 members and an AI Accelerator (AIX) program to operationalize and scale AI technologies. These initiatives, along with role-based training and a culture that encourages experimentation, are crucial for successful adoption.
Evaluating Technology Platforms for Government AI for Population Health
Selecting the right technology platform is a strategic decision. Agencies should evaluate platforms based on these core capabilities:
- Scalability: Can the platform handle massive and growing public health datasets without performance degradation?
- Security: Does it meet stringent security standards and certifications for handling sensitive health data?
- Interoperability: Can it integrate seamlessly with existing legacy systems, EHRs, and other data sources?
- Vendor Lock-in Avoidance: Does it use open, portable solutions to ensure future flexibility?
- Total Cost of Ownership: What are the long-term costs for maintenance, upgrades, and training?
- Data Governance: Does it provide robust tools for access control, auditing, and compliance management? Our federated platform is designed with these capabilities at its core.
The Future Horizon: What’s Next for AI in Public Health?
The future of technology platforms for government ai for population health is moving towards more sophisticated, integrated, and proactive applications. The vision is one of predictive prevention and personalized public health, where interventions are precisely targeted and delivered before crises emerge.
Future Trends in Technology Platforms for Government AI for Population Health
Several key technology trends are set to reshape public health AI platforms:
- Digital twins: Virtual replicas of cities or healthcare systems will allow for simulating policy impacts and predicting disease spread before real-world implementation.
- Edge computing: Processing data closer to its source will enable faster, real-time analytics while enhancing privacy.
- AI-integrated commons: Shared data resources, models, and testbeds across government agencies, as envisioned by HHS, will accelerate reusable AI innovation.
- Open-source tools: A growing emphasis on open-source tools will promote transparency, collaboration, and reduce reliance on proprietary solutions.
- Real-time data processing: Future platforms will further improve real-time capabilities, allowing for instantaneous insights and decision-making during public health emergencies.
The Vision: Personalized Public Health and Predictive Prevention
The ultimate goal is a future where health is managed proactively, individually, and equitably.
- Proactive outreach: AI will identify at-risk populations for targeted interventions before diseases progress.
- Risk stratification at scale: AI will improve risk prediction, allowing for precision public health interventions custom to community needs.
- AI-augmented clinicians: AI will serve as a supportive tool, augmenting the capabilities of public health professionals, not replacing them.
- Precision medicine: By integrating vast datasets, AI will accelerate breakthroughs in more personalized and effective treatments.
- Health equity by design: AI can help overcome health disparities by providing services like real-time translation or identifying systemic inequities for targeted action.
Conclusion: Opening up the Next Era of Public Health with Secure AI Platforms
The journey to leverage technology platforms for government ai for population health is a strategic imperative. We are entering a new era of public health defined by unprecedented insights, greater efficiency, and better health outcomes. The statistics—millions saved and thousands of hours freed—prove the value of a proactive approach to population well-being.
Key challenges remain, including overcoming data silos and ensuring robust governance and security. However, solutions are emerging. Federated analysis platforms, like ours at Lifebit, are instrumental in addressing these issues. By enabling analysis on distributed data without moving it, we provide compliant, real-time insights for public health agencies. Our Trusted Research Environment (TRE) and other solutions facilitate secure collaboration across complex data ecosystems.
The commitment from government agencies worldwide signals a shared vision. By investing in the right technology platforms for government ai for population health, fostering an AI-ready workforce, and establishing strong ethical frameworks, we can open up AI’s full potential. We invite you to partner with us in this mission. Explore solutions for government and find how our federated AI platform can empower your agency to make data-driven decisions that save lives.

