Healthcare Data Sources 101

Half Your Care Data Is Missing: Link Claims + EHR Now to Slash RWE Blind Spots and Delays

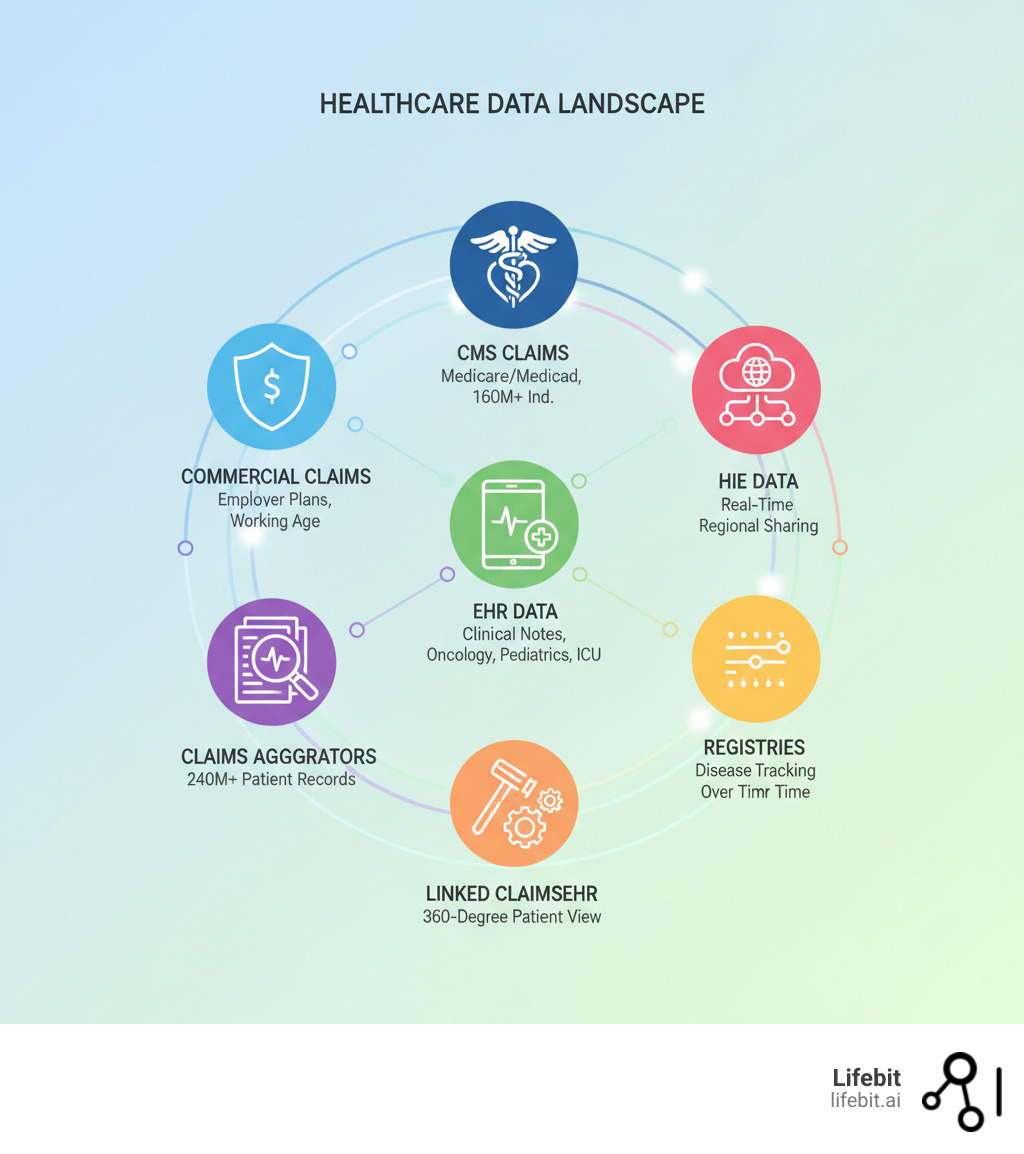
Provide health care data (e.g., commercial and Centers for Medicare & Medicaid Services (CMS)) claims data, commercial claims aggregators data, claims data linked to electronic health records (EHR) data, specialty EHR Data (e.g., oncology, pediatrics, geriatrics, hospital intensive care unit (ICU)), disease or product registry or registry network data, and Health Information Exchange (HIE) Data). is essential for generating real-world evidence that improves patient outcomes, accelerates drug development, and informs healthcare policy.
The healthcare industry is sitting on a data goldmine, but this data is scattered across dozens of incompatible systems. Each source offers a different lens on patient care:
- Claims Data (Commercial & CMS): Insurance records covering what happened and what it cost for diverse populations, from working-age individuals to over 160 million Medicare/Medicaid beneficiaries.
- Claims Aggregators: Large-scale datasets from clearinghouses containing claims from millions of patients.
- EHR Data: Digital patient records with clinical details like lab results, vital signs, and physician notes.
- Specialty EHR Data: Focused datasets for fields like oncology, pediatrics, and ICU care.
- Linked Claims-EHR Data: Combined datasets offering both longitudinal cost information and deep clinical context.
- Disease/Product Registries: Patient-level data tracking specific conditions or treatments over time.
- HIE Data: Real-time health information shared across regional healthcare systems.
This fragmentation creates blind spots. Research shows claims data alone misses up to 50% of preventive services documented in EHRs, while EHRs often lack the long-term view of claims. For pharmaceutical companies, public health agencies, or regulators, having access to integrated, high-quality data is mission-critical. The ability to provide comprehensive health data in a secure, analysis-ready format determines whether you can generate real-world evidence at the speed of science.
I’m Maria Chatzou Dunford, CEO and Co-founder of Lifebit. My background in computational biology and AI has shown me how breaking down data silos accelerates findy and saves lives. We’ve spent over a decade building federated platforms that help organizations securely connect diverse health data across institutions without moving sensitive information.
Simple guide to providing comprehensive healthcare data:
- cms data
- hie health information exchange
- health information
Commercial vs. CMS Claims: Choose Right to Tap 160M+ Lives and Cut Time-to-Insight
Think of claims data as the financial diary of healthcare. Generated for billing purposes, these records have become a powerful tool for understanding real-world healthcare patterns. What makes claims data special is its longitudinal view. It captures a patient’s entire journey—diagnoses, procedures, medications, and costs—across different doctors, hospitals, and pharmacies over months or even years. This breadth is invaluable for pharmacoepidemiology and health economics research.
The Anatomy of a Healthcare Claim
To leverage claims data effectively, it’s crucial to understand its core components. Each claim is a structured record containing several key pieces of information:
- Patient Demographics: Basic information like age, gender, and geographic location (often at the zip code level), which allows for population-level analysis.
- Provider Information: Details about the healthcare provider who rendered the service, identified by a National Provider Identifier (NPI), which helps track care across different settings.
- Diagnosis Codes (ICD-10-CM): These codes represent the “why” of the encounter, specifying the patient’s conditions or symptoms. They are fundamental for identifying patient cohorts with specific diseases.
- Procedure Codes (CPT/HCPCS): These codes detail the “what”—the specific services, procedures, or supplies provided to the patient. They are used to study treatment patterns and healthcare utilization.
- National Drug Codes (NDC): For pharmacy claims, NDCs identify the specific medication dispensed, including its manufacturer, strength, and dosage form. This is essential for studying medication adherence and effectiveness.
- Dates of Service: Timestamps for each encounter create the longitudinal record, allowing researchers to map out a patient’s healthcare journey over time.
- Costs: Financial data includes the amount billed by the provider, the amount approved and paid by the insurer, and the patient’s out-of-pocket responsibility. This is critical for health economics and outcomes research (HEOR).
Commercial Claims Data vs. CMS Claims Data
Not all claims data is the same. Commercial claims data comes from private insurers and primarily covers a healthier, working-age population and their dependents. Resources like the Data Repository from FAIR Health provide insights into how this group uses healthcare, making it ideal for studying conditions prevalent in younger to middle-aged adults or for analyzing employer-sponsored health trends.
CMS claims data represents a different reality, covering over 160 million individuals through Medicare (adults 65+ and those with certain disabilities) and Medicaid (low-income families and individuals). This is where you find deep data on chronic disease, end-of-life care, and vulnerable populations. The Chronic Conditions Data Warehouse (CCW) makes this data particularly valuable for research. If you’re studying Alzheimer’s, long-term diabetes complications, or health disparities in low-income groups, CMS data is essential. Researchers can navigate these vast datasets using tools like the Research Data Assistance Center’s Find the CMS Data File You Need.
The choice depends on your research question. Studying workplace wellness? Use commercial claims. Investigating post-acute care in the elderly? CMS is your answer.
The Role of Commercial Claims Aggregators
Commercial claims aggregators like Merative (formerly IBM Watson Health), Optum, and IQVIA create massive, anonymized datasets by consolidating billing records from numerous insurance companies, representing hundreds of millions of patients. This scale solves the problem of sample size, enabling research on rare diseases and comparisons of treatment patterns across regions. Aggregators help overcome the limitations of “closed” claims systems (data from a single payer), which only show a patient’s activity within that plan. By combining data from many payers, they provide a more complete longitudinal record, even if a patient switches insurance.
These datasets are crucial for comparative effectiveness research, disease prevalence tracking, and post-market drug safety surveillance. However, claims data has inherent limitations. It was built for billing, not clinical research. Diagnoses are billing codes, not clinical confirmations, and you won’t find lab values, vital signs, or clinical reasoning. Coding inaccuracies can occur, and medication adherence is an educated guess based on prescription fills, not actual consumption. This is why researchers increasingly look to combine claims with other sources, like EHR data, to get a more complete picture.
Get the Clinical Why You’re Missing: Use EHR Data to Unlock Labs, Vitals, and Outcomes
If claims data is the “what” and “how much,” Electronic Health Records (EHRs) are the “why” and “how.” Created at the point of care, EHRs are the digital story of a patient’s health journey, capturing clinical decisions, test results, and treatment responses as they happen.
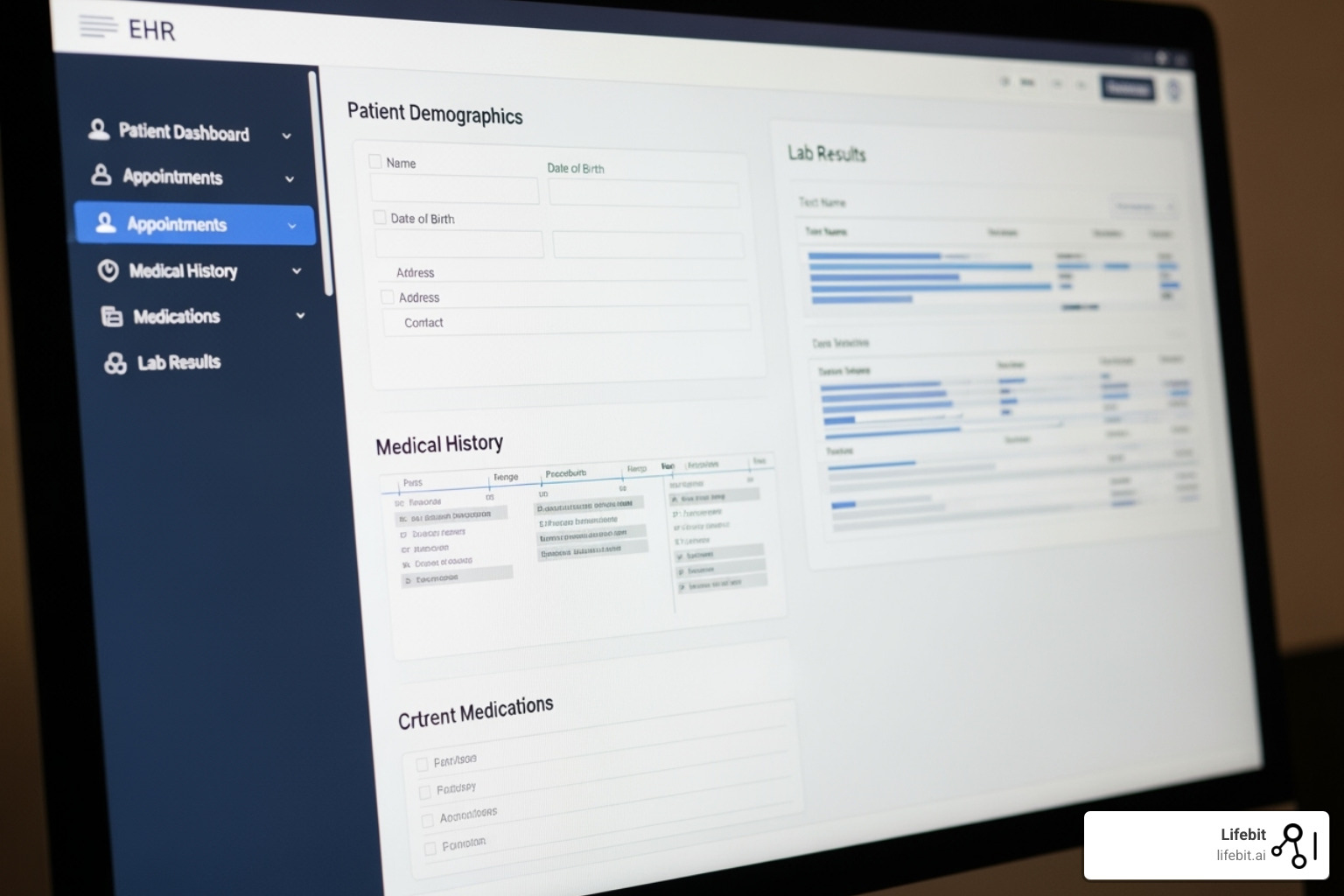
This rich clinical context is what makes EHR data a powerhouse. A billing code shows “Type 2 Diabetes,” but the EHR reveals the full clinical narrative: HbA1c levels over time, blood pressure readings, medication history (including drugs prescribed but not filled), and physician notes detailing treatment rationale. This granular detail includes lab results, vital signs, imaging files, and a vast amount of unstructured data that can be analyzed to extract hidden insights. This depth is invaluable for identifying patient cohorts based on complex clinical criteria that are invisible in claims data.
However, EHR data has its own challenges. Data incompleteness is common, and documentation practices vary widely between clinicians and institutions. Interoperability issues between different EHR systems (like Epic, Cerner, and Allscripts) create fragmentation, requiring significant data engineering to normalize data for research. Furthermore, system-specific biases exist; an academic medical center’s EHR will reflect a different patient population and care patterns than a community hospital’s. Despite these problems, the clinical depth of EHRs is essential for generating meaningful real-world evidence.
Unlocking Unstructured Data with Natural Language Processing (NLP)
A significant portion of the most valuable clinical information—up to 80% of all EHR data—is locked away in unstructured formats like clinical notes, discharge summaries, pathology reports, and radiology interpretations. This narrative text contains the clinical reasoning, patient-reported symptoms, and social determinants of health (SDoH) that structured fields often miss. Natural Language Processing (NLP) is the key to unlocking this treasure trove. NLP algorithms can be trained to read and interpret human language, extracting specific concepts and relationships. For example, NLP can identify a patient’s smoking status, reasons for medication non-adherence, or subtle disease symptoms mentioned in a physician’s notes, transforming unstructured text into structured, analyzable data points.
The Value of Specialty EHR Data (e.g., oncology, pediatrics, geriatrics, ICU)
Specialty EHR data provides an even deeper level of detail for specific medical fields, capturing data points that are critical for that domain but absent in general EHRs.
-
Oncology EHRs: These systems capture precise tumor characteristics (e.g., histology, grade), cancer staging (TNM), genomic testing results (e.g., EGFR, BRCA mutations), and performance status scores (e.g., ECOG). They track complex chemotherapy and immunotherapy regimens, treatment lines, and specific patient responses (e.g., RECIST criteria), which are fundamental for cancer research. Initiatives like USCDI+Cancer are standardizing this data capture, creating a foundation for large-scale cancer research. Learn more at More on USCDI+Cancer from HealthIT.gov.
-
Pediatric EHRs: These track growth charts, developmental milestones, and complex vaccination schedules. They use data structures fundamentally different from adult records, often including caregiver information and social context crucial for understanding a child’s health.
-
Geriatric EHRs: These focus on the interplay of multiple chronic conditions (multimorbidity), polypharmacy risks, and functional status assessments (e.g., Activities of Daily Living). They are designed to capture the unique complexities of caring for older adults.
-
Hospital ICU EHRs: These capture high-frequency, high-resolution physiological data, often streamed directly from bedside monitors. This includes minute-by-minute heart rate, continuous blood pressure from arterial lines, and detailed ventilator settings (e.g., PEEP, FiO2). This granular data is critical for developing predictive models for conditions like sepsis or acute respiratory distress syndrome (ARDS) and for conducting highly precise critical care research.
Specialty EHR data allows researchers to answer highly specific questions that general datasets cannot. It provides the right data for improving care in specific populations, opening up research possibilities that were impossible a decade ago.
Build a 360-Degree Patient View Now: Link Claims, EHR, Registries, and HIE Without Moving Data
The real magic happens when we build bridges between isolated data sources. Claims data shows where a patient went, EHR data reveals what happened clinically, registries track specific diseases with deep granularity, and Health Information Exchanges (HIEs) connect the dots in real-time. Together, they create a 360-degree view of the patient journey, transforming scattered information into actionable real-world evidence.
Linking Claims and EHR Data: The Best of Both Worlds
Combining claims and EHR data merges a bird’s-eye view with a microscopic examination. This integration allows for building comprehensive patient cohorts, improving adherence analysis (by comparing prescriptions in the EHR to fills in claims), and conducting more precise health economic studies. The longitudinal view from claims combined with the rich clinical context from EHRs creates unparalleled breadth and depth.
However, this integration is complex. Patient matching is a major technical and privacy challenge. Methodologies include:
- Deterministic Matching: This approach links records based on exact matches of unique personal identifiers like a Social Security Number or a system-specific patient ID. While highly accurate, these identifiers are rarely available for research due to privacy regulations.
- Probabilistic Matching: This more common method uses algorithms to calculate a “match score” based on the similarity of non-unique identifiers like name, date of birth, gender, and address. It can link records even with slight variations or missing data but requires careful tuning to balance the risk of false positives (incorrectly linking two different people) and false negatives (failing to link records for the same person).
Often, this process is handled by a trusted third party using Privacy-Preserving Record Linkage (PPRL) techniques, where encrypted or tokenized identifiers are matched without exposing raw personal information. A study on linking claims and EHR data highlights these methodological complexities. Furthermore, relying on claims alone can underestimate the quality of care, as many services documented in EHRs never appear in claims.
Here’s how these data sources compare:
| Feature | Claims Data | EHR Data | Linked Claims-EHR Data |
|---|---|---|---|
| Primary Purpose | Reimbursement, billing | Clinical care, patient management | Comprehensive RWE, holistic patient view |
| Data Granularity | Billing codes (ICD, CPT), drug codes, costs | Detailed clinical notes, lab results, vitals, images | Billing codes + detailed clinical context |
| Longitudinal View | Strong (across payers, if aggregated) | Often limited to single health system | Strong (longitudinal clinical and cost data) |
| Population Coverage | Defined by payer (commercial, Medicare, Medicaid) | Defined by health system | Defined by linked populations |
| Clinical Depth | Low (billing-focused) | High (clinical-focused) | High (combines breadth of claims with depth of EHR) |
| Strengths | Cost analysis, utilization patterns, large populations | Granular clinical detail, treatment specifics, narratives | Holistic patient journey, robust research cohorts |
| Limitations | Lacks clinical detail, coding inaccuracies, reimbursement bias | Inconsistent documentation, interoperability issues, system bias | Technical complexity, patient matching, data governance |
The Role of Disease/Product Registries and HIE Data
Disease and product registries add another crucial dimension. These specialized databases track specific patient populations or treatments over time, capturing deep phenotype data (detailed clinical characteristics) often missing from standard systems. For example, the Cystic Fibrosis Foundation Patient Registry has been instrumental in transforming CF care by tracking outcomes, benchmarking care quality across centers, and accelerating clinical trial recruitment. Product registries are vital for post-market surveillance, such as tracking the long-term performance and failure rates of a new artificial hip joint to monitor its real-world safety and effectiveness.
Health Information Exchanges (HIEs) solve the problem of care fragmentation. They are digital bridges connecting disparate EHR systems within a region, enabling secure, timely sharing of patient information between providers for treatment purposes. For research, HIEs offer a powerful, near-real-time view of a patient’s encounters across different health systems in a geographic area. Unlike claims data, which has a time lag, HIEs provide immediate access to clinical information, which is invaluable for public health surveillance (e.g., tracking flu outbreaks) and care coordination studies. By employing sophisticated patient matching algorithms, HIEs serve as the connective tissue that helps unify diverse data sources, ensuring you see the whole patient journey.
Your Multi-Source Study Will Fail Without This: Standards, Interoperability, and Privacy Done Right
Working with diverse healthcare data sources requires overcoming significant challenges in data standardization, interoperability, and privacy. These are not just technical problems but also involve complex governance, security, and regulatory compliance. Without a robust framework to address these issues, any large-scale, multi-source data initiative is destined to fail.
Overcoming Data Standardization and Interoperability Problems
Healthcare data is fragmented across countless “silos”—EHR systems, claims databases, and registries—each with its own proprietary format and terminology. This makes combining data for analysis incredibly difficult and time-consuming.
Data standardization and interoperability are the solutions. Interoperability is the ability of different systems to exchange and use data, while standardization involves agreeing on common formats and terminologies.
Fortunately, the industry is making progress through several key initiatives:
- Common Data Models (CDMs): CDMs like the OMOP (Observational Medical Outcomes Partnership) and PCORnet models create a unified format for observational health data. They act as a universal translator, mapping disparate source data into a consistent structure (e.g., tables for
PERSON,CONDITION_OCCURRENCE,DRUG_EXPOSURE) and a standardized vocabulary (e.g., SNOMED, RxNorm, LOINC). This allows researchers to write a single analysis script that can be executed across a network of databases (like the OHDSI network), dramatically accelerating large-scale, multi-institutional research. - Health Level Seven (HL7): This organization establishes international standards for data transfer. Its modern Fast Healthcare Interoperability Resources (FHIR) standard is a game-changer, enabling real-time, API-based data exchange that is far more flexible and easier to implement than older standards. Learn more at Health Level Seven (HL7).
- US Core Data for Interoperability (USCDI): This defines a standardized set of essential health data classes and elements that certified health IT systems must be able to exchange. This federal requirement ensures that a baseline of critical patient information is consistently available. The ONC leads these efforts, detailed at ONC Interoperability initiatives.
Despite these efforts, harmonizing data, especially unstructured text and data from highly specialized domains, remains a challenge. But the payoff—a connected and insightful healthcare data ecosystem—is worth the effort.
Upholding Ethical and Regulatory Standards
Protecting patient privacy is non-negotiable and a prerequisite for public trust. This means navigating a complex landscape of regulations like HIPAA in the US and GDPR in Europe, which set stringent rules for handling protected health information (PHI).
De-identification techniques are essential for removing personal identifiers to enable research while protecting privacy. This goes beyond simply removing names and addresses. HIPAA outlines two pathways: the Safe Harbor method, which involves removing a specific list of 18 identifiers, and the Expert Determination method, where a statistician certifies that the risk of re-identification is very small. Researchers also use legally binding Data Use Agreements (DUAs) that specify exactly how data can be used, stored, and secured. The entire research plan is typically reviewed and approved by an Institutional Review Board (IRB) to ensure it is ethically sound and that patient welfare is protected.
One of the most promising approaches for balancing research needs with privacy is federated data access. Instead of centralizing sensitive data, this model sends analytical algorithms to the data where it resides. Only aggregated, de-identified results are returned to the researcher, significantly improving privacy and security. This is the core principle behind the Lifebit platform. Other Privacy-Enhancing Technologies (PETs) are also emerging, such as differential privacy, which adds mathematical noise to query results to make it impossible to isolate an individual’s contribution, and homomorphic encryption, which allows computations to be performed directly on encrypted data.
Adhering to these standards builds public trust and is emphasized in guidelines like the “Good practices for real-world data studies” which call for rigorous and ethical conduct.
Turn Raw Data into Real-World Evidence Fast: Safer Drugs, Smarter Care, Lower Costs
The goal of integrating diverse healthcare data is to transform raw information into insights that improve patient lives. When researchers can effectively access and analyze comprehensive health data, they can answer critical questions about treatment effectiveness, real-world side effects, and the true cost of care.

This integrated approach is the foundation of robust Real-World Evidence (RWE), which shows how treatments perform in the messy reality of everyday clinical practice. It captures the full spectrum of patients, not just idealized study subjects.
- Comparative effectiveness research becomes more powerful, helping clinicians and patients make informed decisions based on evidence from people with similar health challenges.
- Pharmacoepidemiology and safety surveillance benefit from large-scale data, allowing regulators to spot rare side effects that might be missed in clinical trials.
- Understanding healthcare costs and utilization becomes more precise by connecting the financial data in claims with the clinical context in EHRs.
Perhaps the most exciting frontier is personalized medicine. By weaving together clinical, cost, genetic, and real-time data, we are moving toward a future of customized treatments.
Biomarker findy is a prime example, linking genomic data with clinical outcomes to predict who will respond to a particular drug. Research on DNA biobanks linked to medical records is opening new frontiers in this area. This leads to targeted therapies that get patients on the right treatment faster.
Predictive analytics powered by AI can forecast disease progression and identify high-risk patients, shifting medicine from reactive to proactive. At Lifebit, our federated platform is built to enable this transformative research, allowing analysis of multi-source data while keeping it secure, turning the promise of personalized medicine into reality.
FAQ: Claims vs. EHR, Linking, and Privacy—Do This Now to Speed RWE
What is the main difference between claims data and EHR data?
Claims data is the financial receipt of healthcare, created for billing. It provides a long-term view of what services were provided and what they cost across different providers. EHR data is the clinical story, created at the point of care. It contains rich details like lab results and physician notes, explaining why a service was provided.
Why is linking different healthcare data sources so important for research?
Linking sources like claims and EHRs creates a 360-degree patient view that neither can provide alone. It combines the longitudinal breadth and cost data of claims with the clinical depth of EHRs. This enables more accurate research into treatment effectiveness, medication adherence, and the true value of care.
What are the biggest challenges when working with healthcare data?
The three biggest challenges are:
- Interoperability: Getting different systems, which were often built in isolation, to connect and share data.
- Standardization: Ensuring data from different sources uses a common language and format so it can be combined and analyzed consistently.
- Privacy and Security: Protecting highly sensitive patient information in compliance with regulations like HIPAA and GDPR, which requires secure environments and sophisticated de-identification techniques. Platforms using a federated approach, which brings analytics to the data, help solve this by minimizing data movement.
Act Now: Connect Claims, EHR, Registries, HIE—or Keep Paying for Broken RWE
We’ve journeyed through healthcare data, from commercial and CMS claims data to EHRs, registries, and HIEs. Each source provides a unique lens, but the real power comes from connecting them. When we link a patient’s insurance claims with their clinical records, we move from fragmented snapshots to a complete understanding of health and disease. This is how we generate real-world evidence for breakthrough treatments and deliver on the promise of personalized medicine.
Overcoming challenges like data standardization, interoperability, and privacy is crucial. With the right approach federated architectures that keep data secure, common data models, and robust governance these obstacles are surmountable.
At Lifebit, this is exactly what our platform is designed to do. Our federated AI platform helps organizations provide health care data (e.g., commercial and Centers for Medicare & Medicaid Services (CMS)) claims data, commercial claims aggregators data, claims data linked to electronic health records (EHR) data, specialty EHR Data (e.g., oncology, pediatrics, geriatrics, hospital intensive care unit (ICU)), disease or product registry or registry network data, and Health Information Exchange (HIE) Data) securely and efficiently, without moving sensitive information from its source.
Our Trusted Research Environment (TRE), Trusted Data Lakehouse (TDL), and R.E.A.L. (Real-time Evidence & Analytics Layer) work together to harmonize data, power advanced AI analytics, and maintain federated governance. We create the trusted environment needed to collaborate, analyze, and find all while keeping patient data protected.
The era of truly personalized medicine is within reach. By connecting the dots between diverse data sources, we don’t just improve research we save lives and make healthcare work better for everyone.
Ready to see how integrated healthcare data can transform your research? Explore Lifebit’s federated biomedical data platform and find what’s possible when data works together.

