Federal Health 101

Stop the $500M Data Waste: How Federal Health Can Cut Costs and Speed Care
Federal health systems are how governments deliver, fund, and regulate healthcare. These national-level programs, agencies, and policies shape health services for millions of people.
Quick Overview: What Federal Health Means
- In Canada: The federal government sets national standards via the Canada Health Act, funds provinces, and provides direct services to groups like veterans and refugees through programs like the Interim Federal Health Program (IFHP).
- In the United States: Federal health includes agencies like the Department of Health & Human Services (HHS) and programs like the Federal Employees Health Benefits (FEHB) Program, which covers 8.3 million federal workers and their families.
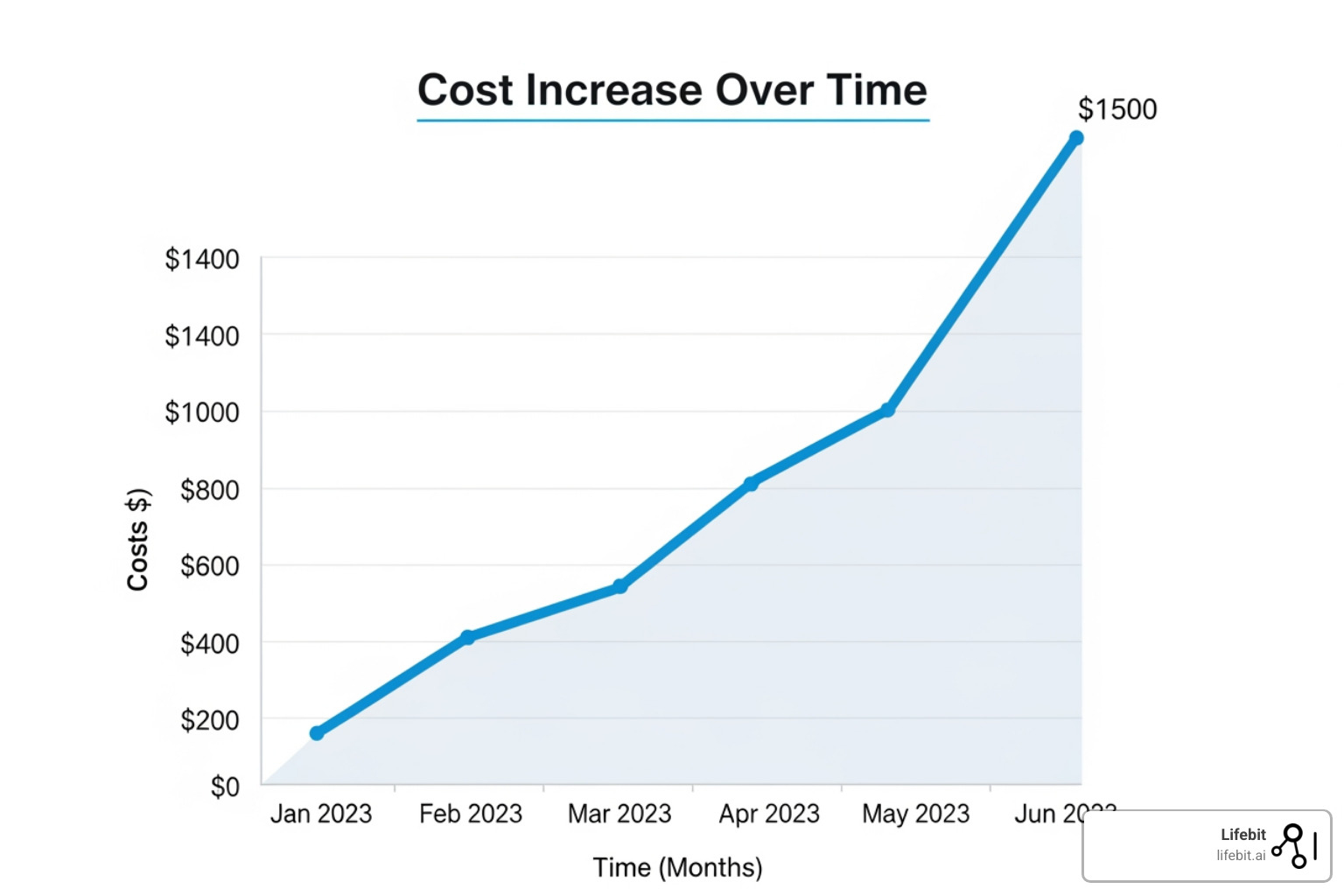
- Key Debate: Rising costs and data accessibility are major issues. Canada’s IFHP costs surged from $66 million to over $821 million in eight years.
Today, federal health is about data, infrastructure, and equity: who gets care, who pays, and how fast governments can respond to crises.
In Canada, the debate centers on the IFHP, which provides temporary health coverage to refugees. Critics point to a 400% user increase and supplemental benefits that many citizens don’t receive.
In the U.S., the federal government runs the world’s largest employer-sponsored health plan (FEHB), but data blocking—where providers restrict access to patient information—is such a problem that HHS is now enforcing penalties to improve data flow.
Both nations struggle to turn health data into actionable insights. Legacy systems and fragmented databases slow everything down. For federal agencies and pharma companies, the question isn’t just what data exists—it’s how to access and analyze it securely and quickly while complying with regulations like HIPAA, FedRAMP, or GDPR.
I’m Maria Chatzou Dunford, CEO of Lifebit. We help public and private sector organizations open up insights from sensitive federal health data using secure, federated analytics. Our platform enables compliant, AI-driven research and real-time evidence generation without moving data.

Quick federal health terms:
Canada’s IFHP Hit $821M: What to Fix Now to Protect Care and Taxpayers
Canada’s federal health system is a partnership: the federal government funds and sets standards, while provinces deliver care. At the center is Health Canada, but one of its programs—the Interim Federal Health Program (IFHP)—has become a lightning rod for controversy.
The numbers are stark: the IFHP’s cost exploded from $66 million in 2016 to over $821 million by 2024—a twelve-fold increase in eight years that has taxpayers demanding answers.
The Core Mission of Health Canada and the Canada Health Act
Health Canada acts as the nation’s health guardian. It regulates drugs and food, sets national care standards for provinces to follow, provides public health information, and invests in research to prevent disease. The foundation of this system is the Canada Health Act, which establishes the five criteria provinces and territories must meet to receive full federal funding via the Canada Health Transfer (CHT):
- Public Administration: Provincial health insurance plans must be administered on a non-profit basis by a public authority.
- Comprehensiveness: The plan must insure all medically necessary services provided by hospitals and physicians.
- Universality: All insured residents must be entitled to the same level of health care.
- Portability: Residents moving from one province to another must continue to be covered by their home province during a minimum waiting period.
- Accessibility: Residents must have reasonable access to health care facilities and services without financial or other barriers.
Health Canada does not run most hospitals or clinics directly (except for specific groups like Indigenous peoples on reserves). Instead, it shapes the system through funding and legislation, a role that often leads to federal-provincial tensions over the adequacy of the CHT. You can explore more about this structure at About Canada’s health care system.
Understanding the IFHP: A Lifeline for Newcomers
The IFHP provides temporary health coverage for specific groups of newcomers who lack provincial or private insurance, including resettled refugees, protected persons, asylum claimants, and certain victims of human trafficking. Administered by Medavie Blue Cross, the program has a complex history; it was significantly scaled back in 2012 by the previous government before being fully restored in 2016, a decision that set the stage for today’s cost pressures.
The program offers two tiers of coverage:
Basic coverage mirrors provincial plans, covering essential hospital services, doctor visits, and emergency care. Supplemental coverage, however, is the primary source of controversy. It includes benefits like dental care, vision care, home care, and physiotherapy—services many Canadian citizens must pay for out-of-pocket or through expensive private insurance. You can see the full breakdown at IFHP benefit grids.
That disparity, where newcomers may temporarily receive more comprehensive coverage than some long-term residents, is fueling much of the current debate.
Skyrocketing Costs and Public Outcry: Why Canadians are Demanding Answers
The number of people served by the IFHP surged from 84,967 in 2016-17 to an estimated 426,750 by 2024-25—a 400% increase. This dramatic rise is linked to global instability and a significant increase in asylum claims in Canada. Of the projected $821 million spent in 2024, over $456 million is allocated to supplementary coverage.
This spending is occurring as the broader Canadian healthcare system faces immense strain. With 6.5 million Canadians lacking a family doctor and provincial health systems struggling with long wait times, the perception that newcomers receive more comprehensive benefits creates significant public friction.
The controversy deepens over several key points:
- Eligibility for Rejected Claimants: Even rejected asylum claimants remain eligible for IFHP benefits until they are removed from Canada, a process that can take months or years. Critics argue this creates a perverse incentive and exploits the system.
- Provider Billing Practices: There are concerns that some healthcare providers charge premium rates for IFHP services, as the program may lack the stringent fee limits found in provincial plans, further inflating costs.
- Public Health vs. Fiscal Prudence: Supporters and advocacy groups defend the program as a compassionate and necessary public health measure, arguing that denying care to vulnerable populations would lead to worse health outcomes and higher long-term costs from emergency room visits. Fiscal conservatives, however, point to the unsustainable growth rate and demand reforms to protect taxpayers.
The IFHP debate highlights a core tension in federal health policy: balancing humanitarian care with fiscal responsibility. As costs climb, Canada must find a path forward that honors both its values and its obligations to taxpayers. You can read more about the detailed cost breakdown in this parliamentary response on IFHP costs.
FEHB Covers 8.3M: How to Pick the Right Plan and Save Now
In contrast to Canada’s universal model, the U.S. federal health system is a complex patchwork where the government acts as a regulator, funder, and direct insurer for specific populations. The U.S. Department of Health & Human Services (HHS) sets national policy, while the Office of Personnel Management (OPM) manages the world’s largest employer-sponsored health program.
While most non-elderly Americans get private insurance through their jobs, the federal government directly provides or funds coverage for millions through programs like the FEHB for federal employees, the Defense Health Agency (DHA) for military personnel and their families, and the Department of Veterans Affairs (VA) for veterans. This vast federal health infrastructure touches tens of millions of lives, operating within the nation’s market-based healthcare approach.

The U.S. Department of Health & Human Services (HHS)
HHS is the guardian of American public health, with a mission to enhance the health and well-being of all Americans. It is a massive umbrella organization with a budget in the trillions, overseeing a wide array of agencies that are household names:
- Centers for Disease Control and Prevention (CDC): The nation’s public health agency, responsible for disease surveillance, prevention, and response to health emergencies.
- National Institutes of Health (NIH): The world’s foremost medical research organization, funding thousands of research projects to uncover new knowledge that leads to better health for everyone.
- Food and Drug Administration (FDA): Protects public health by ensuring the safety, efficacy, and security of human and veterinary drugs, biological products, medical devices, our nation’s food supply, cosmetics, and products that emit radiation.
- Centers for Medicare & Medicaid Services (CMS): Administers Medicare, the federal health insurance program for people 65 or older and certain younger people with disabilities, and Medicaid, a joint federal and state program that helps with medical costs for some people with limited income and resources. Together, these programs cover over 140 million Americans.
You can explore the full scope of their work at the Department of Health & Human Services official website.
The Federal Employees Health Benefits (FEHB) Program
The Federal Employees Health Benefits (FEHB) Program is a prime example of U.S. federal health in action. As the largest employer-sponsored health program globally, it covers 8.3 million federal employees, retirees, and their families. Managed by the Office of Personnel Management (OPM), it is a cornerstone of federal employment benefits.
The FEHB Program is defined by choice. During the annual “Open Season,” typically from mid-November to mid-December, federal employees can enroll, change plans, or adjust their coverage. With roughly 180 different health plans available nationwide, the options can be overwhelming but allow for highly personalized coverage. Plan types include:
- Consumer-Driven and High Deductible Health Plans (HDHPs): These plans feature lower premiums but higher deductibles. They are often paired with a Health Savings Account (HSA) or Health Reimbursement Arrangement (HRA), allowing members to use pre-tax dollars for medical expenses. A young, healthy employee might choose this option to save on premiums and build a tax-advantaged health fund.
- Fee-for-Service (FFS) plans with Preferred Provider Organizations (PPOs): These plans offer the most flexibility, allowing members to see any doctor or specialist without a referral, both in- and out-of-network (though out-of-network care is more expensive). A family with complex medical needs might prefer a PPO for its broad access to specialists.
- Health Maintenance Organizations (HMOs): These plans typically have lower out-of-pocket costs but require members to use doctors, hospitals, and specialists within their network and to get a referral from a Primary Care Physician (PCP) for specialized care.
The federal government subsidizes a significant portion of the premium costs, typically covering about 72% of the total premium, with the employee paying the rest. Unlike Medicare and Medicaid, FEHB members can also participate in pharmacy-sponsored incentive and co-pay assistance programs, giving them more options to manage prescription costs. OPM provides extensive comparison tools to help members choose the right plan based on their expected health needs and financial situation. For more detailed information, visit More on FEHB plans to explore your options.
End 200-Day Delays: Use TEFCA and Anti-Blocking Rules to Cut Costs Fast
While Canada and the U.S. have different federal health structures, both face a common, paralyzing challenge: their health data is trapped in disconnected silos. This isn’t just a technical headache; it has severe real-world consequences, leading to delayed care, wasted resources, and missed opportunities for life-saving research.
For example, the Social Security Administration (SSA) takes over 200 days and spends $500 million annually just to collect medical evidence for disability claims. This staggering delay, caused by data silos and institutional friction like data blocking, wastes taxpayer money and leaves vulnerable Americans waiting for critical support.
The goal is to transform these fragmented systems into secure, interconnected networks that deliver timely insights. This requires robust security and compliance frameworks, like FedRAMP, which sets the rigorous standard for cloud services handling sensitive federal data.
The Root Causes of Data Silos
Data fragmentation stems from more than just outdated technology. Key barriers include:
- Proprietary Systems: Electronic Health Record (EHR) vendors historically built closed systems, making it difficult to export or share data with competing platforms.
- Lack of Standardization: While standards like FHIR (Fast Healthcare Interoperability Resources) are emerging, data is often stored in inconsistent formats, making it difficult to aggregate and analyze.
- Misaligned Incentives: Healthcare providers have not always been incentivized to share data, sometimes viewing it as a competitive asset.
- Complex Privacy Regulations: While essential, regulations like HIPAA can be interpreted conservatively, leading organizations to err on the side of caution and restrict data sharing even when it is legally permissible and clinically beneficial.
Breaking Down Silos: TEFCA and Information Blocking Rules
The U.S. Department of Health & Human Services is tackling this problem head-on. A key part of its strategy is the 21st Century Cures Act, which established two powerful mechanisms: the Information Blocking Rule and TEFCA.
The Information Blocking Rule makes it illegal for healthcare providers, IT developers, and health information exchanges to knowingly and unreasonably interfere with the access, exchange, or use of electronic health information. HHS is now enforcing this with significant enforcement actions and penalties. For certified health IT developers, penalties can reach up to $1 million per violation. This rule is a powerful stick designed to change behavior and foster a culture of data sharing.
Complementing this is the Trusted Exchange Framework and Common Agreement (TEFCA). TEFCA is not a new network itself, but a ‘network of networks’ designed to create a single, secure on-ramp to nationwide health information exchange. It works through Qualified Health Information Networks (QHINs), which are large, established networks that agree to a common set of technical and legal rules for data sharing. This common framework, overseen by The Sequoia Project as the Recognized Coordinating Entity (RCE), allows a provider connected to one QHIN to securely and easily request and receive patient records from a provider connected to any other QHIN. This could dramatically cut the 200-day disability claim processing time for the SSA and improve care coordination everywhere.
The Future of Federal Health: AI and Federated Analytics
Breaking down silos is the first step; applying AI and advanced analytics is the next. The ability to analyze vast, diverse datasets opens up transformative possibilities for federal health programs.
-
Improving Medicare Risk Adjustment: In Medicare Advantage, insurers are paid based on patient sickness levels, calculated using Hierarchical Condition Categories (HCCs). This process often relies on incomplete claims data. AI, specifically Natural Language Processing (NLP), can analyze unstructured data like clinical notes and discharge summaries to find documented but un-coded diagnoses. This leads to more accurate risk scores, ensuring plans are compensated fairly for caring for sicker patients and enabling earlier identification of high-risk individuals for care management programs.
-
Generating Real-World Evidence (RWE): Regulatory bodies like the FDA increasingly use RWE to monitor post-market safety and understand how treatments perform in the real world. However, this data is often spread across multiple health systems. Federated analytics allows researchers to run a single query across these distributed datasets. For example, a safety signal for a new drug could be investigated by analyzing data from the VA, a large academic medical center, and a network of community hospitals simultaneously, without any of them having to move or pool their sensitive patient data. The analysis is brought to the data, and only aggregated, anonymous results are returned.
The challenge is analyzing this sensitive data without violating privacy rules like HIPAA or GDPR. This is where federated analytics provides a breakthrough. Instead of centralizing data in a vulnerable repository, the analytical model is sent to each data location. Queries run locally behind the data owner’s firewall, and only the aggregated insights—which contain no patient-level information—are returned. At Lifebit, our platform is built on this federated principle, enabling compliant, AI-driven research for biopharma, government, and public health organizations.
Stop Guessing: IFHP vs. Provinces and FEHB Eligibility, Explained
What is the main difference between Canadian and US federal health roles?
In Canada, the federal government primarily sets national standards and funds the provinces, which deliver most care. It only provides direct care to specific groups (e.g., veterans, Indigenous peoples). In the U.S., the federal health system acts as a major insurer and direct provider for large populations, such as federal employees (FEHB), seniors, and veterans, in addition to its regulatory role.
Is Canada’s IFHP more generous than provincial plans?
Yes, in some ways. While basic IFHP coverage mirrors provincial plans, its supplemental coverage for services like dental, vision, and physiotherapy often exceeds what many citizens receive without private insurance. With over $456 million spent on these benefits in 2024/2025, this disparity fuels public debate, especially when many Canadians lack access to basic care.
Who is eligible for the FEHB program in the US?
Eligibility is broad, covering most federal employees, retirees, and their eligible family members (spouses and children). Survivors of federal workers can also maintain coverage. The program’s continuity from active employment into retirement is a key benefit. With around 180 plan options, it offers significant flexibility. For more details on plan options and enrollment, you can visit More on FEHB plans.
Act Now or Pay More: Federated Analytics Cuts Federal Health Cost and Risk
The challenges in federal health—from Canada’s soaring IFHP costs to U.S. data blocking—are not just policy debates. They affect federal employees, refugees, veterans, and taxpayers.
The common thread tying these issues together is data—specifically, the inability to access and analyze it securely and efficiently. The delays and costs are staggering, with agencies like the SSA spending over $500 million annually just to collect medical evidence for claims.
The future of federal health is about spending smarter by breaking down data silos securely. It’s about using AI to spot patterns that human eyes might miss, like undiagnosed conditions in clinical notes that could improve Medicare risk adjustment or safety signals that help the FDA protect public health.
This is where federated analytics comes in. Instead of moving sensitive data, the analysis happens where the data lives. Researchers get insights, patient privacy is protected, and regulatory requirements are met.
This is the problem Lifebit solves. Our federated platform, including our Trusted Research Environment (TRE) and R.E.A.L. (Real-time Evidence & Analytics Layer), enables secure, compliant research across sensitive datasets without moving them. We help government agencies and biopharma turn data from a compliance burden into a strategic asset.
The debate between cost and care will continue, but it can be more informed and evidence-based, ultimately better serving the people these federal health programs were designed to help.
Ready to see how your organization can open up insights from sensitive health data without compromising security or compliance? Explore how to unlock insights from sensitive health data.

