Why AI is the New Secret Sauce for Genomic Sequencing

Why AI in Genomics is Changing Healthcare Today
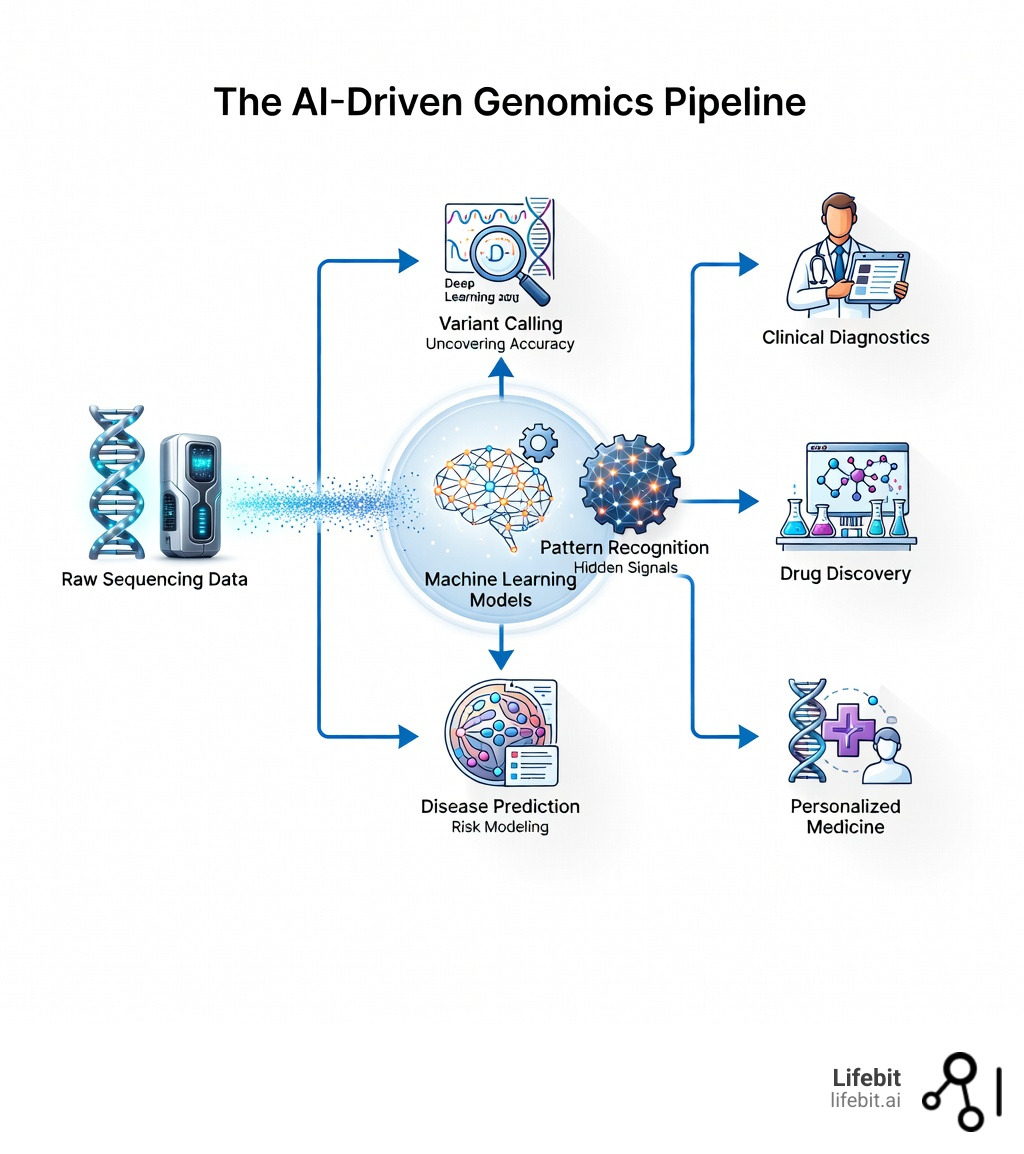
AI in genomics is revolutionizing how we analyze genetic data, diagnose diseases, and develop new treatments. Here’s what you need to know:
Key Applications of AI in Genomics:
- Variant Calling — AI tools like DeepVariant improve accuracy of identifying genetic mutations from DNA sequencing data
- Disease Prediction — Machine learning models analyze patterns in genomic datasets to predict disease risk and outcomes
- Drug Findy — AI accelerates identification of therapeutic targets by mining complex RNA biology data
- Protein Design — Tools like AlphaFold predict protein structures, enabling design of new drugs and biomaterials
- Rare Disease Diagnosis — AI reduces diagnostic delays by matching patient genetic profiles to known conditions
The challenge is massive. Modern genome sequencing generates billions of data points per patient. Traditional bioinformatics tools simply can’t keep pace with this data explosion. That’s where AI steps in—using machine learning and deep learning to find patterns humans would miss, process unstructured sequencing data at scale, and transform weeks of analysis into hours.
But speed isn’t the only benefit. AI is making genomics more accurate, more accessible, and more actionable. From predicting how a single DNA letter change affects disease risk to designing entirely new proteins for therapeutics, AI is bridging the gap between raw genetic data and real-world medical breakthroughs.
Yet challenges remain. Data quality, algorithmic bias, privacy concerns, and the “black box” nature of some AI models all demand attention. Biology is too complex for humans to understand alone—but it’s also too important to leave entirely to machines without transparency and oversight.
As Maria Chatzou Dunford, CEO and Co-founder of Lifebit, I’ve spent over 15 years working at the intersection of computational biology, AI, and genomics—from contributing to Nextflow, the workflow framework powering genomic analysis worldwide, to building federated platforms that enable secure, real-time AI in genomics across global research networks. In this guide, I’ll walk you through exactly how AI is changing genomic sequencing, where it’s making the biggest impact, and what problems we still need to clear.
Ai in genomics basics:
Decoding the Tech: How AI in Genomics Works
To understand why ai in genomics is such a game-changer, we first need to pull back the curtain on the technology itself. At its core, AI provides the “brainpower” to process the Big Data Challenges in Genomics. A single human genome contains roughly 3 billion base pairs. When we use Next Generation Sequencing, we aren’t just reading a book from start to finish; we are shredding millions of copies of that book and trying to piece them back together.

AI excels here because it doesn’t get tired and it doesn’t overlook “noise.” It treats Genomes as vast, multidimensional datasets where it can identify the subtle signals of disease. According to research published in An overview of artificial intelligence in the field of genomics, traditional bioinformatics often falls short when dealing with the sheer variety and velocity of this data. AI, however, thrives on it.
The Hierarchy of AI in Genomics
Not all AI is created equal. In our work, we typically categorize these tools into four main buckets, each serving a distinct purpose in the genomic pipeline:
- Supervised Learning: This is like teaching a student with an answer key. We feed the model labeled data—for example, Genomic sequences from 10,000 patients with a specific heart condition and 10,000 without it. The AI learns to recognize the “fingerprints” of the disease to predict it in new patients. This is the backbone of most diagnostic AI tools used today.
- Unsupervised Learning: Here, there is no answer key. The AI looks at raw Multi-Omics data and finds clusters or patterns on its own. This is incredibly powerful for finding new subtypes of cancer that we didn’t even know existed, or identifying population-specific genetic variations that were previously overlooked.
- Neural Networks (Deep Learning): These are models inspired by the human brain. They consist of layers of “neurons” that weigh data importance. Deep learning is particularly good at analyzing unstructured data, such as the raw images produced during DNA Sequencing Methods. Convolutional Neural Networks (CNNs) are often used for variant calling, while Recurrent Neural Networks (RNNs) and Transformers are increasingly used to understand the “language” of DNA sequences.
- Reinforcement Learning: This involves an agent learning through trial and error to achieve a goal. While less common in basic sequencing, it is becoming a staple in Synthetic Biology and protein folding, where the AI “experiments” with different molecular configurations to find the most stable or functional structure.
The Rise of Genomic Transformers
In the last two years, we have seen a shift toward “Genomic Foundation Models.” Much like Large Language Models (LLMs) like GPT-4 understand human language, these models are trained on billions of nucleotides to understand the “grammar” of the genome. Models like DNABERT or HyenaDNA can process long-range interactions in DNA—understanding how a mutation in one part of a chromosome might affect the expression of a gene millions of base pairs away. This is a level of complexity that traditional statistical models simply cannot capture.
From Raw Data to Variant Calling
The first major hurdle in Genomics is “variant calling”—identifying where a patient’s DNA differs from the reference genome. Traditional methods often struggle with high error rates, especially in complex regions of the genome like repetitive sequences or structural variants.
Tools like DeepVariant (developed by Google) and Clair3 (from HKU) have flipped the script. By treating genomic data as an image-processing task, DeepVariant uses deep neural networks to achieve significantly higher accuracy than older, hand-crafted algorithms. It converts the pile-up of DNA reads into a multi-channel image and uses a CNN to classify the genotype. In fact, many researchers now use a Nextflow DeepVariant Tutorial to implement these high-accuracy pipelines.
As noted in Gene Reports (2025), AI revolutionizes genomics by addressing these high error rates, turning “messy” raw data into a clean list of mutations that doctors can actually use. For those looking to scale, you can even deploy DeepVariant as Nextflow Pipeline CloudOS to handle thousands of samples simultaneously, ensuring that the computational bottleneck doesn’t slow down clinical care.
4 Ways AI is Revolutionizing Clinical Diagnostics and Drug Discovery
If variant calling is the foundation, then clinical application is the skyscraper we’re building on top of it. We are moving away from a “one-size-fits-all” medical model toward Precision Medicine, where treatments are tailored to the individual’s genetic makeup.
1. Accelerating Rare Disease Identification with AI in Genomics
For parents of children with rare genetic conditions, the “diagnostic odyssey” can last years, involving dozens of specialists and inconclusive tests. Statistics show that the pediatric genetic disease burden has a massive economic and emotional impact, often costing families hundreds of thousands of dollars before a diagnosis is reached. AI is shortening this timeline from years to mere hours.
One fascinating application is facial phenotyping. Tools like GestaltMatcher use AI to analyze facial features (phenotypes) that are often associated with rare Mendelian disorders. Many genetic syndromes have subtle physical markers that a human doctor might miss but an AI trained on thousands of images can identify instantly. By combining this visual data with Next-Generation Sequence Testing, clinicians can prioritize the most likely genetic culprits. A randomized trial showed that rapid genome sequencing, improved by AI, achieves world-class diagnostic performance in critically ill infants, often providing answers in less than 24 hours, allowing for immediate life-saving interventions.
2. Generative AI in Genomics: Designing the Future of Biology
Generative AI isn’t just for writing emails or creating art; it’s for “writing” biology. We are entering an era of Generative Genomics, where we use models to design entirely new biological components rather than just analyzing existing ones.
The Sanger Institute’s Generative and Synthetic Genomics programme is a prime example of this. They are building foundational models to engineer biology much like we engineer electronics. This includes:
- Protein Design: Using AlphaFold to predict how proteins fold, which is essential for creating new enzymes and biomaterials. AI can now design proteins that do not exist in nature, such as highly specific binders for viral proteins or enzymes that can break down plastic.
- RNA Therapeutics: Companies are using AI to mine RNA biology data, identifying targets for personalized therapies that were previously considered “undruggable.” AI helps predict the stability and translation efficiency of mRNA vaccines, a technology that was pivotal during the COVID-19 pandemic.
- CRISPR Optimization: AI helps design better “guide RNAs” for gene editing, predicting exactly where the molecular scissors will cut and—crucially—where they might accidentally cut elsewhere (off-target effects). This makes gene therapy significantly safer for human trials.
3. Revolutionizing Oncology and Early Cancer Detection
Cancer is fundamentally a disease of the genome, driven by the accumulation of mutations. AI is now being used to track “circulating tumor DNA” (ctDNA) in the blood—a process often called a liquid biopsy. This allows for non-invasive monitoring of cancer progression and response to treatment.
The NHS Galleri trial is currently testing a blood test that uses machine learning to detect over 50 types of cancer before symptoms even appear. By analyzing methylation patterns in the DNA (chemical tags that turn genes on or off), AI can pinpoint not just if cancer is present, but where in the body it originated with high specificity. This shift from reactive to proactive oncology could save millions of lives by catching cancer at Stage 1 or 2, when it is most treatable.
4. Pharmacogenomics: Personalizing the Prescription Pad
Every year, millions of people suffer from Adverse Drug Reactions (ADRs), which are often caused by genetic variations in how our bodies metabolize medication. AI is transforming Pharmacogenomics by predicting how a patient will respond to a specific drug based on their genetic profile.
For example, AI models can analyze the CYP450 gene family to determine if a patient is a “slow metabolizer” or an “ultra-rapid metabolizer” of common drugs like blood thinners or antidepressants. This allows doctors to prescribe the right dose the first time, avoiding the dangerous “trial and error” phase of medicine. Furthermore, AI is being used to optimize clinical trials by identifying the specific genetic subgroups most likely to benefit from a new drug, significantly reducing the time and cost of bringing new therapies to market. This is a direct answer to “Eroom’s Law”—the observation that drug discovery is becoming slower and more expensive over time despite technological advances.
Overcoming the “Black Box”: Challenges and Ethical Guardrails
As much as we love the “secret sauce” of AI, we have to be honest about the recipe. AI in genomics faces significant problems that we must address to ensure patient safety, scientific integrity, and public trust.
| Feature | Traditional Analysis | AI-driven Genomics |
|---|---|---|
| Speed | Weeks to Months | Hours to Days |
| Scalability | Limited by human experts | Virtually unlimited |
| Transparency | High (Rule-based) | Lower (“Black Box” models) |
| Accuracy | High for known variants | Superior for complex/novel variants |
| Data Requirement | Low | Very High |
The Problem of “Opaque” AI and Interpretability
One of the biggest criticisms of deep learning is that it can be a “black box.” A model might correctly identify a disease-causing mutation with 99% accuracy, but it can’t always explain why it made that choice. In a clinical setting, “because the computer said so” isn’t a valid medical justification. If a surgeon is going to perform a prophylactic mastectomy based on a genetic risk score, they need to understand the underlying biological mechanism.
This is why there is a massive push for Explainable AI (XAI). Research in An overview of artificial intelligence in the field of genomics suggests that rule-based models, such as those using fuzzy logic or attention maps, can provide more human-understandable explanations. For example, an attention map in a genomic transformer can show exactly which nucleotides the model focused on when predicting a splice site mutation, allowing a molecular biologist to verify the finding against known biochemical principles.
Solving the Data Privacy and Ethics Crisis
Genomic data is the most personal data there is. It doesn’t just identify you; it identifies your parents, your children, and your cousins. You can change your password or your credit card number, but you can’t change your DNA. This raises several ethical “red flags”:
- Data Privacy and Sovereignty: How do we share data for research without exposing patient identities? This is why we advocate for Federated Architecture in Genomics. Instead of moving sensitive data to a central AI server (which creates a massive security risk), we move the AI model to the data. The data stays securely behind the hospital’s or government’s firewall, and only the “learned insights” are shared.
- Algorithmic Bias and Health Equity: If an AI is trained mostly on genomes from people of European descent (who currently make up over 80% of genomic study participants), it may be less accurate for people from African, Asian, or Hispanic backgrounds. This can worsen existing health disparities. We must ensure our training sets are as diverse as the global population to prevent “genomic redlining.”
- Informed Consent in the Age of AI: As AI finds new links between genes and diseases, a patient might consent to a study on diabetes but inadvertently find out they have a high risk for Alzheimer’s. How do we manage these “incidental findings”?
- Regulatory Hurdles: Regulatory bodies like the FDA and EMA are struggling to keep up with the pace of AI innovation. Traditional medical device regulations are designed for static products, but AI models can change and improve over time. New frameworks for “Software as a Medical Device” (SaMD) are being developed to ensure that AI remains safe even as it evolves.
The Computational Cost of Innovation
Finally, we must address the “carbon footprint” of AI in genomics. Training a foundation model on millions of genomes requires massive computational power, often running on thousands of GPUs for weeks. This creates a barrier to entry for smaller research institutions and developing nations. At Lifebit, we focus on optimizing these workflows to be as efficient as possible, ensuring that the benefits of AI genomics are not restricted to the wealthiest nations.
The Future of Precision Medicine: Multi-Omics and Beyond
The next frontier isn’t just looking at DNA. It’s about Multi-Omics—integrating DNA (the blueprint), RNA (the message), proteins (the machinery), and metabolites (the output) into a single, comprehensive view of human health. AI is the only tool capable of synthesizing these disparate layers of biological information.
Spatial Genomics and the Cellular Neighborhood
One of the most exciting trends is Spatial Genomics. Traditional sequencing is like putting a tissue sample in a blender and analyzing the resulting “soup.” You know what’s in there, but you don’t know where it was. Spatial genomics allows us to see exactly where genes are being expressed within a tumor or a brain slice.
AI is crucial here for image registration and pattern recognition. By mapping these complex, three-dimensional cellular neighborhoods, AI helps us understand how cancer cells “hide” from the immune system or how neurons communicate in neurodegenerative diseases. This level of detail is paving the way for “next-gen” immunotherapies that can be targeted to specific regions of a tumor.
Digital Twins and the Virtual Patient
We are moving toward the concept of a Genomic Digital Twin. Imagine a virtual model of your biology that doctors can use to test treatments before they ever touch you. By combining your genomic data with real-time data from wearables (heart rate, sleep patterns, glucose levels), AI can create a predictive model of your health.
If you are diagnosed with hypertension, your doctor could run a simulation on your Digital Twin to see which of five different medications will work best with your specific genetic markers and lifestyle. This isn’t science fiction; pilot programs are already exploring how digital twins can improve outcomes for complex chronic diseases.
Scaling Global Health Initiatives
We are seeing a “Cambrian Explosion” of genomic data. Initiatives like Genomics England and the UK Biobank are providing the massive, longitudinal datasets needed to train the next generation of AI. These biobanks are the “oil fields” of the 21st century, providing the raw material for medical breakthroughs.
However, the challenge is no longer just generating the data—it’s analyzing it. One of the most exciting trends is the use of AI to bridge the gap in the clinical workforce. In regions with severe shortages of geneticists, AI-driven decision support systems are helping general practitioners interpret genetic reports, ensuring that a patient’s zip code doesn’t determine their access to precision medicine.
The Convergence of AI and Longevity
Finally, AI in genomics is being applied to the study of aging itself. By analyzing the “epigenetic clock”—changes in DNA methylation that occur as we age—AI can identify the biological drivers of senescence. Researchers are using these insights to identify compounds that could potentially slow down the aging process or prevent age-related diseases like osteoporosis and dementia before they begin. The goal is not just to extend life, but to extend “healthspan”—the number of years we live in good health.
Frequently Asked Questions about AI in Genomics
How does AI improve the accuracy of genome sequencing?
AI improves accuracy primarily through better variant calling. Traditional tools often struggle with “noise” in the sequencing data. AI models like DeepVariant are trained on “truth sets”—genomes that have been sequenced thousands of times to ensure 100% accuracy. The AI learns to recognize the visual patterns of real mutations versus sequencing errors, leading to much cleaner data.
Can AI reduce the time to diagnose rare genetic diseases?
Yes, dramatically. By using phenotype matching (like facial analysis) and automated Bioinformatics Platform workflows, AI can flag causative mutations in minutes. What used to be a years-long “diagnostic odyssey” can now, in some cases, be resolved while a patient is still in the hospital for their initial symptoms.
What are the primary ethical concerns of AI in genomics?
The top concerns are data privacy, bias, and consent. Because genomic data is uniquely identifying, protecting it from breaches is paramount. There is also a major risk that AI models trained on non-diverse data will produce biased results, leading to unequal healthcare outcomes for minority populations.
Conclusion: Scaling Secure Genomic Research
The marriage of AI and genomics is no longer a futuristic concept—it is the current engine of medical findy. However, to truly open up the “secret sauce,” we must move past the era of isolated data silos and “black box” algorithms.
At Lifebit, we believe the future of ai in genomics is federated and secure. Our platform provides a Genomics England Genomics Research Platform style of security, enabling researchers to access global, Multi-Omics data in real-time without ever compromising patient privacy.
By combining Federated Technology in Population Genomics with advanced AI analytics, we are helping biopharma, governments, and public health agencies turn billions of data points into life-saving insights. Whether it’s accelerating drug findy or providing answers for a child with a rare disease, we are committed to making the biorevolution safe, compliant, and accessible to all.
Ready to see how federated AI can transform your research?
Explore Lifebit’s Solutions for Commercial Pharma

